Infectious Diseases
Category: Abstract Submission
Infectious Diseases: Respiratory Viruses
578 - Development and Evaluation of a Multivariable Prediction Model for Influenza Hospitalization in Children
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 578
Publication Number: 578.417
Publication Number: 578.417
Suchitra Rao, University of Colorado School of Medicine, Aurora, CO, United States; Angela Moss, University of Colorado, Aurora, CO, United States; Amanda Dempsey, Merck, dENVER, CO, United States; Samuel R. Dominguez, Children's Hospital Colorado University of Colorado, Aurora, CO, United States; John D. Rice, University of Colorado School of Medicine, Aurora, CO, United States
.jpg)
Suchitra Rao, MBBS, MSCS (she/her/hers)
Associate Professor
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background: A risk-stratification tool for severe influenza infection based on objective clinical parameters that can be embedded in the electronic health record has the potential to lead to more standardized practice, reducing unnecessary testing and antiviral use.
Objective: Our objectives were to develop a prediction model to support influenza test decision-making in an emergent care setting.
Design/Methods: We conducted a retrospective cohort study to develop a predictive model for influenza hospitalization in children 6 months-18 years of age with acute respiratory illness who had influenza molecular testing during an emergency department (ED) or Urgent Care (UC) visit at a large quaternary center from 2010-2020. Candidate predictors included sociodemographic characteristics, co-morbidities and early vital sign data in the ED/UC. Three logistic regression models were trained: one with all predictors, one utilizing penalized regression, and a clinical model incorporating national guideline recommendations. The predictive accuracy of the models was assessed with internal and external validation. Model performance was assessed using area under the receiver operating characteristic curve (AUC), sensitivity, specificity, positive (PPV) and negative predictive values (NPV).
Results: Among 23,017 visits representing 17,492 children, 1419 children were hospitalized with influenza infection. Compared with children who were influenza negative, or not hospitalized, children who were hospitalized with PCR-confirmed influenza were more likely to be older (mean age 59 months vs 37 months, p < 0.0001), to be of Hispanic ethnicity (34% vs 32%, p = 0.0390) to have a high-risk medical condition (77% vs 68%, p < 0.0001) and were less likely to be of white race (58% vs 62%, p = 0.0008) (Table 1). All models had similar predictive accuracy (AUC 0.60-0.63). Age, adjusted respiratory rate and >1 high-risk comorbidity were the strongest predictors of severe influenza. With prediction risk threshold chosen for 90% sensitivity, the clinical model had specificity of 19.0%, PPV of 6.71% and NPV of 96.9%. Application of this risk threshold in a similar population would reduce unnecessary influenza testing by 18.4% (Table 2). Conclusion(s): A clinical model incorporating age, at least one high-risk comorbidity and respiratory rate/oxygen saturation with a high sensitivity threshold has high NPV with potential to reduce unnecessary influenza testing by approximately one-fifth.
Table 1. Sociodemographic and Clinical Characteristics of Cohort, by Influenza Result and Hospitalization Status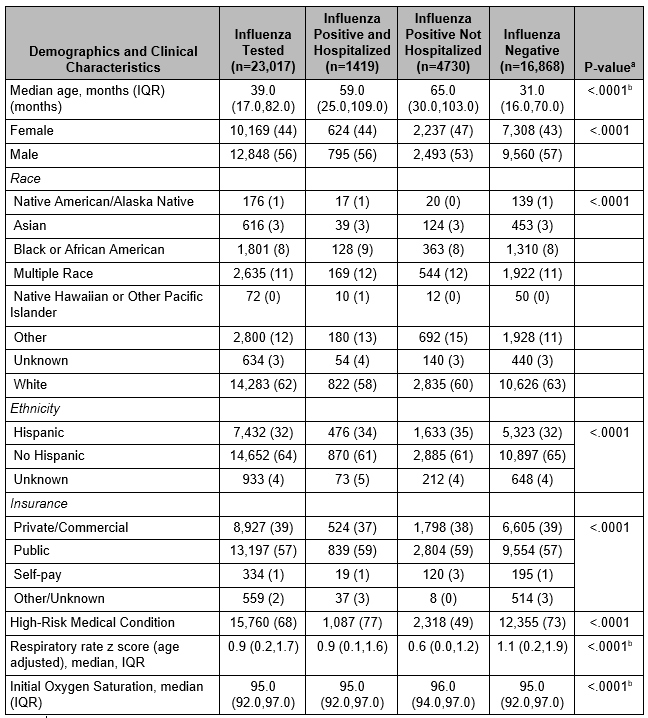 a-all p values calculated using Pearson Chi Square test unless otherwise specified
a-all p values calculated using Pearson Chi Square test unless otherwise specified
b-p values calculated using Kruskall-Wallis test
Table 2. Sensitivity, specificity, positive and negative predictive value for predictive models using training set to identify risk of hospitalization from influenza with threshold set at 90% sensitivity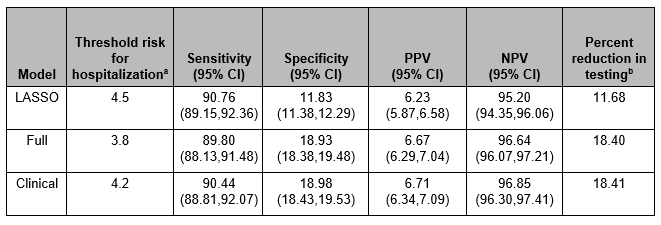 LASSO model included age (months), oxygen saturation
LASSO model included age (months), oxygen saturation
Full model included gender, race, ethnicity, payor, age (months), age and temperature adjusted heart rate (z score), age adjusted respiratory rate (z score), oxygen saturation, high risk medical condition (categorical)
Clinical model included age (months), oxygen saturation, age adjusted respiratory rate (z score) and presence of a high-risk medical condition.
a- Predicted probability threshold chosen to obtain approximately 90% sensitivity in training cohort
b- Percent reduction in testing that would occur using a sensitivity of 90%, and testing only those above the probability risk for hospitalization threshold
c- LASSO- least absolute shrinkage and selection operator (penalized regression model)
Objective: Our objectives were to develop a prediction model to support influenza test decision-making in an emergent care setting.
Design/Methods: We conducted a retrospective cohort study to develop a predictive model for influenza hospitalization in children 6 months-18 years of age with acute respiratory illness who had influenza molecular testing during an emergency department (ED) or Urgent Care (UC) visit at a large quaternary center from 2010-2020. Candidate predictors included sociodemographic characteristics, co-morbidities and early vital sign data in the ED/UC. Three logistic regression models were trained: one with all predictors, one utilizing penalized regression, and a clinical model incorporating national guideline recommendations. The predictive accuracy of the models was assessed with internal and external validation. Model performance was assessed using area under the receiver operating characteristic curve (AUC), sensitivity, specificity, positive (PPV) and negative predictive values (NPV).
Results: Among 23,017 visits representing 17,492 children, 1419 children were hospitalized with influenza infection. Compared with children who were influenza negative, or not hospitalized, children who were hospitalized with PCR-confirmed influenza were more likely to be older (mean age 59 months vs 37 months, p < 0.0001), to be of Hispanic ethnicity (34% vs 32%, p = 0.0390) to have a high-risk medical condition (77% vs 68%, p < 0.0001) and were less likely to be of white race (58% vs 62%, p = 0.0008) (Table 1). All models had similar predictive accuracy (AUC 0.60-0.63). Age, adjusted respiratory rate and >1 high-risk comorbidity were the strongest predictors of severe influenza. With prediction risk threshold chosen for 90% sensitivity, the clinical model had specificity of 19.0%, PPV of 6.71% and NPV of 96.9%. Application of this risk threshold in a similar population would reduce unnecessary influenza testing by 18.4% (Table 2). Conclusion(s): A clinical model incorporating age, at least one high-risk comorbidity and respiratory rate/oxygen saturation with a high sensitivity threshold has high NPV with potential to reduce unnecessary influenza testing by approximately one-fifth.
Table 1. Sociodemographic and Clinical Characteristics of Cohort, by Influenza Result and Hospitalization Status
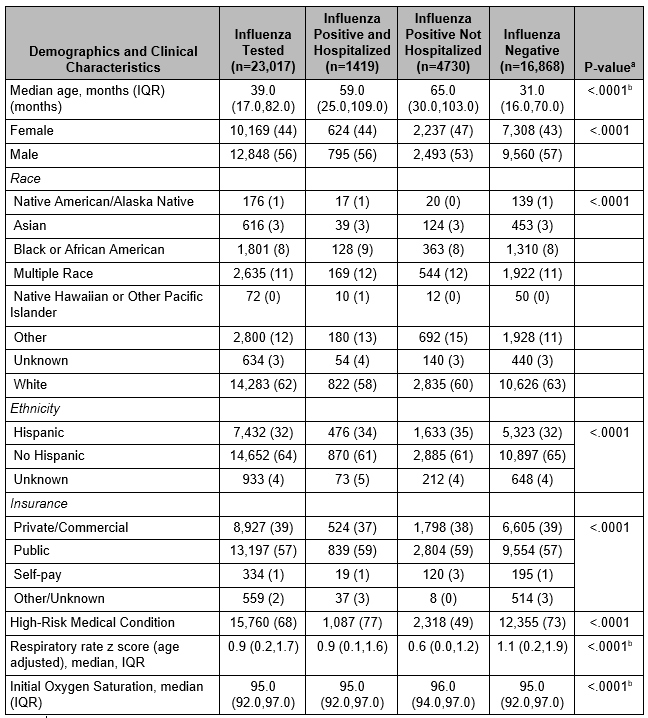 a-all p values calculated using Pearson Chi Square test unless otherwise specified
a-all p values calculated using Pearson Chi Square test unless otherwise specifiedb-p values calculated using Kruskall-Wallis test
Table 2. Sensitivity, specificity, positive and negative predictive value for predictive models using training set to identify risk of hospitalization from influenza with threshold set at 90% sensitivity
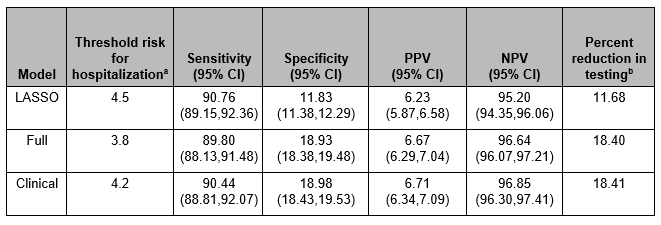 LASSO model included age (months), oxygen saturation
LASSO model included age (months), oxygen saturationFull model included gender, race, ethnicity, payor, age (months), age and temperature adjusted heart rate (z score), age adjusted respiratory rate (z score), oxygen saturation, high risk medical condition (categorical)
Clinical model included age (months), oxygen saturation, age adjusted respiratory rate (z score) and presence of a high-risk medical condition.
a- Predicted probability threshold chosen to obtain approximately 90% sensitivity in training cohort
b- Percent reduction in testing that would occur using a sensitivity of 90%, and testing only those above the probability risk for hospitalization threshold
c- LASSO- least absolute shrinkage and selection operator (penalized regression model)
