Back
Neonatal Neurology: Clinical
Category: Abstract Submission
Neurology 7: Neonatal Neurology Term Imaging
345 - Comparison of the prognostic value of different MRI techniques in neonatal encephalopathy: a systematic review and meta-analysis
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 345
Publication Number: 345.443
Publication Number: 345.443
Tim Hurley, Trinity College Dublin, Booterstown, Dublin, Ireland; Mary O'Dea, Health Service Executive, Dublin, Dublin, Ireland; Aoife Branagan, Coombe Woman and Infants University Hospital, Dublin, Dublin, Ireland; Megan Ni Bhroin, Trinity College dublin, Dublin, Dublin, Ireland; Megan Dibble, Trinity College Dublin, Manchester, England, United Kingdom; Arun Bokde, Trinity College Dublin, Dublin, Dublin, Ireland; Eleanor J Molloy, Trinity college the university of dublin, Dublin, Dublin, Ireland
- EM
Eleanor J Molloy, MB BCh BAO FRCPI PhD
Chair of Paediatrics
Trinity College Dublin
Dublin, Ireland
Presenting Author(s)
Background: Neonatal encephalopathy (NE) remains the primary cause long term neurodevelopmental disability in term newborns. An increasing number of interventions are available for newborns at risk of cerebral palsy and other neurodevelopmental conditions. It is critical that high risk patients are recognized early so that interventions can be implemented as early as possible. MRI offers valuable prognostic information in NE but the predictive value varies by MRI technique.
Objective: To examine the evidence currently available to determine the optimum MRI technique in NE.
Design/Methods: This meta-analysis was designed according to the Preferred Reporting Items for Systematic Reviews and Meta- Analyses (PRISMA) guidelines and registered with Prospero (CRD42021286461). PubMed, Embase, Web of Science, and the Cochrane database were searched with relevant search terms from January 1966 to July 2020. Observational and interventional studies that included patients over 35 weeks gestational age at birth with any clinical diagnosis of NE, that associated MRI results with neurodevelopmental outcomes, were included. The outcome was a composite of mortality or adverse neurodevelopmental outcome over 12 months of age. Screening, quality assessment and data extraction were completed using Covidence software. Risk of bias assessment was carried out using QUIPS-2 tool. Diagnostic odds ratio (DOR) was calculated using a random-effects model and Meta-analyst software.
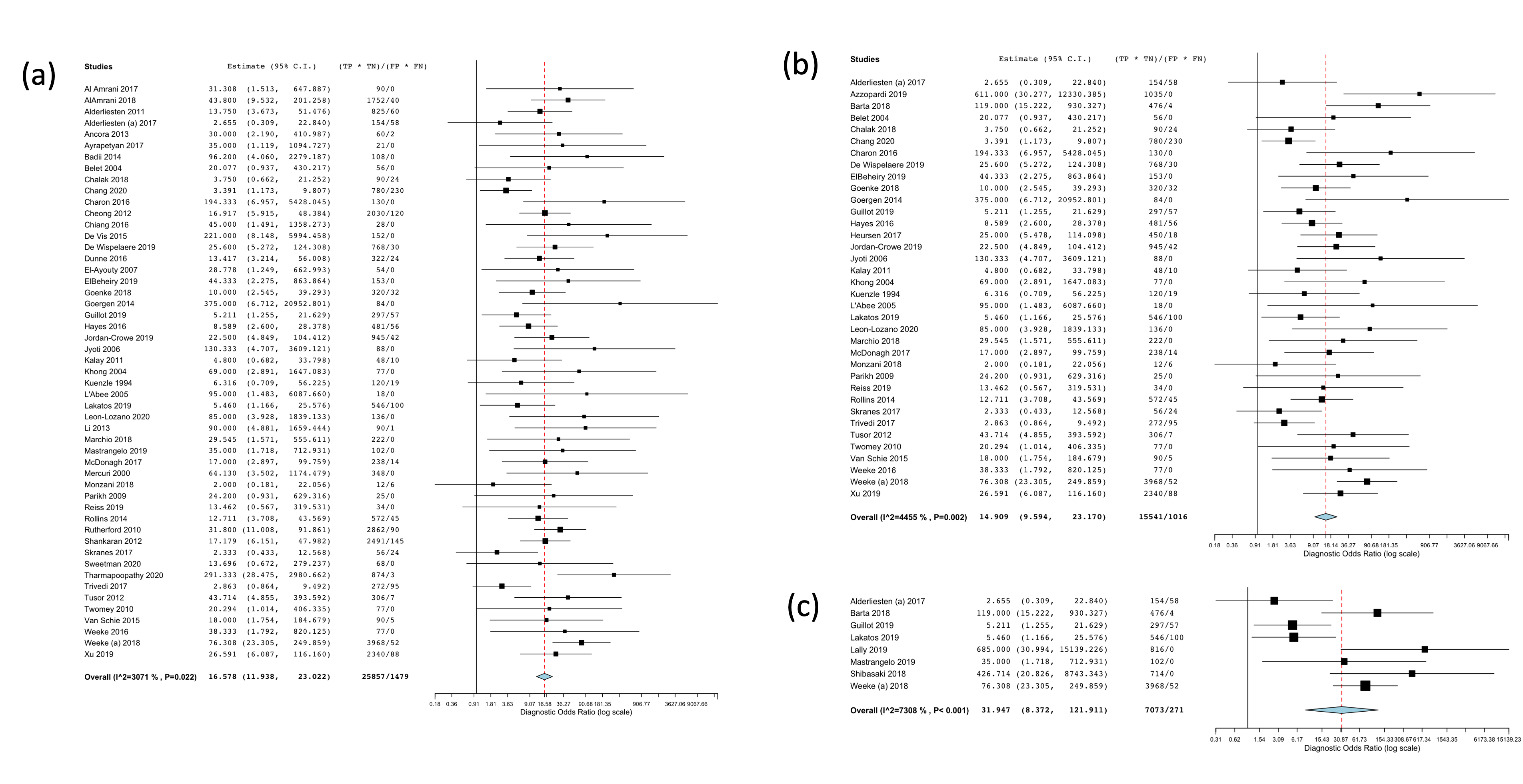
Results: The literature search provided 3626 results. Following title, abstract and full text screening 114 studies were included in the qualitative assessment, and 59 were included in the meta-analysis. The overall DOR of MRI in the diagnosis of adverse outcome was 20.98 (95% CI 14.76 – 29.83). 51 studies were included in the subgroup of conventional T1/T2 imaging which provided a DOR of 16.58 (95% CI 11.94 – 23.02). 36 studies were included in the diffusion weighted imaging subgroup which provided a DOR of 14.91 (95% CI 9.59 – 23.17). 8 studies were included in the magnetic resonance spectroscopy subgroup which provided a DOR of 31.95 (95% CI 8.37 – 121.91). There was moderate heterogeneity in the overall meta-analysis of MRI to predict outcome in NE (I2 42%).Conclusion(s): MRI is an excellent prognostic biomarker for outcome in NE. MRS appears to provide the highest DOR but the least consistent results between studies. Further work to examine the causes of heterogeneity and inconsistency between results is required. The optimum timing of MRI and the optimum MRS metabolites also requires examination.
Figure 1. Forest plot of the diagnostic log odds ratio for MRI in neonatal encephalopathy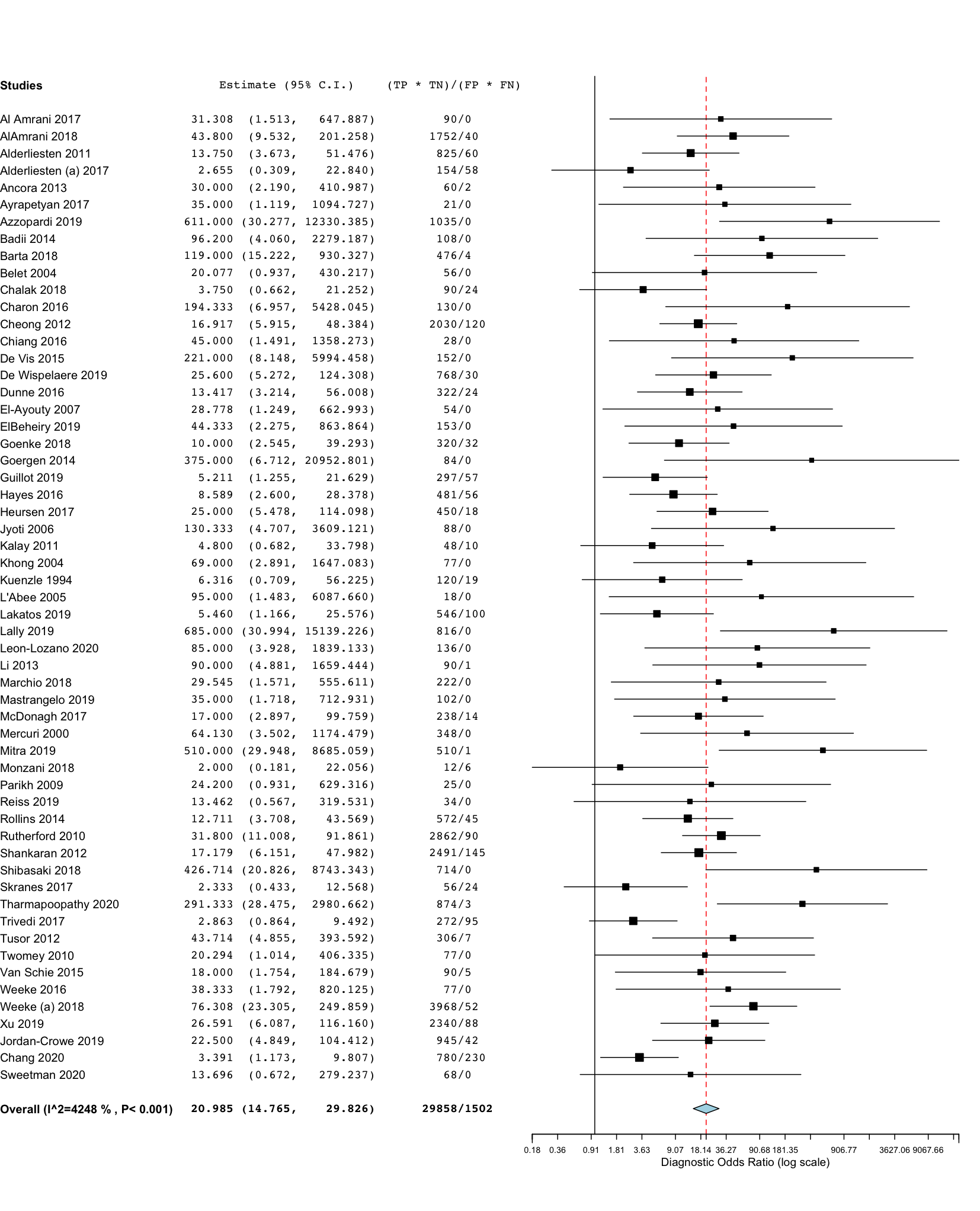
Figure 2. Forest plots of the diagnostic log odds ratio for (a) T1/T2 imaging (b) diffusion weighted imaging and (c) magnetic resonance spectroscopy in neonatal encephalopathy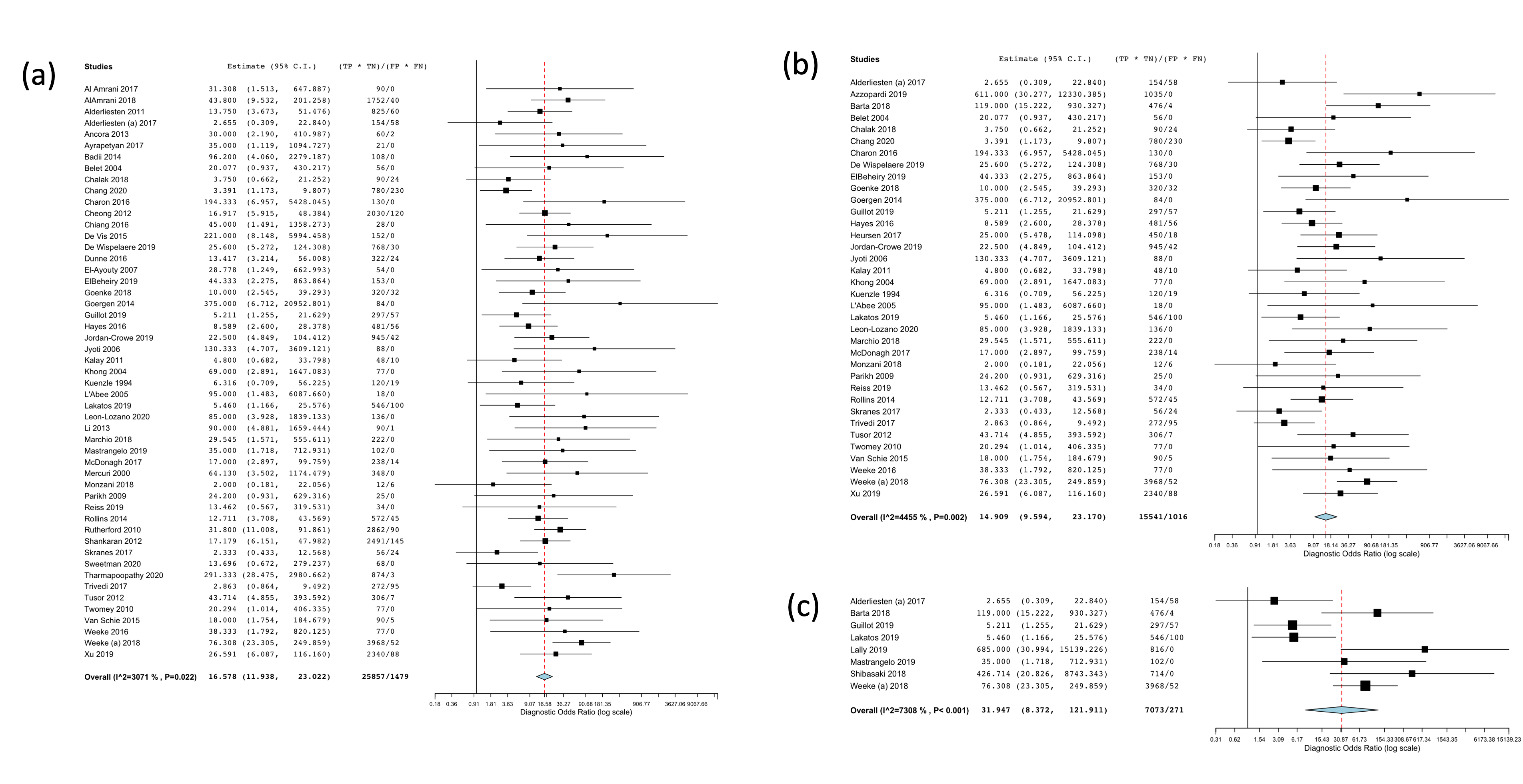
Objective: To examine the evidence currently available to determine the optimum MRI technique in NE.
Design/Methods: This meta-analysis was designed according to the Preferred Reporting Items for Systematic Reviews and Meta- Analyses (PRISMA) guidelines and registered with Prospero (CRD42021286461). PubMed, Embase, Web of Science, and the Cochrane database were searched with relevant search terms from January 1966 to July 2020. Observational and interventional studies that included patients over 35 weeks gestational age at birth with any clinical diagnosis of NE, that associated MRI results with neurodevelopmental outcomes, were included. The outcome was a composite of mortality or adverse neurodevelopmental outcome over 12 months of age. Screening, quality assessment and data extraction were completed using Covidence software. Risk of bias assessment was carried out using QUIPS-2 tool. Diagnostic odds ratio (DOR) was calculated using a random-effects model and Meta-analyst software.
Results: The literature search provided 3626 results. Following title, abstract and full text screening 114 studies were included in the qualitative assessment, and 59 were included in the meta-analysis. The overall DOR of MRI in the diagnosis of adverse outcome was 20.98 (95% CI 14.76 – 29.83). 51 studies were included in the subgroup of conventional T1/T2 imaging which provided a DOR of 16.58 (95% CI 11.94 – 23.02). 36 studies were included in the diffusion weighted imaging subgroup which provided a DOR of 14.91 (95% CI 9.59 – 23.17). 8 studies were included in the magnetic resonance spectroscopy subgroup which provided a DOR of 31.95 (95% CI 8.37 – 121.91). There was moderate heterogeneity in the overall meta-analysis of MRI to predict outcome in NE (I2 42%).Conclusion(s): MRI is an excellent prognostic biomarker for outcome in NE. MRS appears to provide the highest DOR but the least consistent results between studies. Further work to examine the causes of heterogeneity and inconsistency between results is required. The optimum timing of MRI and the optimum MRS metabolites also requires examination.
Figure 1. Forest plot of the diagnostic log odds ratio for MRI in neonatal encephalopathy
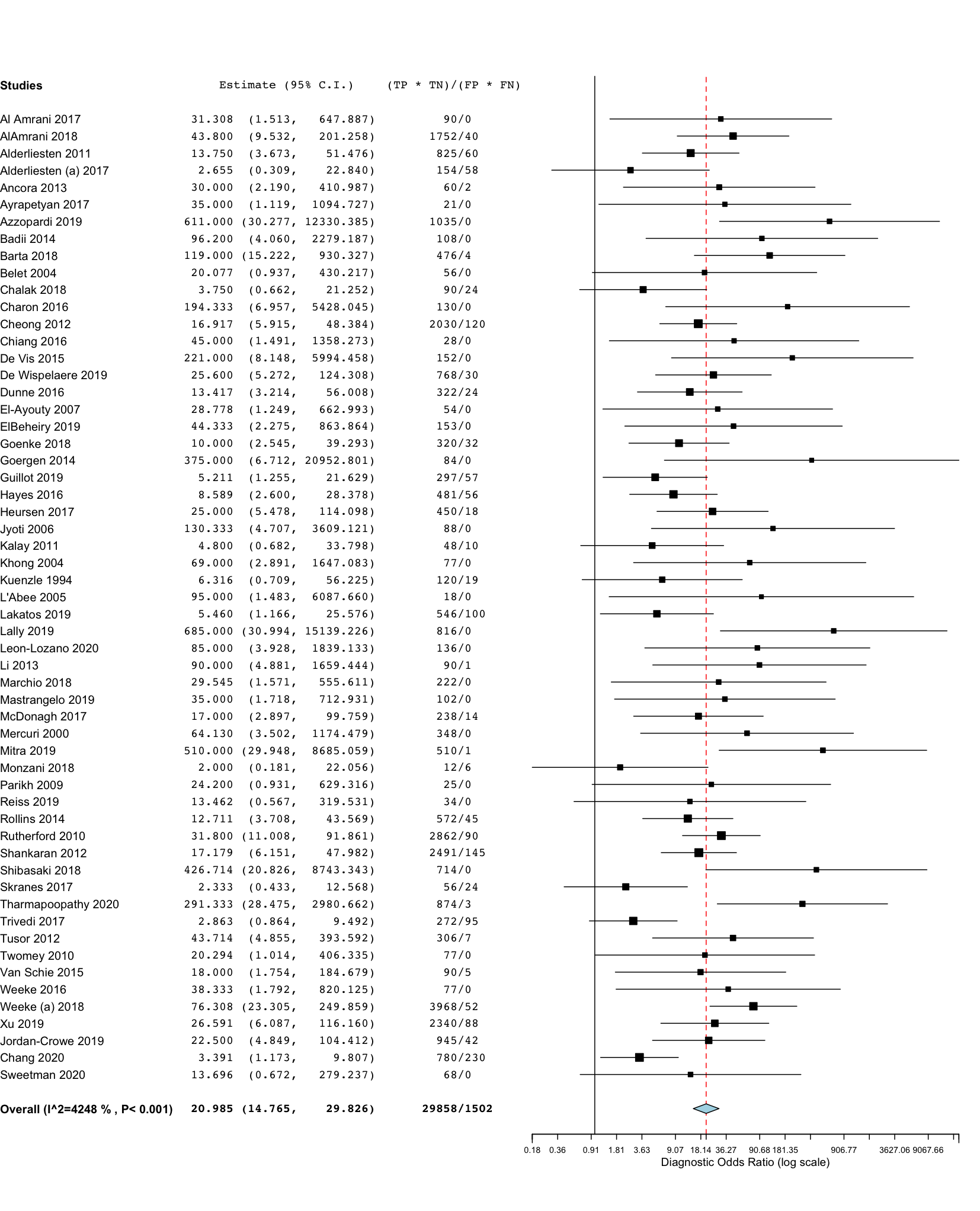
Figure 2. Forest plots of the diagnostic log odds ratio for (a) T1/T2 imaging (b) diffusion weighted imaging and (c) magnetic resonance spectroscopy in neonatal encephalopathy