Neonatal Pulmonology
Category: Abstract Submission
Neonatal Pulmonology V: Preclinical studies and Clinical Care Issues
473 - Association Between Intraventricular Hemorrhage and Respiratory Severity Scores in Extremely Low Birth Weight Infants on Mechanical Ventilation.
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 473
Publication Number: 473.433
Publication Number: 473.433
Monika Piatek, University of Kentucky College of Medicine, Grosse Pointe Shores, MI, United States; Elie G. Abu Jawdeh, University of Kentucky College of Medicine, Lexington, KY, United States; Peter J. Giannone, University of Kentucky College of Medicine, Lexington, KY, United States; Brandon Miller, University of Texas, Houston, TX, United States; Aric Schadler, University of Kentucky College of Medicine, Lexington, KY, United States; Mina Hanna, University of Kentucky College of Medicine, Lexington, KY, United States
- MP
Monika Piatek, MD
Fellow
University of Kentucky College of Medicine
Grosse Pointe Shores, Michigan, United States
Presenting Author(s)
Background: Pathogenesis of intraventricular hemorrhage (IVH) in preterm neonates is multifactorial. While neonatal respiratory pathology including mechanical ventilation and pneumothorax are known risk factors for IVH, less is known about how IVH affects respiratory function.
Objective: The study aimed to define the relationship between IVH and the development of progressive lung disease in extremely low birth weight (ELBW) infants placed on high frequency jet ventilators (HFJV). We hypothesized that infants with severe IVH had higher respiratory severity scores (RSSs) than infants with mild/none IVH within the first 7 days of life.
Design/Methods: This was a single-center retrospective cohort study. We enrolled preterm infants with a gestational age of less than 30 weeks of gestation, and birth weight of less than 1000 grams who were admitted to the NICU at Kentucky Children's Hospital between 2018-2021. We extracted demographic data for both neonates and mothers from the electronic medical record. HFJV daily settings in the first week of life were collected. We used RSS, the product of mean airway pressure (MAP) and fraction of inspired oxygen (FiO2) to estimate the severity of neonatal lung disease.
Results: 135 infants met the inclusion criteria. 72% of neonates had none/low grade IVH (Grade I or Grade II), while 28% had severe IVH (Grade III or Grade IV). Infants who had severe IVH had significantly lower gestational ages [(24.3 0 ± 1.0 vs. 26.0 ± 1.8); p < 0.001], birth weights [(667 ± 138 vs. 732 ± 147); p=0.021] and were delivered vaginally (63% vs. 82%; p=0.018). Neonates with severe IVH were more likely to be placed on single (21% vs. 6%; p=0.011) or multiple pressors (37% vs. 12%; p=0.001), and receive blood transfusion (p < 0.001) within the first 7 days of life. Postnatal RSSs were correlated with IVH severity. We found a trend of worsening RSSs within the first week of life in the group of infants with severe IVH. The median RSS (IQR) in the severe IVH group and none/low grade IVH group was 3.6 (2.7-4.1) and 2.3 (2.0-3.1), respectively (p < 0.001).Conclusion(s): This study is first to show that severe IVH is associated with higher RSSs predicting early lung injury in ELBW infants placed on a mechanical ventilator within the first 7 days of life. The injury of the lungs is explained by the increasing trend of RSSs within the first week of life. We speculate that after severe IVH, inflammatory markers are released into the systemic circulation, affecting extracerebral organs particularly leading to worsening lung injury. A prospective study is needed to better assess the relationship between IVH and RSSs.
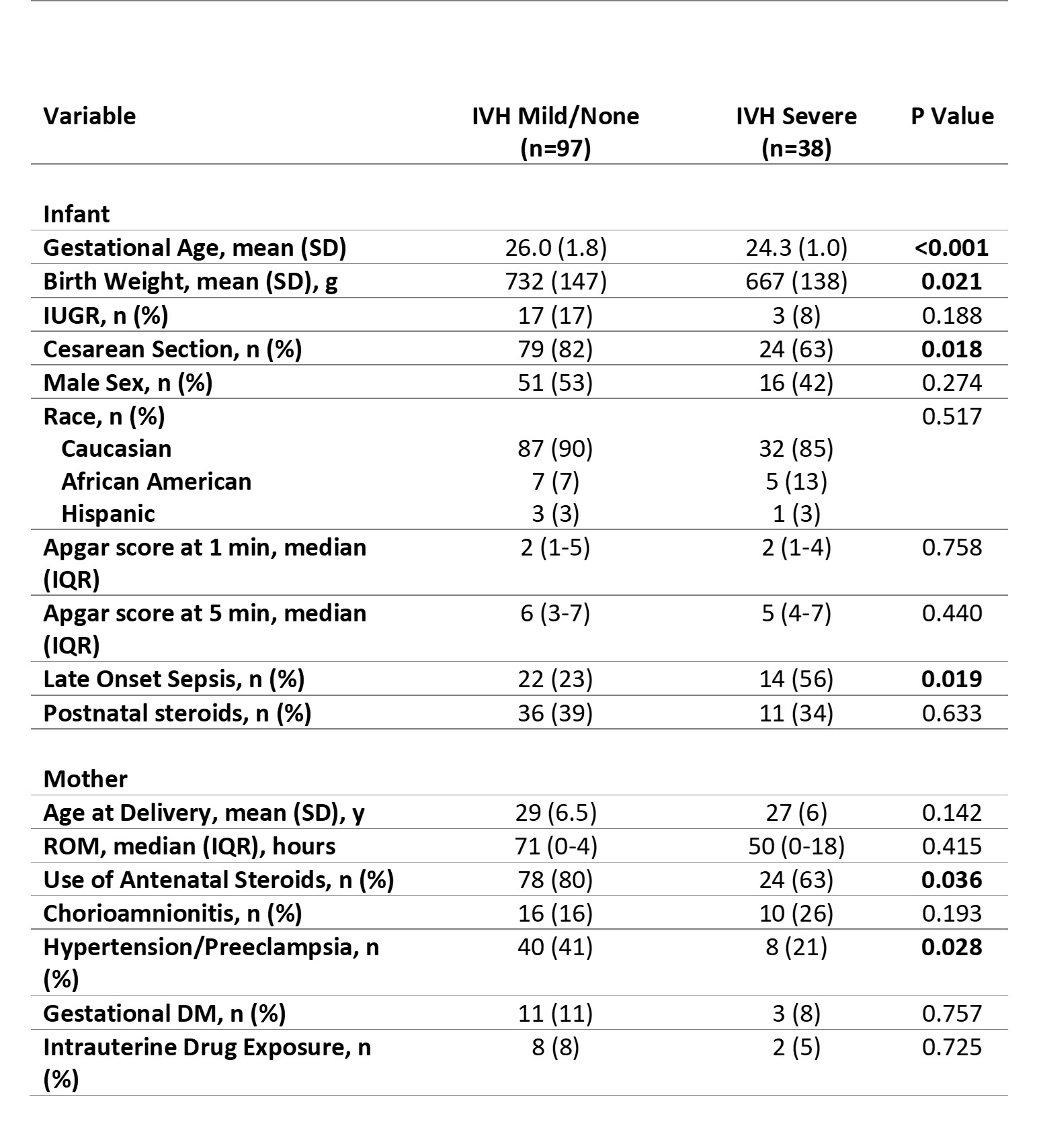
Demographic Data.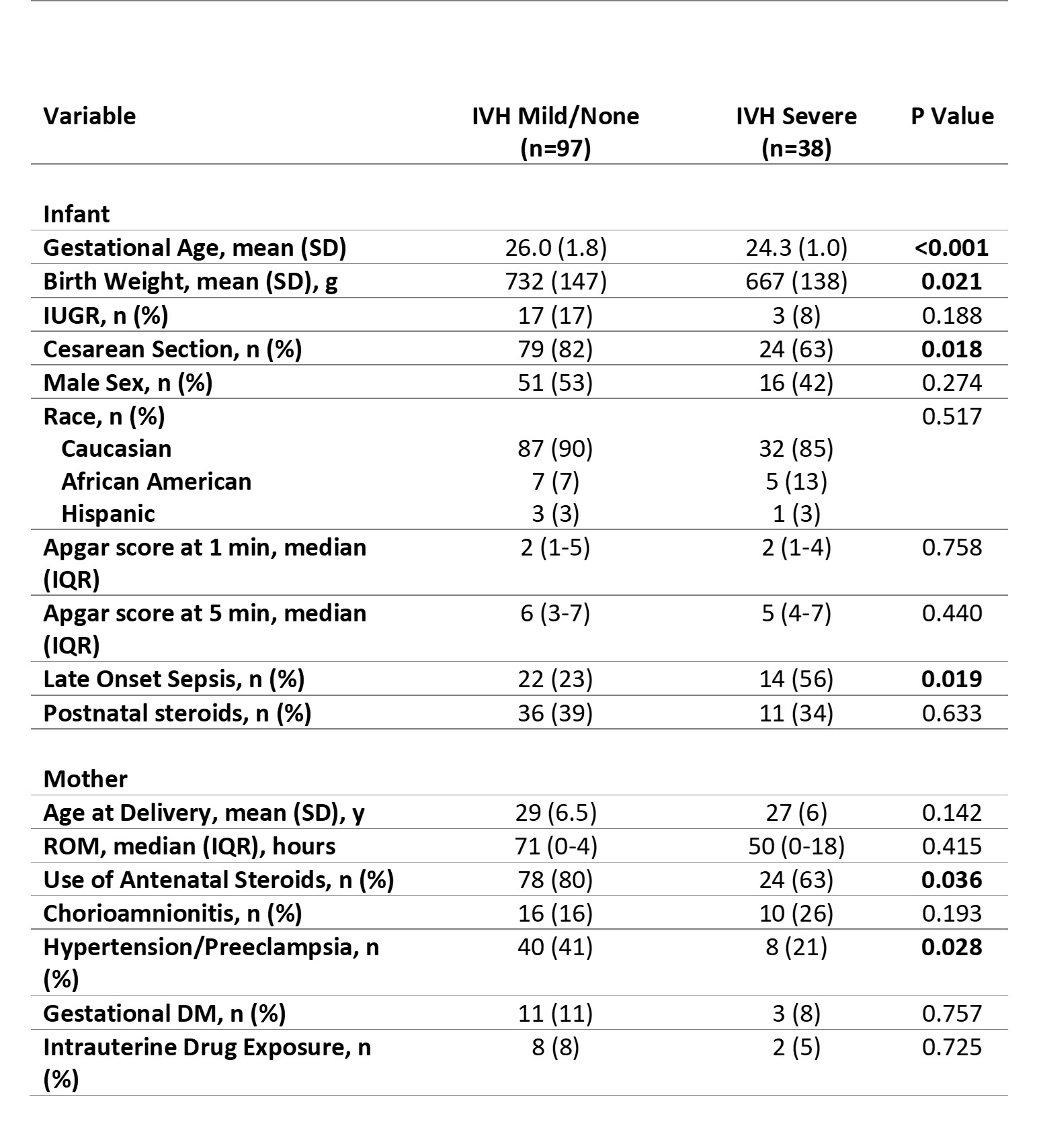
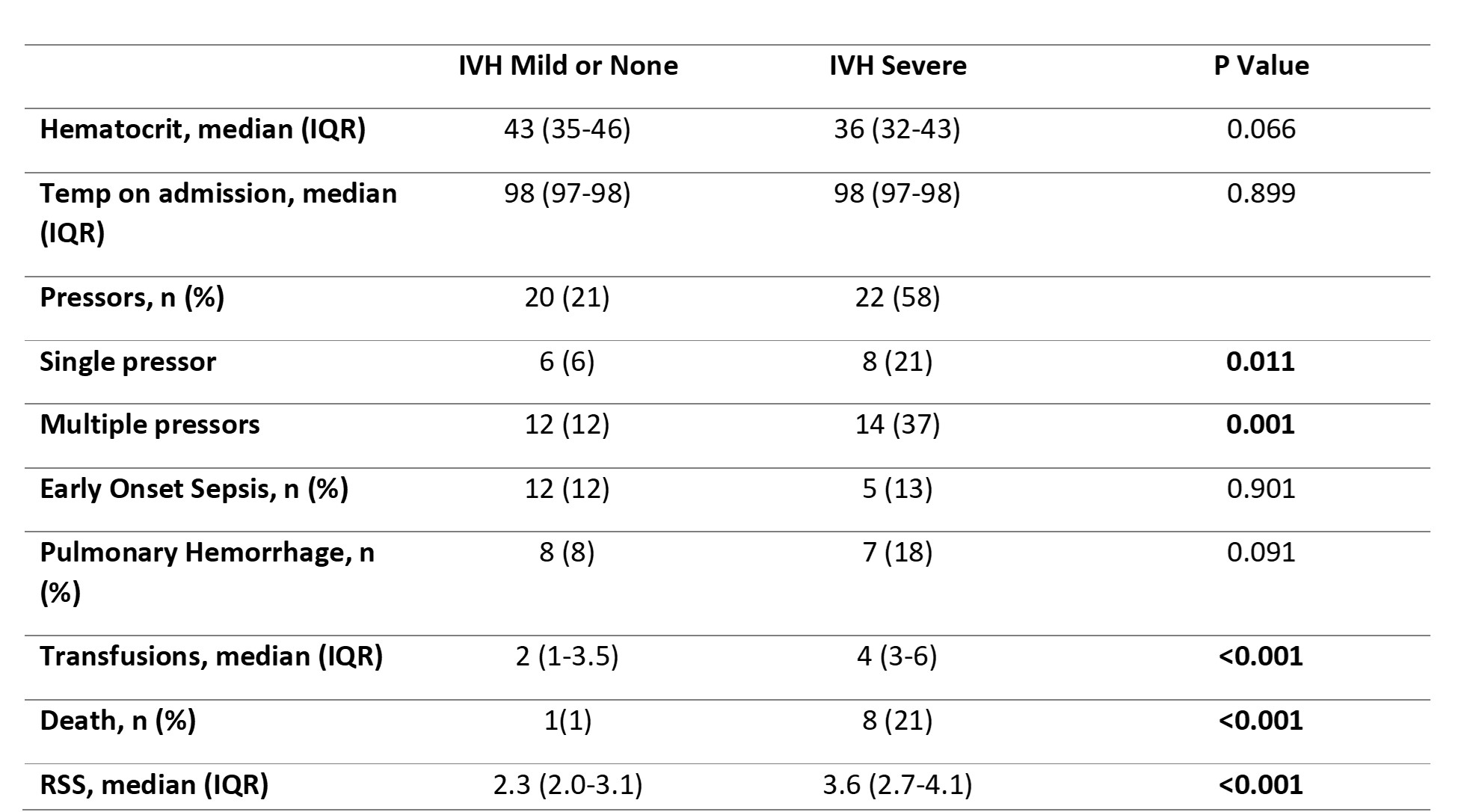
Clinical Variables in the First Week of Life.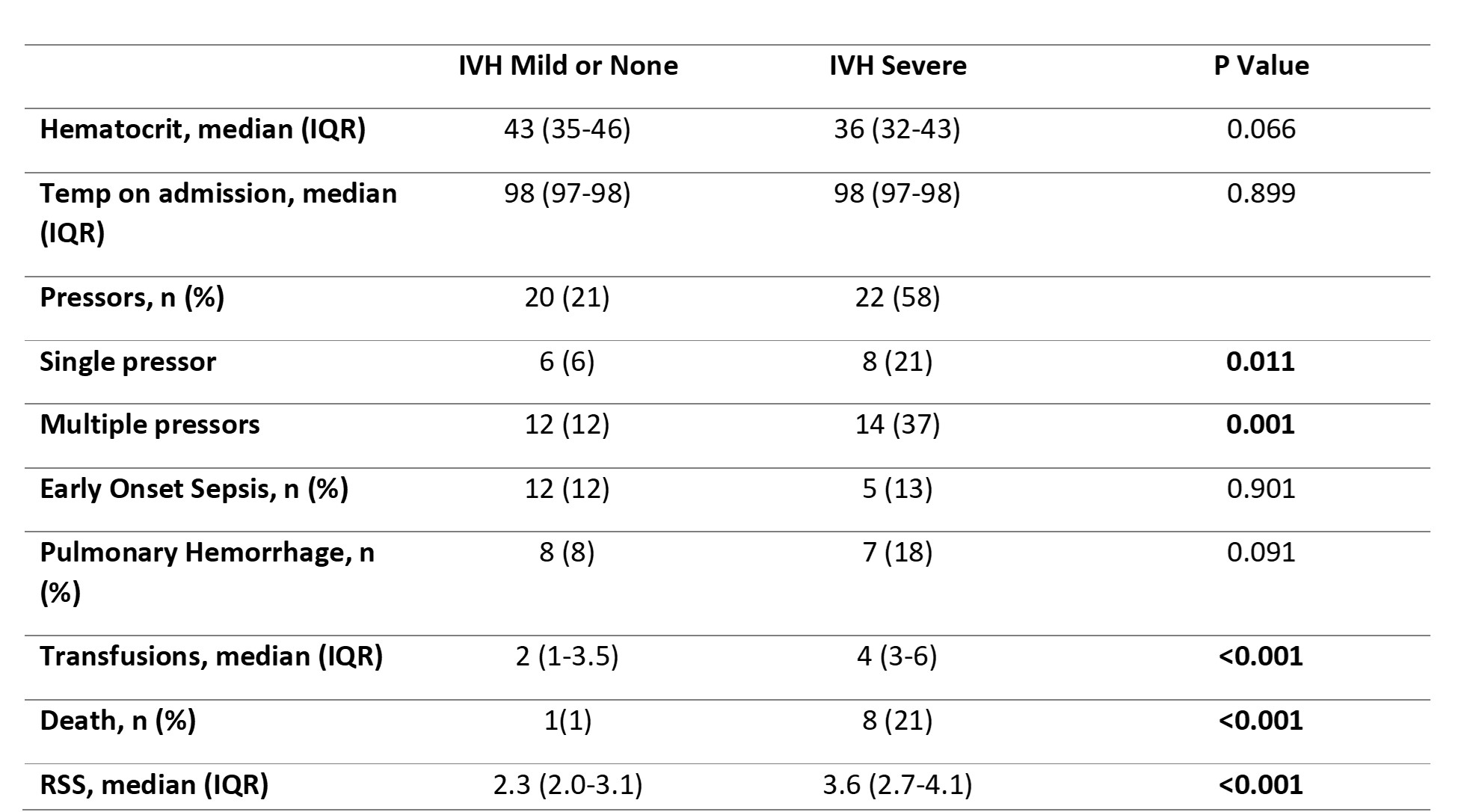
Objective: The study aimed to define the relationship between IVH and the development of progressive lung disease in extremely low birth weight (ELBW) infants placed on high frequency jet ventilators (HFJV). We hypothesized that infants with severe IVH had higher respiratory severity scores (RSSs) than infants with mild/none IVH within the first 7 days of life.
Design/Methods: This was a single-center retrospective cohort study. We enrolled preterm infants with a gestational age of less than 30 weeks of gestation, and birth weight of less than 1000 grams who were admitted to the NICU at Kentucky Children's Hospital between 2018-2021. We extracted demographic data for both neonates and mothers from the electronic medical record. HFJV daily settings in the first week of life were collected. We used RSS, the product of mean airway pressure (MAP) and fraction of inspired oxygen (FiO2) to estimate the severity of neonatal lung disease.
Results: 135 infants met the inclusion criteria. 72% of neonates had none/low grade IVH (Grade I or Grade II), while 28% had severe IVH (Grade III or Grade IV). Infants who had severe IVH had significantly lower gestational ages [(24.3 0 ± 1.0 vs. 26.0 ± 1.8); p < 0.001], birth weights [(667 ± 138 vs. 732 ± 147); p=0.021] and were delivered vaginally (63% vs. 82%; p=0.018). Neonates with severe IVH were more likely to be placed on single (21% vs. 6%; p=0.011) or multiple pressors (37% vs. 12%; p=0.001), and receive blood transfusion (p < 0.001) within the first 7 days of life. Postnatal RSSs were correlated with IVH severity. We found a trend of worsening RSSs within the first week of life in the group of infants with severe IVH. The median RSS (IQR) in the severe IVH group and none/low grade IVH group was 3.6 (2.7-4.1) and 2.3 (2.0-3.1), respectively (p < 0.001).Conclusion(s): This study is first to show that severe IVH is associated with higher RSSs predicting early lung injury in ELBW infants placed on a mechanical ventilator within the first 7 days of life. The injury of the lungs is explained by the increasing trend of RSSs within the first week of life. We speculate that after severe IVH, inflammatory markers are released into the systemic circulation, affecting extracerebral organs particularly leading to worsening lung injury. A prospective study is needed to better assess the relationship between IVH and RSSs.
Demographic Data.
Clinical Variables in the First Week of Life.