Neonatal GI Physiology & NEC
Category: Abstract Submission
Neonatal GI Physiology & NEC I
486 - Detection of SARS-CoV-2 in stool but not nares of newborns of mothers with COVID-19 during pregnancy
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 486
Publication Number: 486.424
Publication Number: 486.424
Jenny C. Jin, NewYork-Presbyterian Komansky Children’s Hospital, Brooklyn, NY, United States; Aparna Ananthanarayanan, Weill Cornell Medicine, forest hills, NY, United States; Julia A. Brown, Weill Cornell Medicine, New York, NY, United States; Stephanie Rager, Weill Cornell Medicine, New York, NY, United States; Yaron Bram, Weill Cornell Medicine, New York, NY, United States; Katherine Sanidad, Weill Cornell Medicine, New York, NY, United States; Mohammed Amir, Weill Cornell Medicine, New york, NY, United States; Rebecca Baergen, Weill Cornell Medicine, New York, NY, United States; Heidi Stuhlmann, Weill Cornell Medicine, New York, NY, United States; Robert Schwartz, Weill Cornell Medicine, New York, NY, United States; Jeffrey Perlman, Weill Cornell Medicine, New York City, NY, United States; Melody Y. Zeng, Weill Cornell M, New York, NY, United States
- JJ
Jenny C. Jin, MD
NICU Fellow
NewYork-Presbyterian Weill Cornell Medicine
Brooklyn, New York, United States
Presenting Author(s)
Background: In utero transmission of SARS coronavirus 2 (SARS-CoV-2) has not been fully investigated. Negative nasal PCR tests in newborns born to mothers with COVID-19 during pregnancy do not exclude the possibility of SARS-CoV-2 present in other tissues, such as the intestine. Intestinal reservoirs of SARS-CoV-2 have been found in recovered adults, suggesting persistent intestinal viral accumulation.
Objective: To investigate potential evidence of in utero transmission of SARS-CoV-2 in the stool of newborns born to mothers with COVID-19 infection during pregnancy.
Design/Methods: We investigated stool from 1 day to 2 months of age from 14 newborns born at 25-41 weeks whose mothers had COVID-19 during pregnancy. Newborns were admitted at delivery to the NICU or newborn nursery of our urban academic hospital from July 2020 to May 2021. A comparison group of 30 newborns had similar GAs and were born to mothers without COVID-19 during pregnancy. SARS-CoV-2 RNA was quantified with quantitative PCR using primers against SARS-CoV-2 envelope protein and non-structural protein 14 (NSP-14), spike protein with ELISA, and inflammatory cytokines interleukin-6 (IL-6) and interferon-γ (IFN-γ) elicited by stool homogenates in mouse bone marrow macrophages. This study was IRB approved with parental consent.
Results: Despite negative nasal PCRs from all newborns, viral RNAs and spike protein were detected in the stool of 11 out of 14 newborns as early as the first day of life (range 0-2 months, Figure 2A, 2B). Stool RNA and spike protein levels increased over time in 2 and 4 newborns, respectively (Figure 3A, 3B). Stool homogenates from all newborns elicited elevated inflammatory cytokines, IL-6 and IFN-γ, from mouse macrophages (Figure 1). Most newborns were clinically well except for one death from gestational autoimmune liver disease and one with necrotizing enterocolitis.Conclusion(s): These novel findings suggest risk of in utero SARS-CoV-2 transmission to the premature and term fetal intestine during gestation despite negative postnatal nasal PCRs. It is unclear if the presence of viral RNA and protein within the gut microbiome represents active virus in newborns with clinical hospital courses typical of their gestational age in 12 out of 14 cases. However, increasing levels of viral RNA and protein over time suggest replication in some infants, and their gut microbiome induced inflammation in mouse models. The presence of SARS-CoV-2 RNA and spike protein in the intestines of newborns may potentially impact development of the gut microbiome and the immune system and should be further investigated.
CVCV Jenny Jin 010622.pdf
Figure 2. Detection of SARS-CoV-2 viral RNA and spike protein in stool specimens.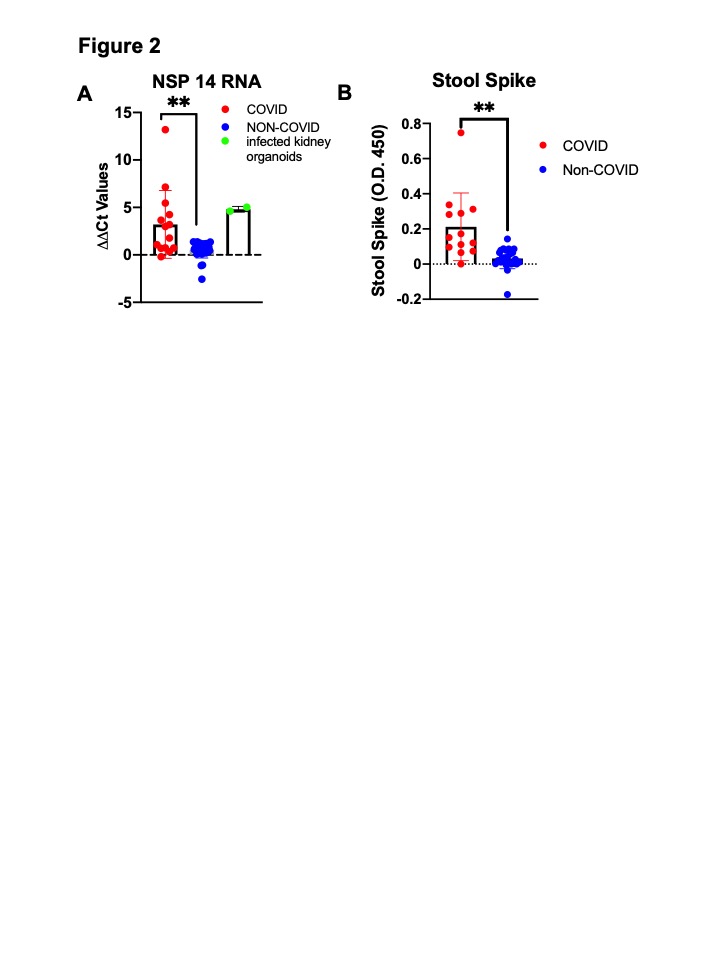 A. ∆∆Ct (levels quantified by qPCR) values of stool specimens collected from COVID-19 (n=14) and non-COVID-19 (n=11) groups using the primers for NSP 14. **p < 0.001; unpaired t test. Positive controls were kidney organoids infected with SARS-CoV-2. B. Detection of the spike protein in the stool samples of COVID-19 (n=14) and non-COVID-19 (n=30) neonates by enzyme-linked immunosorbent assay (ELISA). Relative amounts of spike in all stool specimens were shown as absorbance at O.D. 450 after subtracting background levels. **p < 0.001; unpaired t test. The stool specimens with the highest viral or spike protein were included for each neonate; GA-matched samples from neonates without maternal COVID-19 history were used for comparison.
A. ∆∆Ct (levels quantified by qPCR) values of stool specimens collected from COVID-19 (n=14) and non-COVID-19 (n=11) groups using the primers for NSP 14. **p < 0.001; unpaired t test. Positive controls were kidney organoids infected with SARS-CoV-2. B. Detection of the spike protein in the stool samples of COVID-19 (n=14) and non-COVID-19 (n=30) neonates by enzyme-linked immunosorbent assay (ELISA). Relative amounts of spike in all stool specimens were shown as absorbance at O.D. 450 after subtracting background levels. **p < 0.001; unpaired t test. The stool specimens with the highest viral or spike protein were included for each neonate; GA-matched samples from neonates without maternal COVID-19 history were used for comparison.
Objective: To investigate potential evidence of in utero transmission of SARS-CoV-2 in the stool of newborns born to mothers with COVID-19 infection during pregnancy.
Design/Methods: We investigated stool from 1 day to 2 months of age from 14 newborns born at 25-41 weeks whose mothers had COVID-19 during pregnancy. Newborns were admitted at delivery to the NICU or newborn nursery of our urban academic hospital from July 2020 to May 2021. A comparison group of 30 newborns had similar GAs and were born to mothers without COVID-19 during pregnancy. SARS-CoV-2 RNA was quantified with quantitative PCR using primers against SARS-CoV-2 envelope protein and non-structural protein 14 (NSP-14), spike protein with ELISA, and inflammatory cytokines interleukin-6 (IL-6) and interferon-γ (IFN-γ) elicited by stool homogenates in mouse bone marrow macrophages. This study was IRB approved with parental consent.
Results: Despite negative nasal PCRs from all newborns, viral RNAs and spike protein were detected in the stool of 11 out of 14 newborns as early as the first day of life (range 0-2 months, Figure 2A, 2B). Stool RNA and spike protein levels increased over time in 2 and 4 newborns, respectively (Figure 3A, 3B). Stool homogenates from all newborns elicited elevated inflammatory cytokines, IL-6 and IFN-γ, from mouse macrophages (Figure 1). Most newborns were clinically well except for one death from gestational autoimmune liver disease and one with necrotizing enterocolitis.Conclusion(s): These novel findings suggest risk of in utero SARS-CoV-2 transmission to the premature and term fetal intestine during gestation despite negative postnatal nasal PCRs. It is unclear if the presence of viral RNA and protein within the gut microbiome represents active virus in newborns with clinical hospital courses typical of their gestational age in 12 out of 14 cases. However, increasing levels of viral RNA and protein over time suggest replication in some infants, and their gut microbiome induced inflammation in mouse models. The presence of SARS-CoV-2 RNA and spike protein in the intestines of newborns may potentially impact development of the gut microbiome and the immune system and should be further investigated.
CVCV Jenny Jin 010622.pdf
Figure 2. Detection of SARS-CoV-2 viral RNA and spike protein in stool specimens.
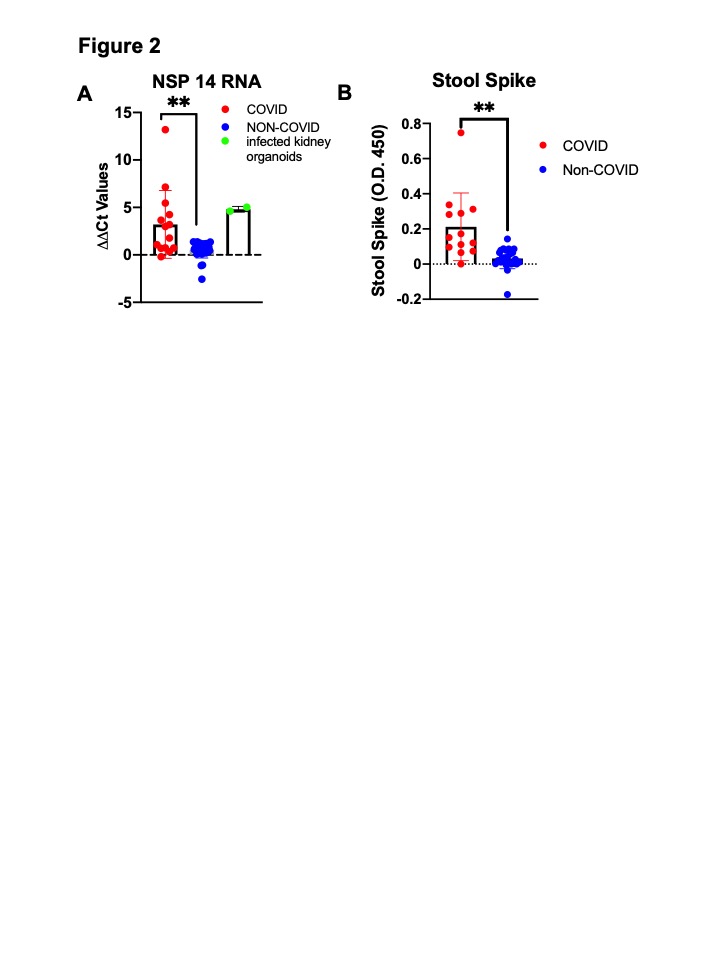 A. ∆∆Ct (levels quantified by qPCR) values of stool specimens collected from COVID-19 (n=14) and non-COVID-19 (n=11) groups using the primers for NSP 14. **p < 0.001; unpaired t test. Positive controls were kidney organoids infected with SARS-CoV-2. B. Detection of the spike protein in the stool samples of COVID-19 (n=14) and non-COVID-19 (n=30) neonates by enzyme-linked immunosorbent assay (ELISA). Relative amounts of spike in all stool specimens were shown as absorbance at O.D. 450 after subtracting background levels. **p < 0.001; unpaired t test. The stool specimens with the highest viral or spike protein were included for each neonate; GA-matched samples from neonates without maternal COVID-19 history were used for comparison.
A. ∆∆Ct (levels quantified by qPCR) values of stool specimens collected from COVID-19 (n=14) and non-COVID-19 (n=11) groups using the primers for NSP 14. **p < 0.001; unpaired t test. Positive controls were kidney organoids infected with SARS-CoV-2. B. Detection of the spike protein in the stool samples of COVID-19 (n=14) and non-COVID-19 (n=30) neonates by enzyme-linked immunosorbent assay (ELISA). Relative amounts of spike in all stool specimens were shown as absorbance at O.D. 450 after subtracting background levels. **p < 0.001; unpaired t test. The stool specimens with the highest viral or spike protein were included for each neonate; GA-matched samples from neonates without maternal COVID-19 history were used for comparison.