Back
Mental Health
Category: Abstract Submission
Mental Health II
537 - Evaluating Burnout Among Pediatric Residents During the COVID-19 Pandemic: A Mixed Methods Study
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 537
Natasha Dilwali, NewYork-Presbyterian Komansky Children’s Hospital, New York, NY, United States; Christina M. Tempesta, NewYork-Presbyterian Komansky Children’s Hospital, New York, NY, United States; Erika Abramson, Weill Cornell Medicine, New York, NY, United States; Laurie Gordon, Weill Cornell Medicine, NNew York, NY, United States; Sonia Ruparell, Boston Children's Hospital, Division of Orthopedics and Sports medicine, Division of Musculoskeletal Ultrasound and Harvard Medical School, Boston, MA, United States
- ND
Natasha Dilwali, MD
Resident
NewYork-Presbyterian Komansky Children’s Hospital
Weill Cornell Medicine The New York Presbyterian Hospital
New York, New York, United States
Presenting Author(s)
Background: COVID-19 continues to create uncertainty and unparalleled stress. Residents involved in caring for patients with COVID-19 are at high risk of developing negative psychological consequences such as burnout, depression, and anxiety. Compared to other physicians, residents have higher rates of burnout, fatigue, and depersonalization.
Objective: We explored the impact of the COVID-19 pandemic on resident burnout and sought program-level solutions to mitigate burnout.
Design/Methods: We conducted focus groups and administered the Maslach Burnout Inventory (MBI) to residents in a medium-sized, academic pediatric residency program in New York City. A constant comparison analysis was used to derive themes from focus groups until we achieved thematic saturation. Burnout on the MBI was defined as a high subscale score for the emotional exhaustion domain (≥27), and/or the depersonalization domain (≥10), and/or a low score in the personal achievement domain ( < 33). Scores were compared to results from residents in the same program in 2019.
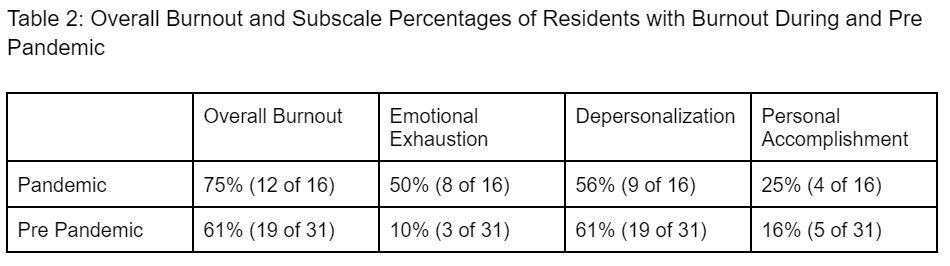
Results: Five focus groups were conducted among second and third-year residents (n=17 of 40). The MBI was completed by 16 of these residents. Five themes were identified (Table 1). First, burnout is accentuated during a pandemic due to pervasive feelings of personal isolation. Second, residents need programs to acknowledge the extent of the disruption as well as loss of normal coping strategies. Third, programs should ensure residents feel recognized for efforts above and beyond what ordinarily would be expected. Fourth, cultivating a culture of transparency around administrative decisions is essential. Lastly, burnout can be reduced through small program changes such as redistributing resident workload. 75% of respondents met the criteria for burnout from March to June 2020 compared to 61% in 2019. Depersonalization remained the highest subscale score (Table 2, 61% pre-pandemic, 56% during the pandemic). Percentage of residents with emotional exhaustion increased (Table 2, 10% pre-pandemic, 50% during the pandemic).Conclusion(s): Our study demonstrates pandemic burnout is unique and requires different mitigation and support strategies at the program level. By understanding the specific factors that contribute to burnout, early interventions can be implemented, which may mitigate the rising rates of depersonalization and emotional exhaustion seen throughout the pandemic.
Table 1: Thematic Analysis of Focus Groups with Correlating Quotes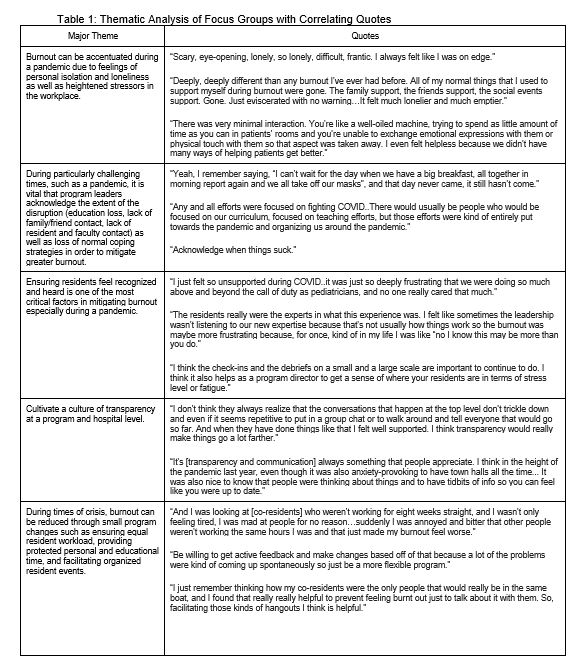
Table 2: Overall Burnout and Subscale Percentages of Residents with Burnout During and Pre Pandemic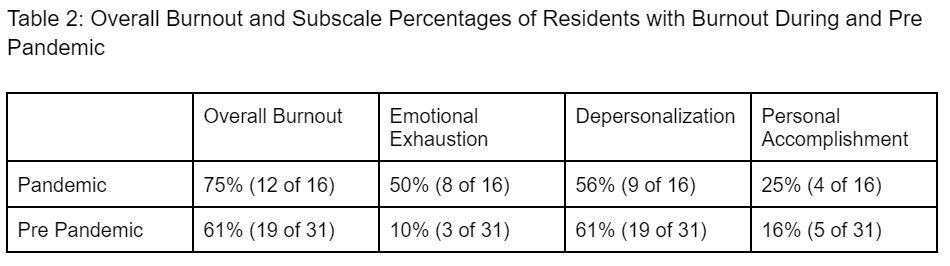
Objective: We explored the impact of the COVID-19 pandemic on resident burnout and sought program-level solutions to mitigate burnout.
Design/Methods: We conducted focus groups and administered the Maslach Burnout Inventory (MBI) to residents in a medium-sized, academic pediatric residency program in New York City. A constant comparison analysis was used to derive themes from focus groups until we achieved thematic saturation. Burnout on the MBI was defined as a high subscale score for the emotional exhaustion domain (≥27), and/or the depersonalization domain (≥10), and/or a low score in the personal achievement domain ( < 33). Scores were compared to results from residents in the same program in 2019.
Results: Five focus groups were conducted among second and third-year residents (n=17 of 40). The MBI was completed by 16 of these residents. Five themes were identified (Table 1). First, burnout is accentuated during a pandemic due to pervasive feelings of personal isolation. Second, residents need programs to acknowledge the extent of the disruption as well as loss of normal coping strategies. Third, programs should ensure residents feel recognized for efforts above and beyond what ordinarily would be expected. Fourth, cultivating a culture of transparency around administrative decisions is essential. Lastly, burnout can be reduced through small program changes such as redistributing resident workload. 75% of respondents met the criteria for burnout from March to June 2020 compared to 61% in 2019. Depersonalization remained the highest subscale score (Table 2, 61% pre-pandemic, 56% during the pandemic). Percentage of residents with emotional exhaustion increased (Table 2, 10% pre-pandemic, 50% during the pandemic).Conclusion(s): Our study demonstrates pandemic burnout is unique and requires different mitigation and support strategies at the program level. By understanding the specific factors that contribute to burnout, early interventions can be implemented, which may mitigate the rising rates of depersonalization and emotional exhaustion seen throughout the pandemic.
Table 1: Thematic Analysis of Focus Groups with Correlating Quotes
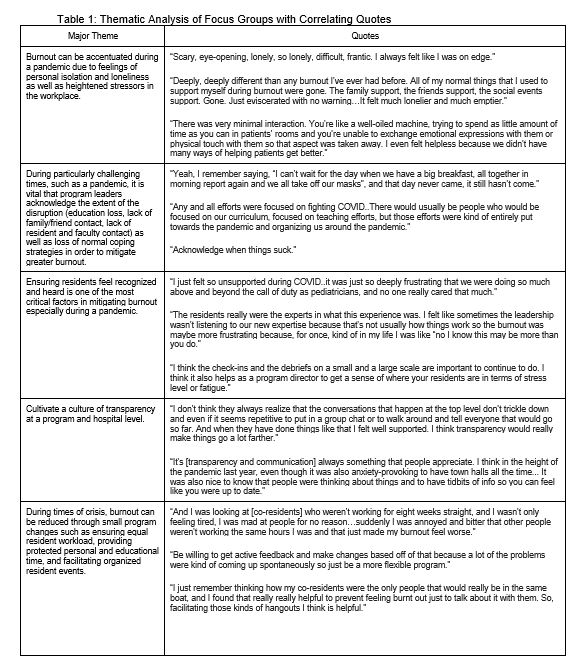
Table 2: Overall Burnout and Subscale Percentages of Residents with Burnout During and Pre Pandemic