Child Abuse & Neglect
Category: Abstract Submission
Child Abuse & Neglect I
216 - Child protective services reporting in the context of intimate partner violence: A Delphi process
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 216
Publication Number: 216.401
Publication Number: 216.401
Camille Skinner, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States; Emily Killough, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Cynterria Henderson, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States; Adelaide Eichman, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Kimberly A. Randell, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Maya I. Ragavan, University of Pittsburgh, Wexford, PA, United States

Camille Skinner
Medical Student
University of Pittsburgh School of Medicine
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Child abuse and neglect (CAN) and intimate partner violence (IPV) often co-occur. Child protective services (CPS) reporting for families experiencing IPV is complex; state regulations and provider practices around reporting are variable.
Objective: The goals of this study were to: 1) determine indications for CPS reporting by pediatric providers in the context of IPV and 2) develop expert-driven best practices for use when CPS reporting is indicated.
Design/Methods: We conducted a modified Delphi study with multidisciplinary experts in IPV and CAN (pediatric providers, social workers, and IPV advocates). Participants completed 3 rounds of online anonymous surveys. In Round 1, participants reviewed 1) multiple scenarios involving IPV (e.g., child exposure to physical or sexual IPV) and indicated if CPS reporting was indicated and 2) a list of investigator-developed best practices for CPS reporting in the context of IPV, and suggested additional best practices. In Round 2, participants received a summary of Round 1 responses, and indicated degree of agreement with each indication for CPS reporting and best practice using a 5-point Likert scale. In Round 3, participants reviewed aggregated data from Rounds 1 and 2, and made final determinations regarding clinical scenarios and best practices. Descriptive statistics (frequency, means) were used; in Round 3, consensus was defined as >80% in agreement on an item.
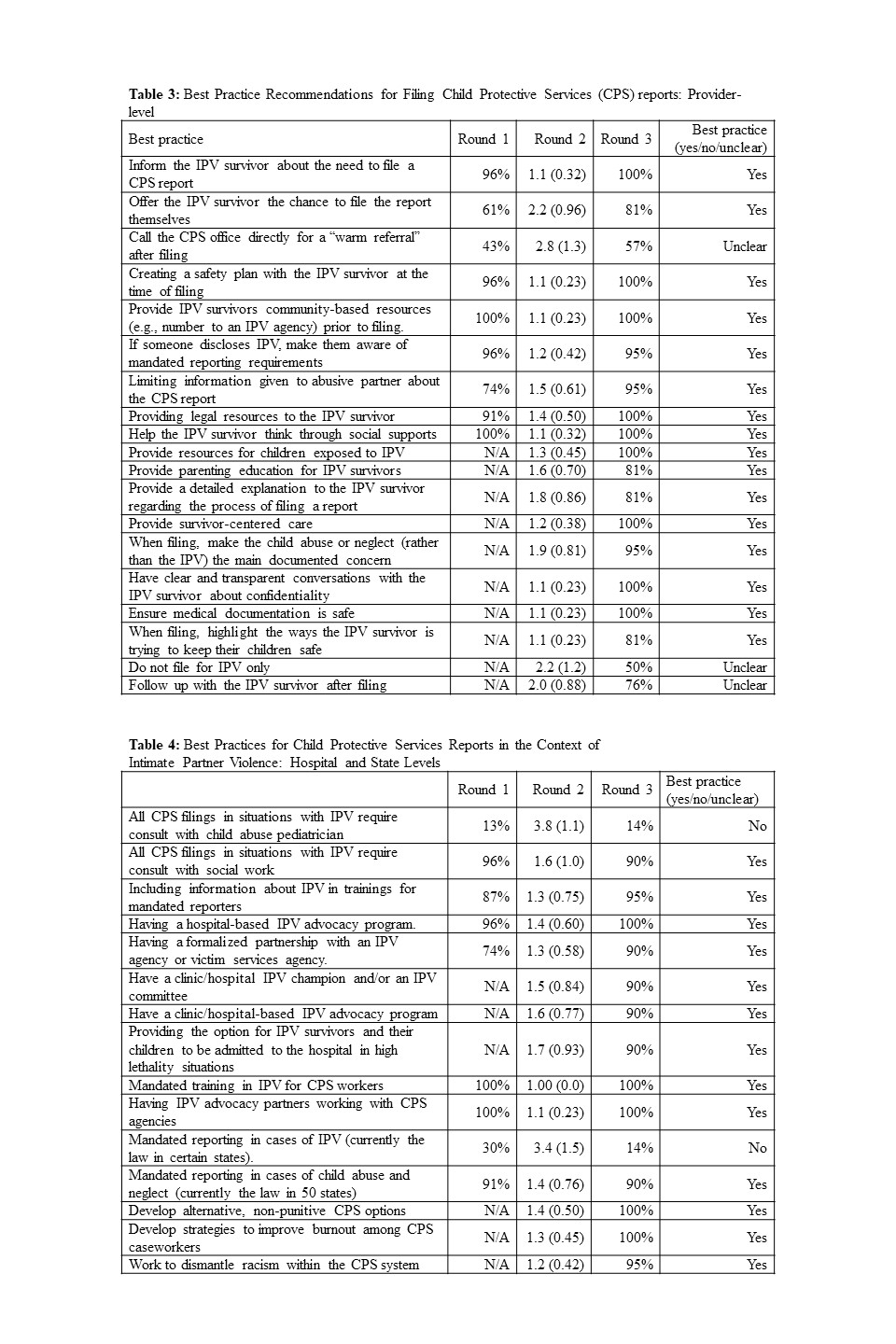
Results: Twenty-three (40%) of the invited experts participated (Table 1). Participants were in consensus that CPS reporting was indicated when CAN was present and not indicated for exposure to IPV only. Consensus was not reached for scenarios regarding children directly witnessing IPV or experiencing health symptoms due to IPV exposure (Table 2). Experts agreed on a variety of best practices when CPS filing is indicated in the context of IPV. These included mechanisms to support IPV survivors in clinical settings, such as resource provision, safety planning assistance, and healthcare-based IPV advocacy programs, as well as optimization of the child welfare system (Tables 3-4). Free responses acknowledged the complexity of this topic and limitations in CPS response (Table 5).Conclusion(s): This study provides expert-driven recommendations on indications for CPS reporting in the context of IPV and best practices to support IPV survivors and children when reporting. Findings highlight the inherent complexity of CPS reporting in these scenarios. Additional work is needed to further clarify best practices, including refining study findings with providers, IPV survivors and advocates, and CPS caseworkers.
CV - Camille Skinner.pdf
Tables 3 and 4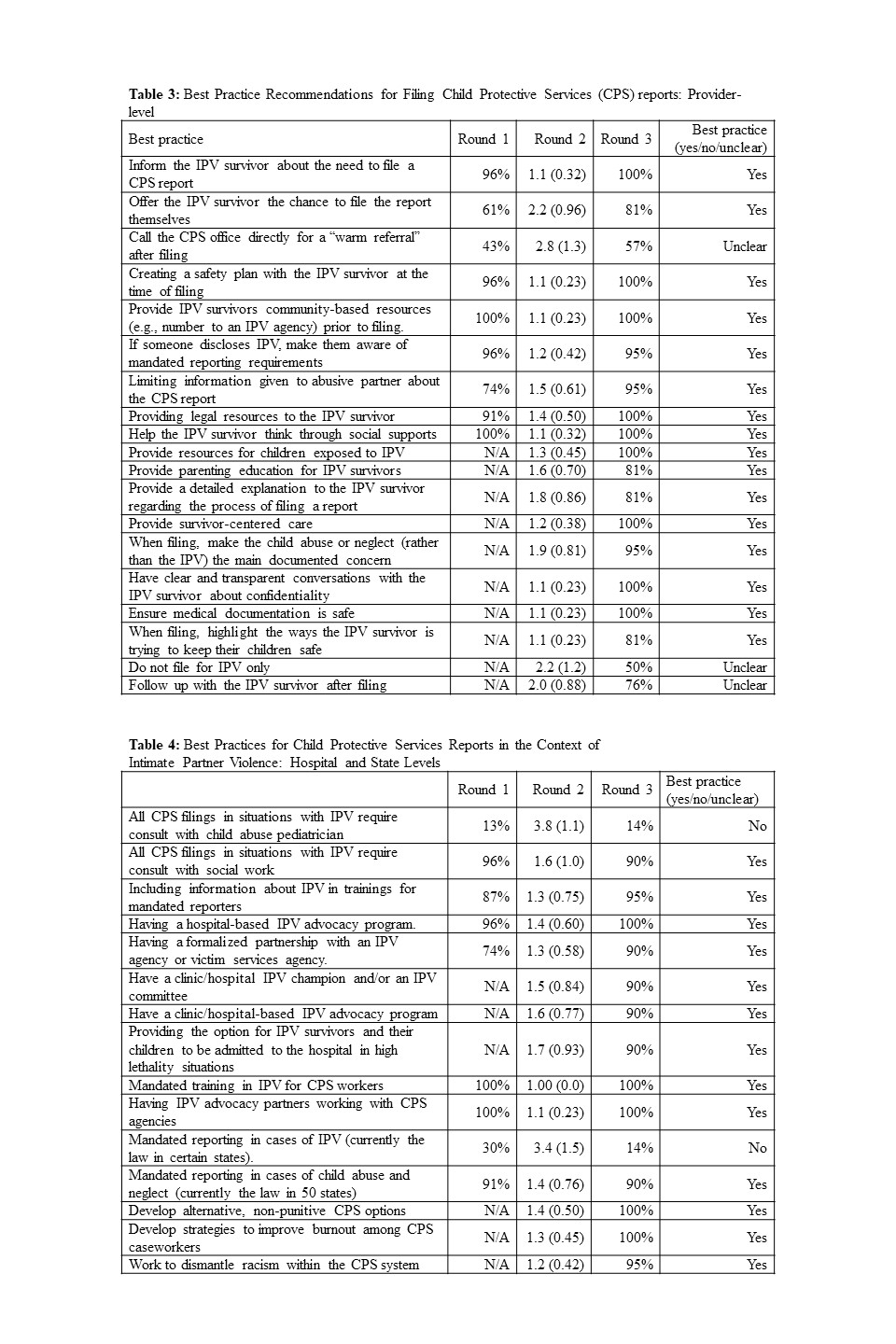
Objective: The goals of this study were to: 1) determine indications for CPS reporting by pediatric providers in the context of IPV and 2) develop expert-driven best practices for use when CPS reporting is indicated.
Design/Methods: We conducted a modified Delphi study with multidisciplinary experts in IPV and CAN (pediatric providers, social workers, and IPV advocates). Participants completed 3 rounds of online anonymous surveys. In Round 1, participants reviewed 1) multiple scenarios involving IPV (e.g., child exposure to physical or sexual IPV) and indicated if CPS reporting was indicated and 2) a list of investigator-developed best practices for CPS reporting in the context of IPV, and suggested additional best practices. In Round 2, participants received a summary of Round 1 responses, and indicated degree of agreement with each indication for CPS reporting and best practice using a 5-point Likert scale. In Round 3, participants reviewed aggregated data from Rounds 1 and 2, and made final determinations regarding clinical scenarios and best practices. Descriptive statistics (frequency, means) were used; in Round 3, consensus was defined as >80% in agreement on an item.
Results: Twenty-three (40%) of the invited experts participated (Table 1). Participants were in consensus that CPS reporting was indicated when CAN was present and not indicated for exposure to IPV only. Consensus was not reached for scenarios regarding children directly witnessing IPV or experiencing health symptoms due to IPV exposure (Table 2). Experts agreed on a variety of best practices when CPS filing is indicated in the context of IPV. These included mechanisms to support IPV survivors in clinical settings, such as resource provision, safety planning assistance, and healthcare-based IPV advocacy programs, as well as optimization of the child welfare system (Tables 3-4). Free responses acknowledged the complexity of this topic and limitations in CPS response (Table 5).Conclusion(s): This study provides expert-driven recommendations on indications for CPS reporting in the context of IPV and best practices to support IPV survivors and children when reporting. Findings highlight the inherent complexity of CPS reporting in these scenarios. Additional work is needed to further clarify best practices, including refining study findings with providers, IPV survivors and advocates, and CPS caseworkers.
CV - Camille Skinner.pdf
Tables 3 and 4