Back
Health Services Research
Category: Abstract Submission
Health Services Research III
8 - Feasibility of AI-assisted home-based remote auscultation for pediatric cardiology telemedicine visits
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 8
Publication Number: 8.414
Publication Number: 8.414
Jessica Campanile, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; William C. Golden, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Julia M. Kim, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Michael Crocetti, Johns Hopkins Community Physicians, Baltimore, MD, United States; W. Reid Thompson, Johns Hopkins Children's Center, Baltimore, MD, United States

Jessica Campanile, BA (she/they)
Medical Student
Perelman School of Medicine at the University of Pennsylvania
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: The use of AI-assisted remote auscultation during pediatric cardiology telemedicine visits may aid in clinical decision-making when determining need for echocardiogram or in-person evaluation as well as ease financial, logistical, and emotional burdens for pediatric patients and their families. We previously tested and found highly feasible AI-assisted auscultation when heart sounds were recorded and sent from primary healthcare settings for later cardiologist interpretation. With the onset of COVID-19 and increased use of telemedicine we hypothesized that in-home, synchronous remote auscultation with AI-assist could also be feasible and useful for determining need for echocardiography and in-person visits.
Objective: Assess in-home remote auscultation during pediatric cardiology telemedicine visits to determine potential feasibility and utility for routine clinical use and further study.
Design/Methods: 47 patients were recruited, consented and enrolled. During the video visit, the cardiologist guided patients and/or families through auscultation of the chest using an electronic stethoscope sent to the home. Heart and lungs sounds were evaluated in real-time and recorded. AI analysis (eMurmur®) determined heart rate and presence or absence of murmurs. User experience and clinical data were collected by electronic survey after the visit.
Results: Patient, family and cardiologist surveys showed in-home remote auscultation was successful in 96% of attempted cases with reasons for failure including patient factors (e.g. crying, moving) or technical issues. For most visits, recordings and their sound quality were suitable for AI-interpretation and clinical decision-making. Most patients and families felt the enhanced video visits were the same as or better than in-person visits (Figure). Clinical findings included presence of murmurs, other abnormal heart sounds and postural changes in heart rate (Table). In 70% of visits, 10-15 minutes were spent on remote auscultation. Auscultatory findings were used for clinical decision making.Conclusion(s): In-home remote cardiac auscultation is feasible, clinically valuable and acceptable to patients and providers. Additional potential benefits of recording heart and lung sounds with AI-assisted remote auscultation may be reduced variability of decision-making and the ability to compare findings to previous visits, resulting in more appropriate use of echocardiography. Beyond the pandemic, this technology should also lessen barriers to specialty care for under-resourced populations and patients living in remote locations.
Post-Visit Survey of Patients and Families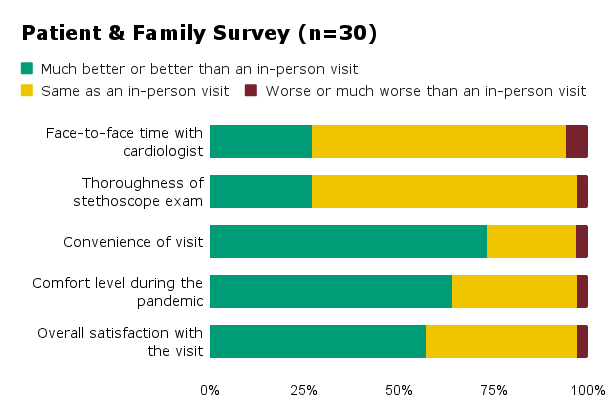 Patients and families (n=30) rated remote auscultation visit metrics compared to an in-person visit.
Patients and families (n=30) rated remote auscultation visit metrics compared to an in-person visit.
Auscultatory Findings Found by Remote Auscultation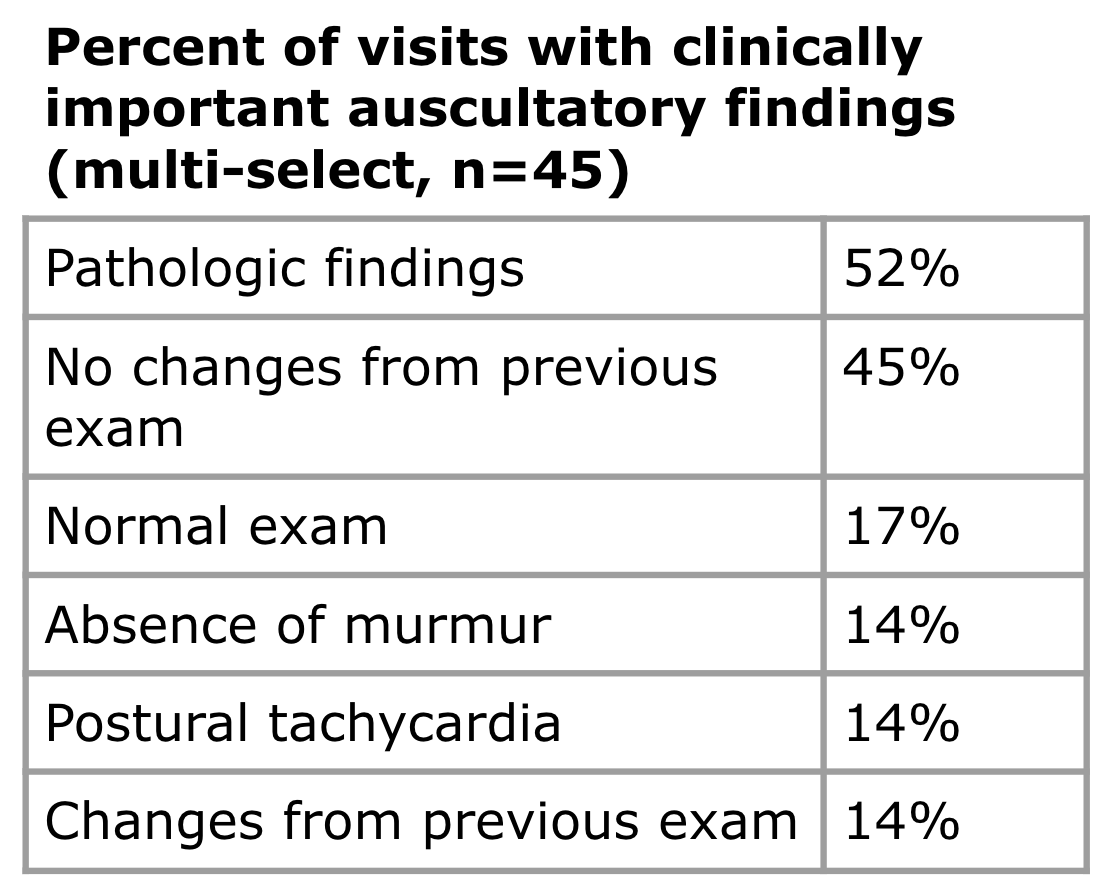 Percentage of visits (n=45) with selected clinically important findings according to cardiologist post visit survey is shown.
Percentage of visits (n=45) with selected clinically important findings according to cardiologist post visit survey is shown.
Objective: Assess in-home remote auscultation during pediatric cardiology telemedicine visits to determine potential feasibility and utility for routine clinical use and further study.
Design/Methods: 47 patients were recruited, consented and enrolled. During the video visit, the cardiologist guided patients and/or families through auscultation of the chest using an electronic stethoscope sent to the home. Heart and lungs sounds were evaluated in real-time and recorded. AI analysis (eMurmur®) determined heart rate and presence or absence of murmurs. User experience and clinical data were collected by electronic survey after the visit.
Results: Patient, family and cardiologist surveys showed in-home remote auscultation was successful in 96% of attempted cases with reasons for failure including patient factors (e.g. crying, moving) or technical issues. For most visits, recordings and their sound quality were suitable for AI-interpretation and clinical decision-making. Most patients and families felt the enhanced video visits were the same as or better than in-person visits (Figure). Clinical findings included presence of murmurs, other abnormal heart sounds and postural changes in heart rate (Table). In 70% of visits, 10-15 minutes were spent on remote auscultation. Auscultatory findings were used for clinical decision making.Conclusion(s): In-home remote cardiac auscultation is feasible, clinically valuable and acceptable to patients and providers. Additional potential benefits of recording heart and lung sounds with AI-assisted remote auscultation may be reduced variability of decision-making and the ability to compare findings to previous visits, resulting in more appropriate use of echocardiography. Beyond the pandemic, this technology should also lessen barriers to specialty care for under-resourced populations and patients living in remote locations.
Post-Visit Survey of Patients and Families
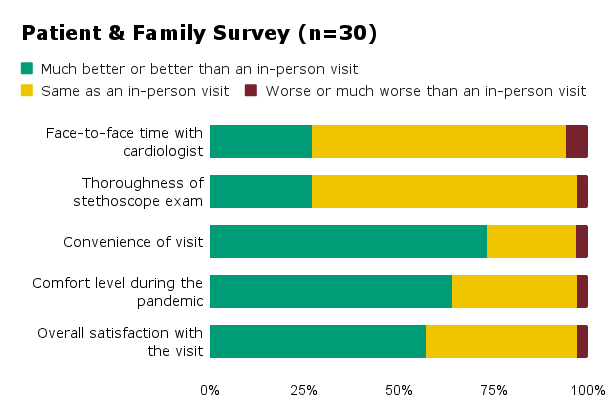 Patients and families (n=30) rated remote auscultation visit metrics compared to an in-person visit.
Patients and families (n=30) rated remote auscultation visit metrics compared to an in-person visit.Auscultatory Findings Found by Remote Auscultation
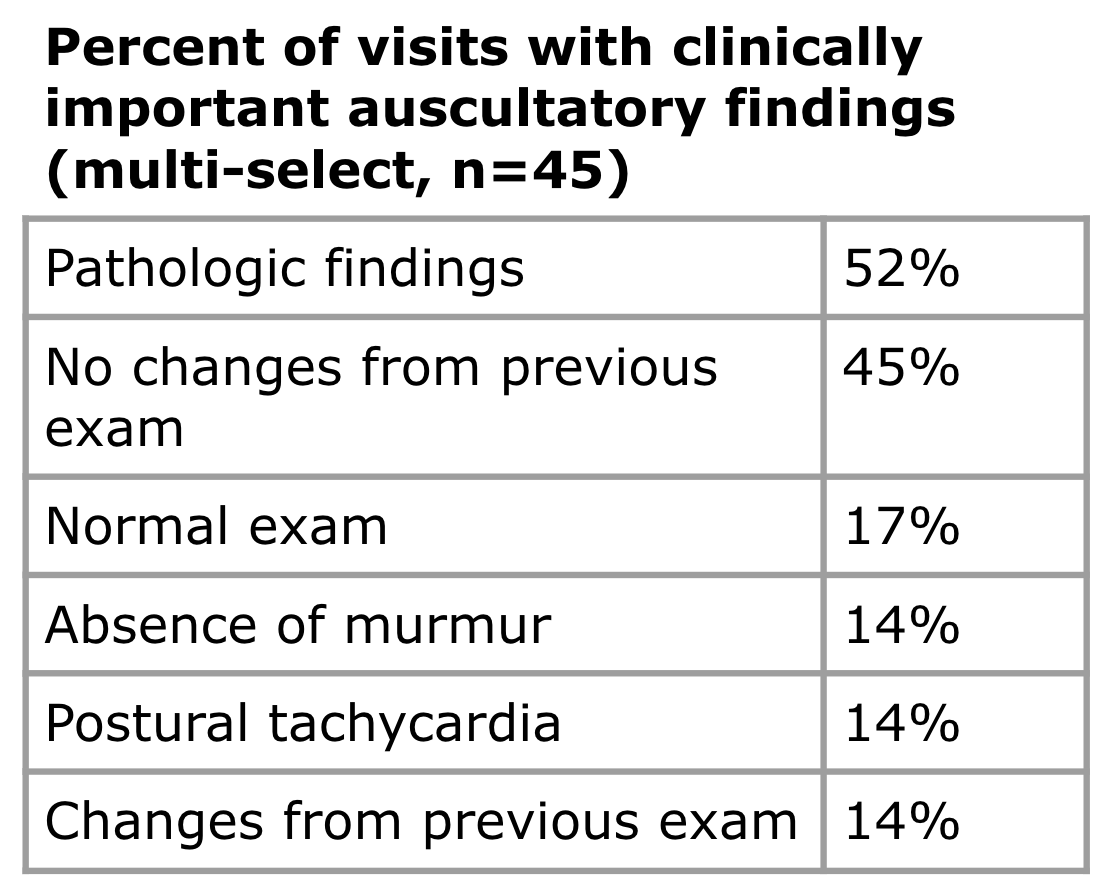 Percentage of visits (n=45) with selected clinically important findings according to cardiologist post visit survey is shown.
Percentage of visits (n=45) with selected clinically important findings according to cardiologist post visit survey is shown.