Hospital Medicine: Hospital Medicine Quality Improvement
Category: Abstract Submission
Hospital Medicine: Systems/Population Health
137 - A quality improvement project to improve hospital-to-home transitions of care using discharge televisits
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 137
Publication Number: 137.416
Publication Number: 137.416
Kulsajan S. Bhatia, State University of New York Downstate Medical Center College of Medicine, Brooklyn, NY, United States; Khawar Nawaz, SUNY Downstate medical center, Brookyn, NY, United States; Lee M. Waldman, SUNY Downstate Medical Center, Brooklyn, NY, United States; Saema Khandakar, SUNY Downstate College of Medicine, Albertson, NY, United States; Hal Sitt, NYC Health+Hospitals/Kings County, Brooklyn, NY, United States; Ninad Desai, State University of New York Downstate Medical Center College of Medicine, Brooklyn, NY, United States; Risa Bochner, New York City Health and Hospitals Kings County, Brooklyn, NY, United States

Kulsajan S. Bhatia, MBBS
Resident
SUNY Downstate Health Sciences University
Brooklyn, New York, United States
Presenting Author(s)
Background: One in five families reports a major problem with the transition from hospital to home. Virtual telephone visits (televisits), which are gaining popularity during the COVID-19 pandemic to improve healthcare access, cost, experience, and effectiveness, can potentially enhance the safety of hospital-to-home transitions.
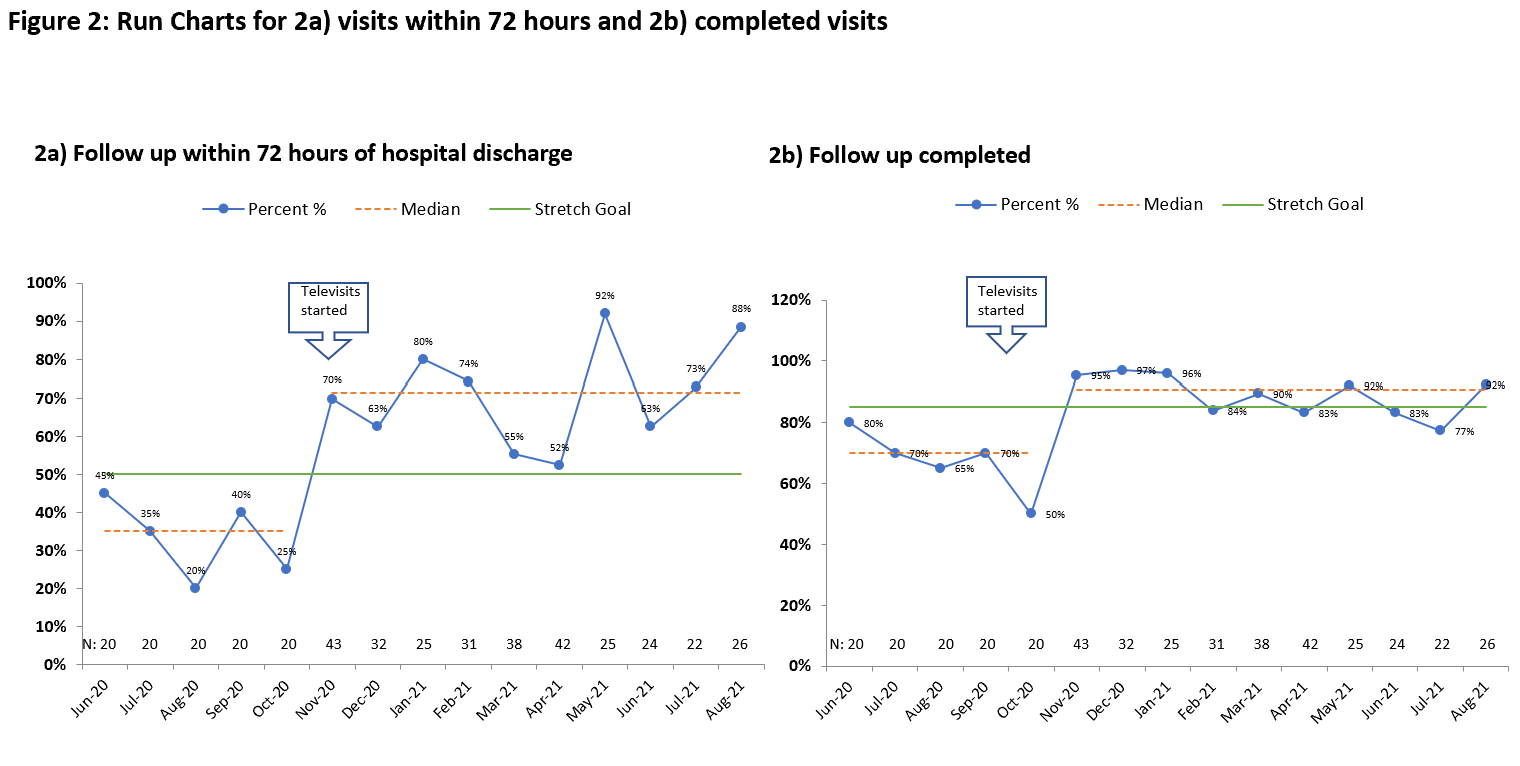
Objective: Starting October 2020, conduct hospital discharge televisits to improve follow up within 72 hours of hospital discharge from 35% to 50% and completed follow up from 70% to 85% by August 2021.
Design/Methods: A team of pediatric residents, hospitalists, outpatient pediatricians, and quality improvement specialists convened starting in July 2020 and used the Model for Improvement and key driver diagram to guide improvement work (Figure 1). Baseline data were collected from June 2020-October 2020. From October 29, 2020, to August 31, 2021, the team conducted the following Plan-Do-Study-Act cycles: Built a televisit template in the electronic medical record with 10 slots per week, trained residents on televisit workflow, created a previsit checklist, and provided feedback to and elicited feedback from providers conducting the televisits. The outcome measures were the proportion of patients with televisits who had follow-up within 72 hours of discharge and with completed follow-up. The process measure was the proportion of televisit appointment slots filled. The balancing measure was seven-day readmissions. Topics addressed during the tele-visits were also recorded and categorized. Data was tracked continuously and displayed on run charts.
Results: There were 308 televisits scheduled and 275 (89.3%) completed during the study period. Follow-up within 72 hours increased to 71.2% (Figure 2a) and completed follow-up to 90.7% (Figure 2b). Topics addressed included results of diagnostic testing, medication issues, scheduling subspecialty appointments, and symptom-related concerns (Figure 3). Of the 434 available televisit slots, 308 (71.0%) were scheduled. There were 4 (1.5%) readmissions within 7-days of discharge for patients with completed televisits.Conclusion(s): Televisits are an innovative way to increase the timeliness and completeness of hospital discharge follow-up. Since they are conducted by the inpatient physician team who discharged the patient, they provide superior continuity of care compared to traditional follow-up and allow for immediate intervention as needed. They allow discussion of clinically relevant topics like results of diagnostic testing. In the current COVID-19 pandemic, telemedicine has been critical for safe and effective continuity of care post-discharge.
Kulsajan Bhatia CVKulsajan Singh Bhatia cv.pdf
Run charts for visits within 72 hrs and completed discharge televisits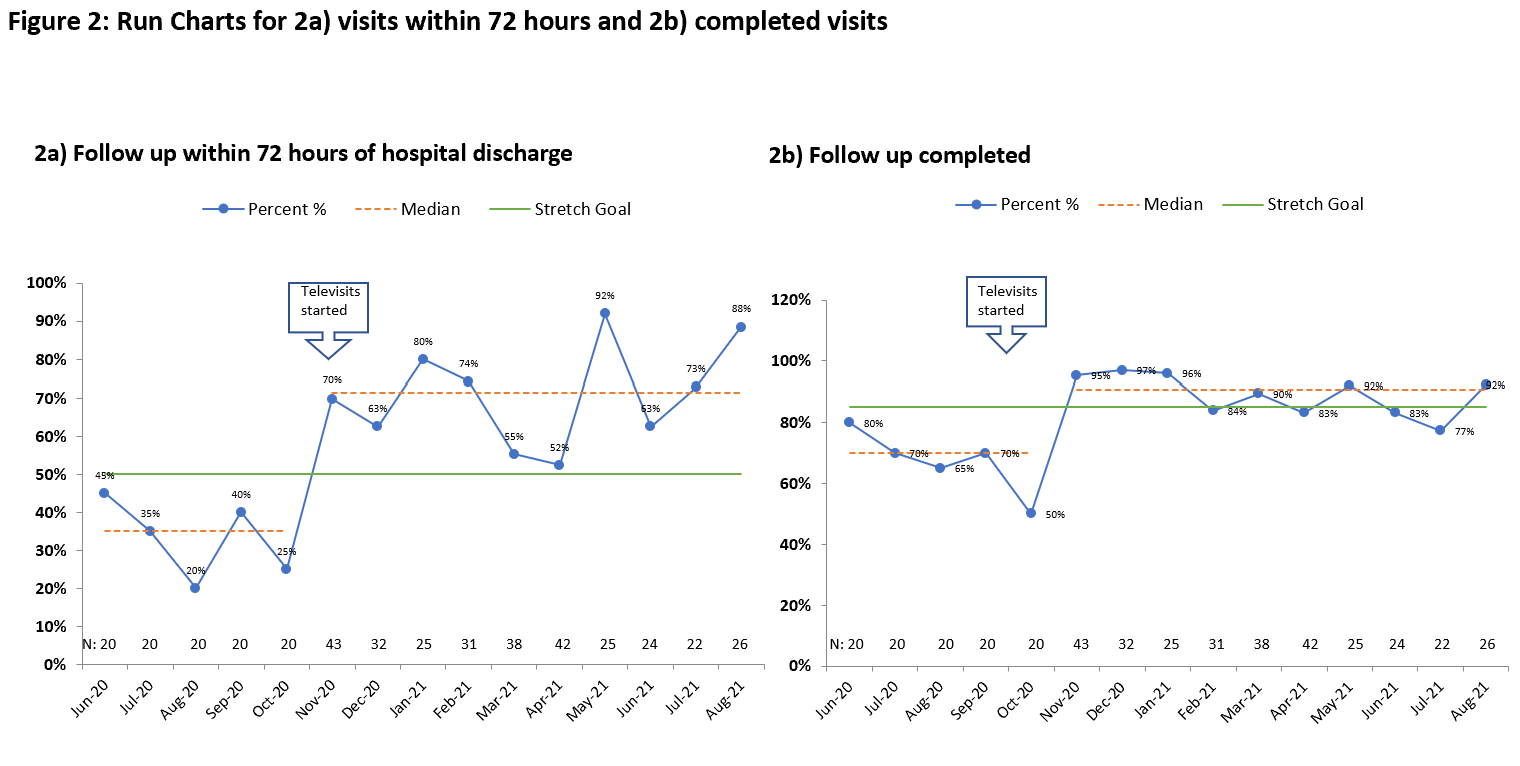
Objective: Starting October 2020, conduct hospital discharge televisits to improve follow up within 72 hours of hospital discharge from 35% to 50% and completed follow up from 70% to 85% by August 2021.
Design/Methods: A team of pediatric residents, hospitalists, outpatient pediatricians, and quality improvement specialists convened starting in July 2020 and used the Model for Improvement and key driver diagram to guide improvement work (Figure 1). Baseline data were collected from June 2020-October 2020. From October 29, 2020, to August 31, 2021, the team conducted the following Plan-Do-Study-Act cycles: Built a televisit template in the electronic medical record with 10 slots per week, trained residents on televisit workflow, created a previsit checklist, and provided feedback to and elicited feedback from providers conducting the televisits. The outcome measures were the proportion of patients with televisits who had follow-up within 72 hours of discharge and with completed follow-up. The process measure was the proportion of televisit appointment slots filled. The balancing measure was seven-day readmissions. Topics addressed during the tele-visits were also recorded and categorized. Data was tracked continuously and displayed on run charts.
Results: There were 308 televisits scheduled and 275 (89.3%) completed during the study period. Follow-up within 72 hours increased to 71.2% (Figure 2a) and completed follow-up to 90.7% (Figure 2b). Topics addressed included results of diagnostic testing, medication issues, scheduling subspecialty appointments, and symptom-related concerns (Figure 3). Of the 434 available televisit slots, 308 (71.0%) were scheduled. There were 4 (1.5%) readmissions within 7-days of discharge for patients with completed televisits.Conclusion(s): Televisits are an innovative way to increase the timeliness and completeness of hospital discharge follow-up. Since they are conducted by the inpatient physician team who discharged the patient, they provide superior continuity of care compared to traditional follow-up and allow for immediate intervention as needed. They allow discussion of clinically relevant topics like results of diagnostic testing. In the current COVID-19 pandemic, telemedicine has been critical for safe and effective continuity of care post-discharge.
Kulsajan Bhatia CVKulsajan Singh Bhatia cv.pdf
Run charts for visits within 72 hrs and completed discharge televisits