Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine XV
64 - Feasibility of A Video Otoscope for Diagnosis of Otologic Pathology in Pediatric Patients
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 64
Publication Number: 64.408
Publication Number: 64.408
Jen Nystrom, Nationwide Children's Hospital, Columbus, OH, United States; Maya S. Iyer, Nationwide Children's Hospital, Columbus, OH, United States; Daniel J. Scherzer, Nationwide Children's Hospital, Columbus, OH, United States; Morgan Wurtz, DO, Nationwide Children's Hospital, Columbus, OH, United States; Charmaine Lo, Nationwide Children's Hospital, Columbus, OH, United States

Jen Nystrom, MD
Pediatric Emergency Medicine Fellow
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: Performing otoscopic exams can be difficult in pediatric patients secondary to patient compliance. This can lead to misdiagnosis, overtreatment, and complications of common pediatric otologic conditions like acute otitis media (AOM).
Objective: The purpose of this pilot study was to examine the feasibility of using a video otoscope for the diagnosis of otologic pathology in children presenting to a pediatric emergency department
Design/Methods: We obtained otoscopic videos using the JEDMED Horus + HD Video Otoscope. We randomized participants with fever, cough, congestion, respiratory or ear complaints to a video or standard otoscopy cohort and a physician completed their bilateral ear exams. Physicians reviewed otoscope videos with the patient’s caregiver. The caregiver and the physician then completed separate surveys using a 5-point Likert Scale regarding perceptions of the otoscopic exam.
Results: We enrolled 213 participants (94 standard otoscopy;119 video otoscopy). We used Wilcoxon rank sum testing to compare results across cohorts and age groups. There was no significant difference between video and standard otoscopy with regards to caregiver perception of comfort (p=0.54), cooperation (p =0.19), satisfaction (p =0.59), or diagnosis understanding (p =0.23). For physicians, there was no significant difference between cohorts with ease of device use (p=0.25) or quality of otoscopic view (R ear p =0.19, L ear p =0.053), though quality of view tended to be poorer with the video otoscope due to difficulties with focus, brightness, and view obstruction. Perceptions of length of time (LOT) to complete the ear exams were significantly longer using the video otoscope for both caregivers (p < 0.001) and physicians (p =0.01). There was no statistical difference in AOM diagnosis between cohorts (p=0.20). There were also no significant differences between cohorts when sub-analyzed by age group: 0-5 months (n=23, 11%), 6-23 months (n=65, 30%), 2-5 years old (n=60, 28%), and 6-18 years old (n=65, 30).Conclusion(s): Caregivers perceive that video and standard otoscopy are comparable in comfort, cooperation, exam satisfaction, and diagnosis understanding. However, exam LOT and otoscopic view satisfaction may limit the JEDMED’s feasibility in a busy pediatric emergency department.
CV - Jennifer Nystrom, MDOfficial Curriculum Vitae with signature.pdf
Physician Perceptions of Video vs Standard Otoscopy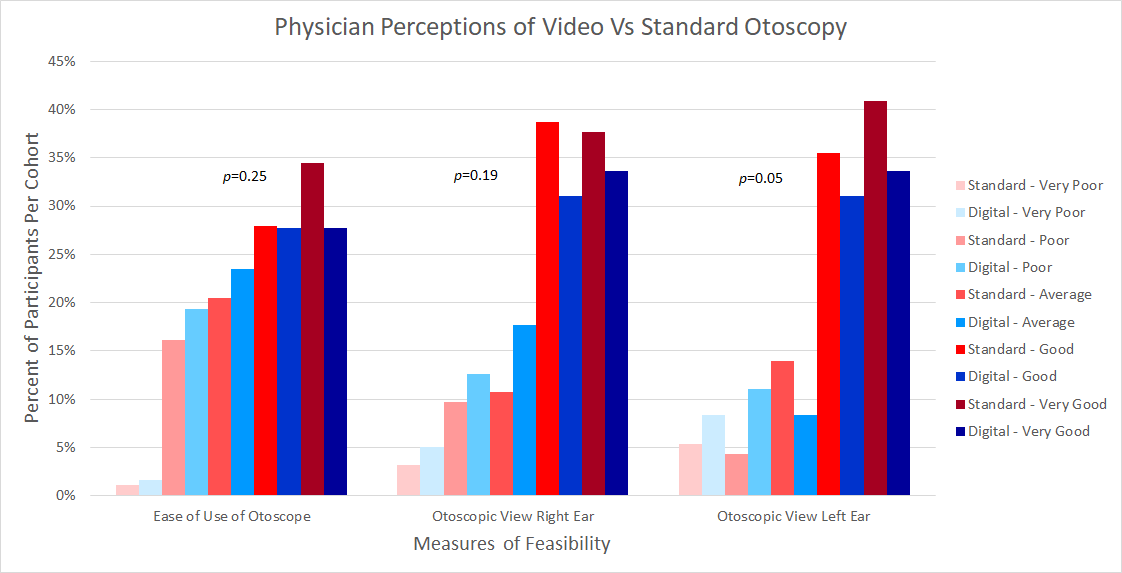 Physicians ranked their perceptions of video and standard otoscopy from 1 (very poor) to 5 (very good). Wilcoxon rank sum testing was used to analyze data.
Physicians ranked their perceptions of video and standard otoscopy from 1 (very poor) to 5 (very good). Wilcoxon rank sum testing was used to analyze data.
Objective: The purpose of this pilot study was to examine the feasibility of using a video otoscope for the diagnosis of otologic pathology in children presenting to a pediatric emergency department
Design/Methods: We obtained otoscopic videos using the JEDMED Horus + HD Video Otoscope. We randomized participants with fever, cough, congestion, respiratory or ear complaints to a video or standard otoscopy cohort and a physician completed their bilateral ear exams. Physicians reviewed otoscope videos with the patient’s caregiver. The caregiver and the physician then completed separate surveys using a 5-point Likert Scale regarding perceptions of the otoscopic exam.
Results: We enrolled 213 participants (94 standard otoscopy;119 video otoscopy). We used Wilcoxon rank sum testing to compare results across cohorts and age groups. There was no significant difference between video and standard otoscopy with regards to caregiver perception of comfort (p=0.54), cooperation (p =0.19), satisfaction (p =0.59), or diagnosis understanding (p =0.23). For physicians, there was no significant difference between cohorts with ease of device use (p=0.25) or quality of otoscopic view (R ear p =0.19, L ear p =0.053), though quality of view tended to be poorer with the video otoscope due to difficulties with focus, brightness, and view obstruction. Perceptions of length of time (LOT) to complete the ear exams were significantly longer using the video otoscope for both caregivers (p < 0.001) and physicians (p =0.01). There was no statistical difference in AOM diagnosis between cohorts (p=0.20). There were also no significant differences between cohorts when sub-analyzed by age group: 0-5 months (n=23, 11%), 6-23 months (n=65, 30%), 2-5 years old (n=60, 28%), and 6-18 years old (n=65, 30).Conclusion(s): Caregivers perceive that video and standard otoscopy are comparable in comfort, cooperation, exam satisfaction, and diagnosis understanding. However, exam LOT and otoscopic view satisfaction may limit the JEDMED’s feasibility in a busy pediatric emergency department.
CV - Jennifer Nystrom, MDOfficial Curriculum Vitae with signature.pdf
Physician Perceptions of Video vs Standard Otoscopy
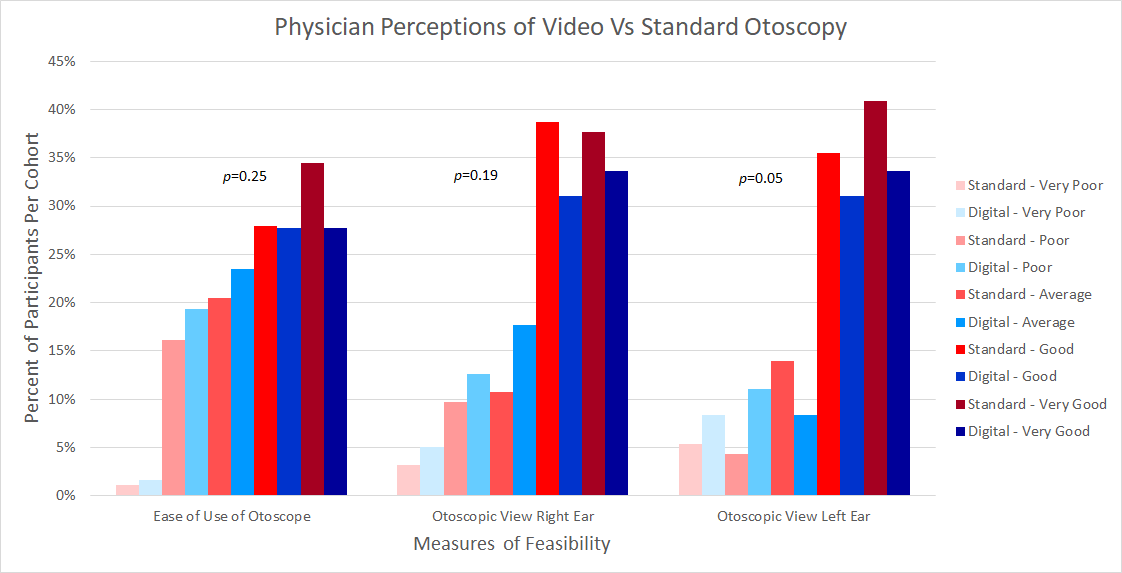 Physicians ranked their perceptions of video and standard otoscopy from 1 (very poor) to 5 (very good). Wilcoxon rank sum testing was used to analyze data.
Physicians ranked their perceptions of video and standard otoscopy from 1 (very poor) to 5 (very good). Wilcoxon rank sum testing was used to analyze data.