Neonatal Pulmonology
Category: Abstract Submission
Neonatal Pulmonology V: Preclinical studies and Clinical Care Issues
474 - Association of Mycoplasma and Ureaplasma Respiratory Colonization and Bronchopulmonary Dysplasia in Extremely Preterm Infants- A Propensity Score Matched Case-Control Study
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 474
Publication Number: 474.433
Publication Number: 474.433
Vivek V. Shukla, University of Alabama at Birmingham, Birmingham, AL, United States; Binh Vu, University of Alabama School of Medicine, Hoover, AL, United States; Crystal Seales, University of Alabama School of Medicine, Birmingham, AL, United States; AKM F. Rahman, University of Alabama at Birmingham, Vestavia, AL, United States; Colm P. Travers, University of Alabama at Birmingham, Birmingham, AL, United States; Kent A. Willis, The University of Alabama at Birmingham, Birmingham, AL, United States; Charitharth Vivek Lal, University of Alabama at Birmingham, AL, Birmingham, AL, United States; Donna Crabb, University of Alabama at Birmingham, Birmingham, AL, United States; Amy E. Ratliff, University of Alabama School of Medicine, Birmingham, AL, United States; Thomas P. Atkinson, University of Alabama School of Medicine, Birmingham, AL, United States; Ken Waites, University of Alabama at Birmingham, Birmingham, AL, United States; Waldemar A. Carlo, University of Alabama at Birmingham, Birmingham, AL, United States; Namasivayam Ambalavanan, University of Alabama School of Medicine, Birmingham, AL, United States

Vivek Shukla, MD (he/him/his)
Assistant Professor
University of Alabama at Birmingham
Birmingham, Alabama, United States
Presenting Author(s)
Background: Several unmatched observational studies have shown that extremely preterm (≤28 6/7 weeks gestational age, EP) infants with bronchopulmonary dysplasia (BPD) have a higher incidence of respiratory colonization with Mycoplasma and Ureaplasma. As respiratory colonization with Mycoplasma and Ureaplasma cannot be replicated as a randomized trial, the available evidence for increased risk of BPD in infants with Mycoplasma and Ureaplasma colonization is weak.
Objective: To test the hypothesis that EP Infants with both Mycoplasma and Ureaplasma respiratory colonization will have the highest risk of developing BPD compared to either microbe alone.
Design/Methods: Propensity score-matched case-control design comparing infants with Mycoplasma, Ureaplasma, and combined Mycoplasma and Ureaplasma respiratory colonization with matched controls. EP infants admitted to the UAB Hospital with respiratory (tracheal aspirate/nasopharyngeal) culture for Mycoplasma and Ureaplasma from January 01, 2014, to September 30, 2021, were included. The primary outcome was BPD (≥grade 2 by Jensen’s classification) or death by 36 weeks postmenstrual age (PMA). Propensity score 1:1 matching using nearest neighbor was done by logistic regression analysis using the variables of gestational age, birth weight, race, sex, and antenatal corticosteroid exposure and using the caliper distance cut-off of 0.15.
Results: A total of 512 EP infants were included. Colonization distribution was: 157 (30.6%) had either Mycoplasma or Ureaplasma or both, 65 (12.7%) had Mycoplasma (26 alone, 39 with Ureaplasma), 131 (25.6%) had Ureaplasma (92 alone, 39 with Mycoplasma), 39 (7.6%) with both, and 355 (69.3%) with none (Figure). On propensity score-matched analysis, there was no difference in the incidence of BPD/death between the infants colonized with both Mycoplasma and Ureaplasma as compared to the non-colonized (15/37 (40%) vs. 17/37 (46%), p= 0.59). Additionally, there was no difference in the incidence of BPD/death between the infants in either of the colonized groups compared to the non-colonized group (all p > 0.05, Table).Conclusion(s): The findings of the current propensity score-matched case-control study suggest no increase in the risk of BPD or death by 36 weeks PMA in EP infants with Mycoplasma and/or Ureaplasma respiratory colonization at birth. As all colonized infants were treated with appropriate antibiotics, the risks of untreated colonization cannot be ascertained in this study.
Figure: Participant Distribution and Outcomes by Colonization Status.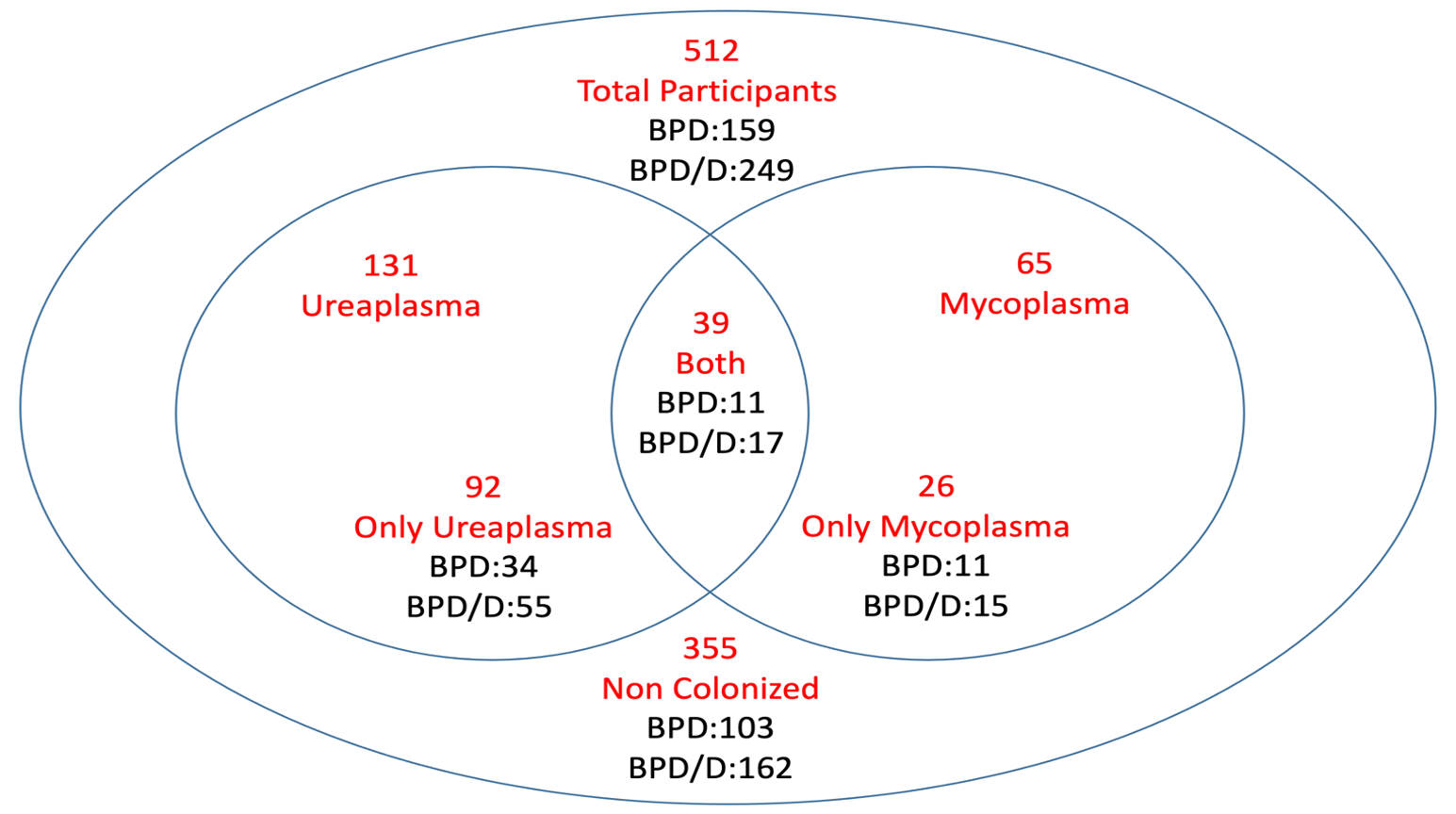 Colonization distribution was as follows: Of 512 infants, 157 had either Mycoplasma or Ureaplasma or both: 65 (12.7%) with Mycoplasma (26 alone, 39 with Ureaplasma), 131 (25.6%) with Ureaplasma (92 alone, 39 with Mycoplasma), 39 (7.6%) with both, and 355 (69.3%) with none. Outcome: BPD or death by 36 weeks postmenstrual age. BPD= bronchopulmonary dysplasia, D=death.
Colonization distribution was as follows: Of 512 infants, 157 had either Mycoplasma or Ureaplasma or both: 65 (12.7%) with Mycoplasma (26 alone, 39 with Ureaplasma), 131 (25.6%) with Ureaplasma (92 alone, 39 with Mycoplasma), 39 (7.6%) with both, and 355 (69.3%) with none. Outcome: BPD or death by 36 weeks postmenstrual age. BPD= bronchopulmonary dysplasia, D=death.
Table: Outcome Comparison by Colonization Status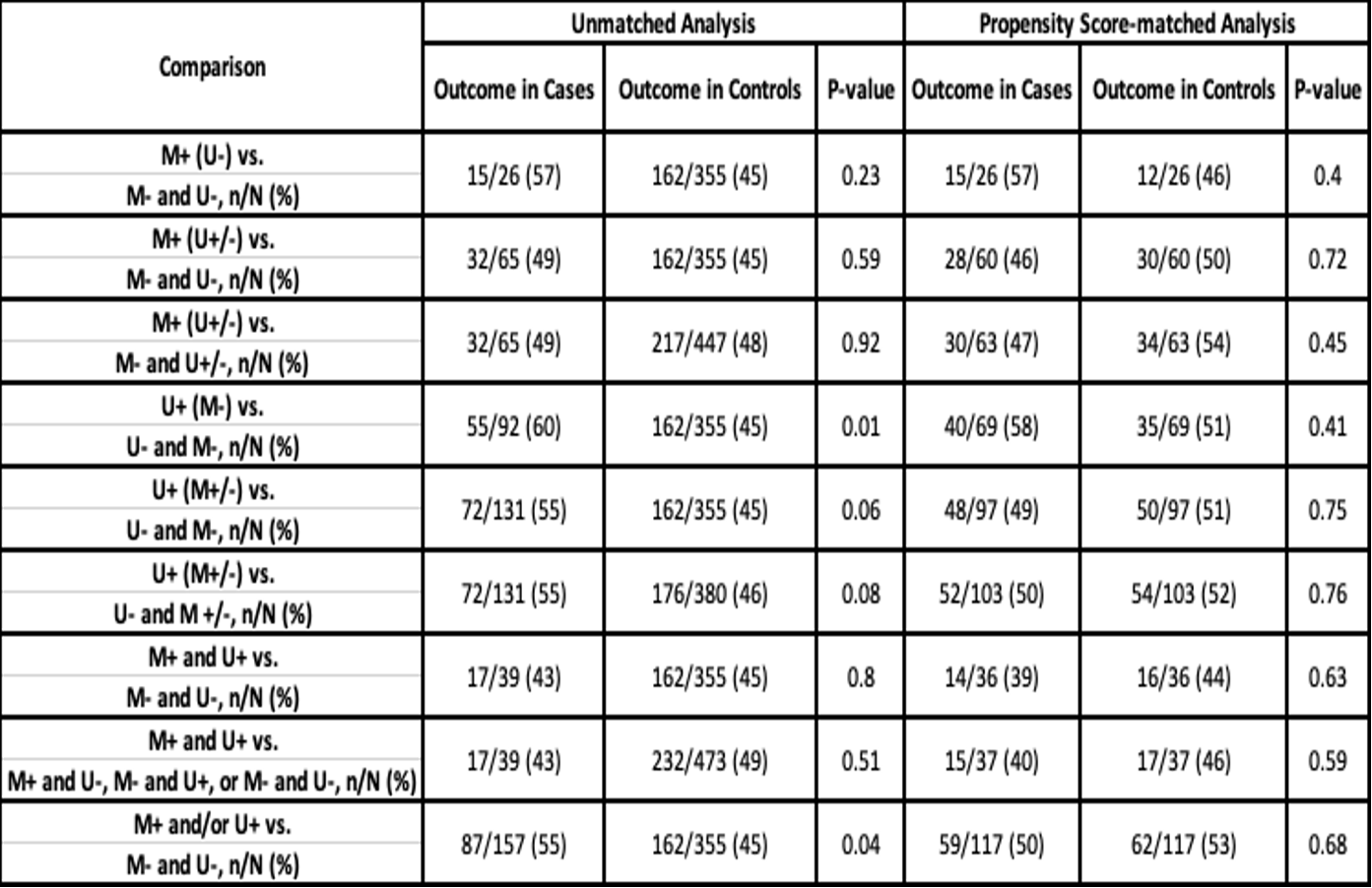 Outcome: BPD or death by 36 weeks postmenstrual age. M=Mycoplasma, U=Ureaplasma, +=positive, -=negative
Outcome: BPD or death by 36 weeks postmenstrual age. M=Mycoplasma, U=Ureaplasma, +=positive, -=negative
Objective: To test the hypothesis that EP Infants with both Mycoplasma and Ureaplasma respiratory colonization will have the highest risk of developing BPD compared to either microbe alone.
Design/Methods: Propensity score-matched case-control design comparing infants with Mycoplasma, Ureaplasma, and combined Mycoplasma and Ureaplasma respiratory colonization with matched controls. EP infants admitted to the UAB Hospital with respiratory (tracheal aspirate/nasopharyngeal) culture for Mycoplasma and Ureaplasma from January 01, 2014, to September 30, 2021, were included. The primary outcome was BPD (≥grade 2 by Jensen’s classification) or death by 36 weeks postmenstrual age (PMA). Propensity score 1:1 matching using nearest neighbor was done by logistic regression analysis using the variables of gestational age, birth weight, race, sex, and antenatal corticosteroid exposure and using the caliper distance cut-off of 0.15.
Results: A total of 512 EP infants were included. Colonization distribution was: 157 (30.6%) had either Mycoplasma or Ureaplasma or both, 65 (12.7%) had Mycoplasma (26 alone, 39 with Ureaplasma), 131 (25.6%) had Ureaplasma (92 alone, 39 with Mycoplasma), 39 (7.6%) with both, and 355 (69.3%) with none (Figure). On propensity score-matched analysis, there was no difference in the incidence of BPD/death between the infants colonized with both Mycoplasma and Ureaplasma as compared to the non-colonized (15/37 (40%) vs. 17/37 (46%), p= 0.59). Additionally, there was no difference in the incidence of BPD/death between the infants in either of the colonized groups compared to the non-colonized group (all p > 0.05, Table).Conclusion(s): The findings of the current propensity score-matched case-control study suggest no increase in the risk of BPD or death by 36 weeks PMA in EP infants with Mycoplasma and/or Ureaplasma respiratory colonization at birth. As all colonized infants were treated with appropriate antibiotics, the risks of untreated colonization cannot be ascertained in this study.
Figure: Participant Distribution and Outcomes by Colonization Status.
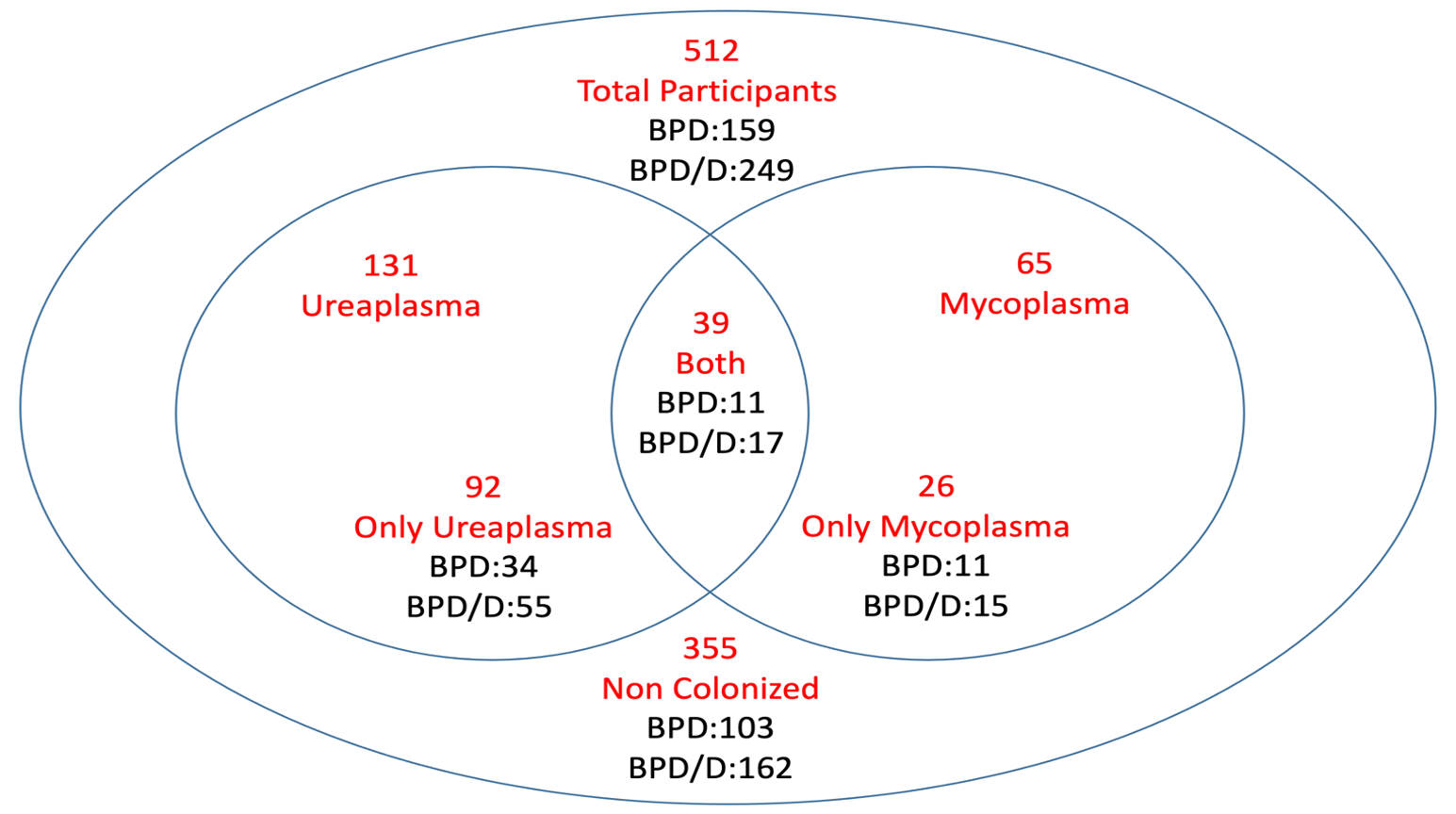 Colonization distribution was as follows: Of 512 infants, 157 had either Mycoplasma or Ureaplasma or both: 65 (12.7%) with Mycoplasma (26 alone, 39 with Ureaplasma), 131 (25.6%) with Ureaplasma (92 alone, 39 with Mycoplasma), 39 (7.6%) with both, and 355 (69.3%) with none. Outcome: BPD or death by 36 weeks postmenstrual age. BPD= bronchopulmonary dysplasia, D=death.
Colonization distribution was as follows: Of 512 infants, 157 had either Mycoplasma or Ureaplasma or both: 65 (12.7%) with Mycoplasma (26 alone, 39 with Ureaplasma), 131 (25.6%) with Ureaplasma (92 alone, 39 with Mycoplasma), 39 (7.6%) with both, and 355 (69.3%) with none. Outcome: BPD or death by 36 weeks postmenstrual age. BPD= bronchopulmonary dysplasia, D=death.Table: Outcome Comparison by Colonization Status
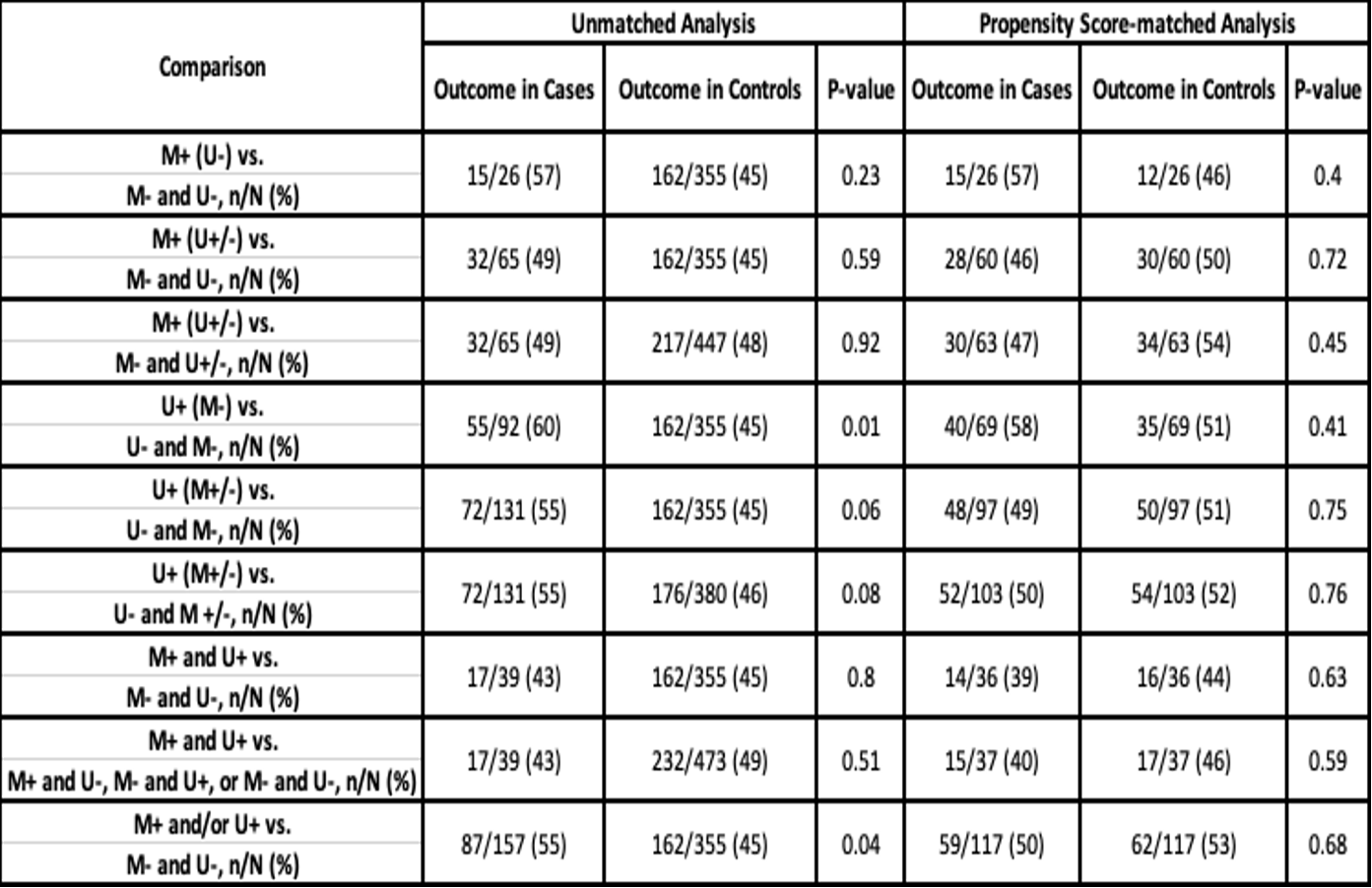 Outcome: BPD or death by 36 weeks postmenstrual age. M=Mycoplasma, U=Ureaplasma, +=positive, -=negative
Outcome: BPD or death by 36 weeks postmenstrual age. M=Mycoplasma, U=Ureaplasma, +=positive, -=negative