Neonatal Infectious Diseases/Immunology
Category: Abstract Submission
Neonatal Infectious Diseases/Immunology: COVID-19
289 - Placental Immune Responses Following COVID-19 in Pregnancy Correlate with Infant Cytokines and Timing of Maternal Infection
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 289
Publication Number: 289.226
Publication Number: 289.226
Lillian Juttukonda, Boston Children's Hospital, Boston, MA, United States; Elisha Wachman, Boston Medical Center, Boston, MA, United States; Jeffery O. Boateng, Boston Medical Center, Boston, MA, United States; Yoel Benarroch, Boston University School of Medicine, Boston, MA, United States; Jennifer Snyder-Cappione, Boston University, Boston, MA, United States; Elizabeth Taglauer, Boston University School of Medicine, Boston, MA, United States; Katherine M. Clarke, Boston University School of Medicine, Boston, MA, United States

Lillian Juttukonda, MD, PhD (she/her/hers)
Neonatology Fellow
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: COVID-19 infection continues to impact numerous pregnancies worldwide and is associated with varied perinatal complications. Placental immune responses may help prevent fetal SARS-CoV-2 transmission, but inflammation at the maternal-fetal interface can cause adverse outcomes including preterm labor and altered fetal development. Current understanding of the maternal placental immune response to COVID-19 is limited, particularly for infections earlier in gestation.
Objective: To assess how the timing of maternal SARS-CoV-2 infection in pregnancy impacts placental immune cell and cytokine responses, and to correlate placental immune responses with maternal and infant serum cytokines at delivery.
Design/Methods: Placental tissue, maternal blood, and cord/infant blood were collected from maternal-fetal dyads following pregnancies with symptomatic COVID-19 during the 2nd (2nd Tri COVID, n=8) or 3rd trimester (3rd Tri COVID, n=8) and from SARS-CoV-2-negative controls (Control, n=8). Decidual natural killer (NK) cells, macrophages, and T cells were evaluated using quantitative microscopy, and placental cytokine mRNA expression was evaluated using quantitative reverse transcriptase PCR (qRT-PCR). Serum cytokine levels were quantified by LegendPlex assay.
Results: Compared with Controls, 3rd Tri COVID placentas had significantly increased macrophages, NK cells and T cells, while 2nd Tri COVID only had significantly increased T cells (Figure 1). IL-6, IL-8, IL-10 and TNF- were significantly downregulated in 2nd Tri COVID placentas compared to controls, whereas only IL-8 was significantly changed in 3rd Tri COVID placentas (Figure 2). In correlation analysis between placental immune cells and maternal/infant serum cytokines, the strongest correlations were between placental T cell abundance and infant levels of IL-6, IL-8, and IP-10, as well as maternal IP-10 (Figure 3).Conclusion(s): Maternal 3rd trimester COVID-19 was associated with both innate and adaptive immune cell responses. Maternal 2nd trimester COVID-19 showed evidence of a resolving placental immune response, with cytokine downregulation and normalization of innate immune cells. T cell abundance in the placenta was associated with maternal and infant serum proinflammatory cytokines. Further studies are warranted to characterize the impact of COVID-induced placental inflammation on neonatal outcomes.
Figure 1: Immune cell infiltrates in the placenta vary by timing of maternal COVID-19 infection during pregnancy.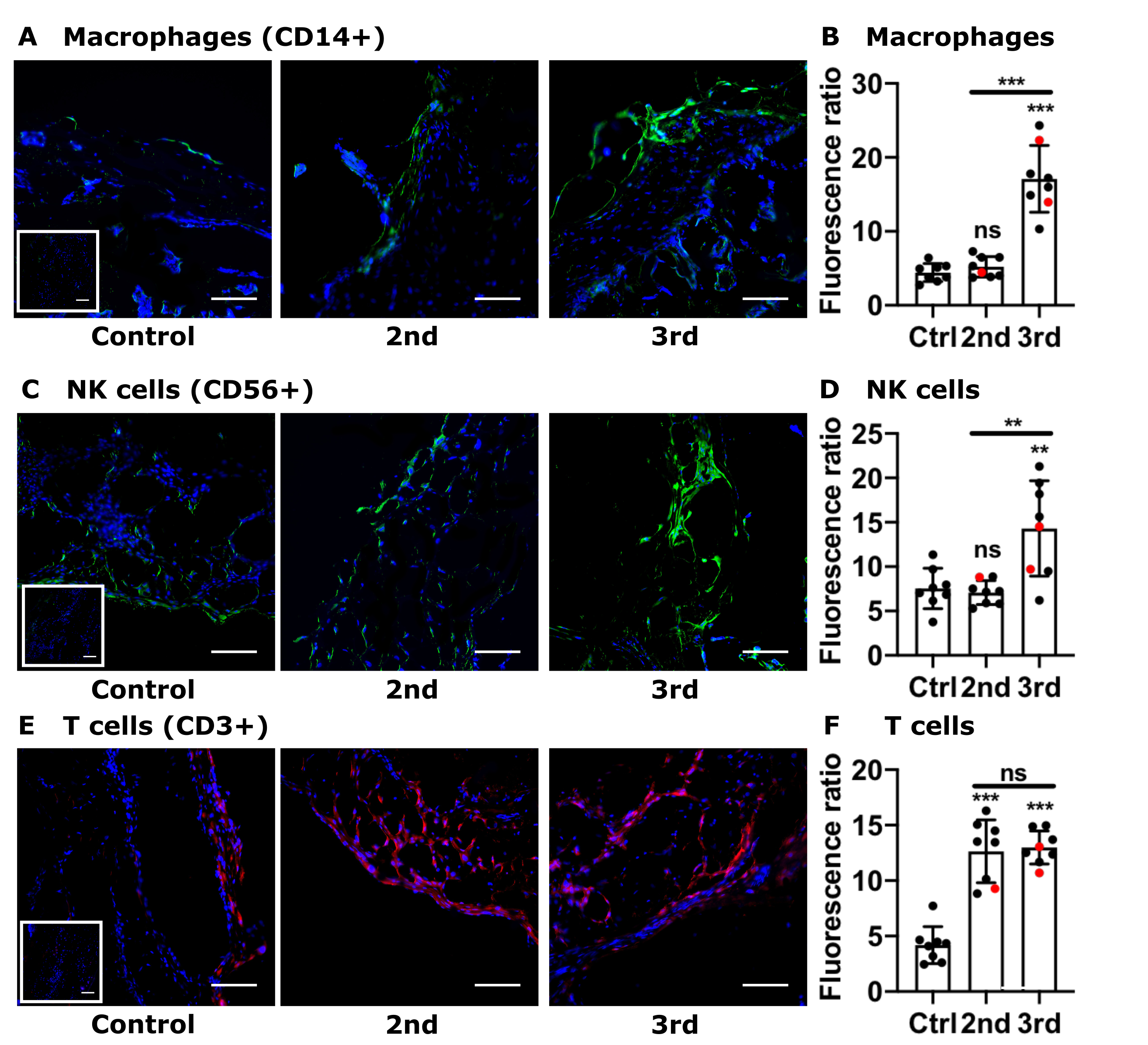 (A, C, E) Representative images (200x) of placental decidual areas stained for (A) CD14 (macrophage marker, green), (C) CD56 (NK cell marker, green), or (E) CD3 (T cell marker, red) immunofluorescence. (B, D, F) Graphical analysis of comparative fluorescence quantitation of (B) macrophages (CD14+), (E) NK cells (CD56+), or (F) T cells (CD3+). Red circles indicate placentas with positive staining for SARS-CoV-2 Spike protein. 2nd = 2nd Trimester COVID (n = 8); 3rd = 3rd Trimester COVID (n = 8); control/ctrl = negative for COVID (n = 8). ns = not significant; ** p < 0.01; ** p < 0.001 by ANOVA. Scale bar: 50µm; insets: secondary-only negative controls.
(A, C, E) Representative images (200x) of placental decidual areas stained for (A) CD14 (macrophage marker, green), (C) CD56 (NK cell marker, green), or (E) CD3 (T cell marker, red) immunofluorescence. (B, D, F) Graphical analysis of comparative fluorescence quantitation of (B) macrophages (CD14+), (E) NK cells (CD56+), or (F) T cells (CD3+). Red circles indicate placentas with positive staining for SARS-CoV-2 Spike protein. 2nd = 2nd Trimester COVID (n = 8); 3rd = 3rd Trimester COVID (n = 8); control/ctrl = negative for COVID (n = 8). ns = not significant; ** p < 0.01; ** p < 0.001 by ANOVA. Scale bar: 50µm; insets: secondary-only negative controls.
Figure 2: Placental cytokine expression varies by timing of maternal infection.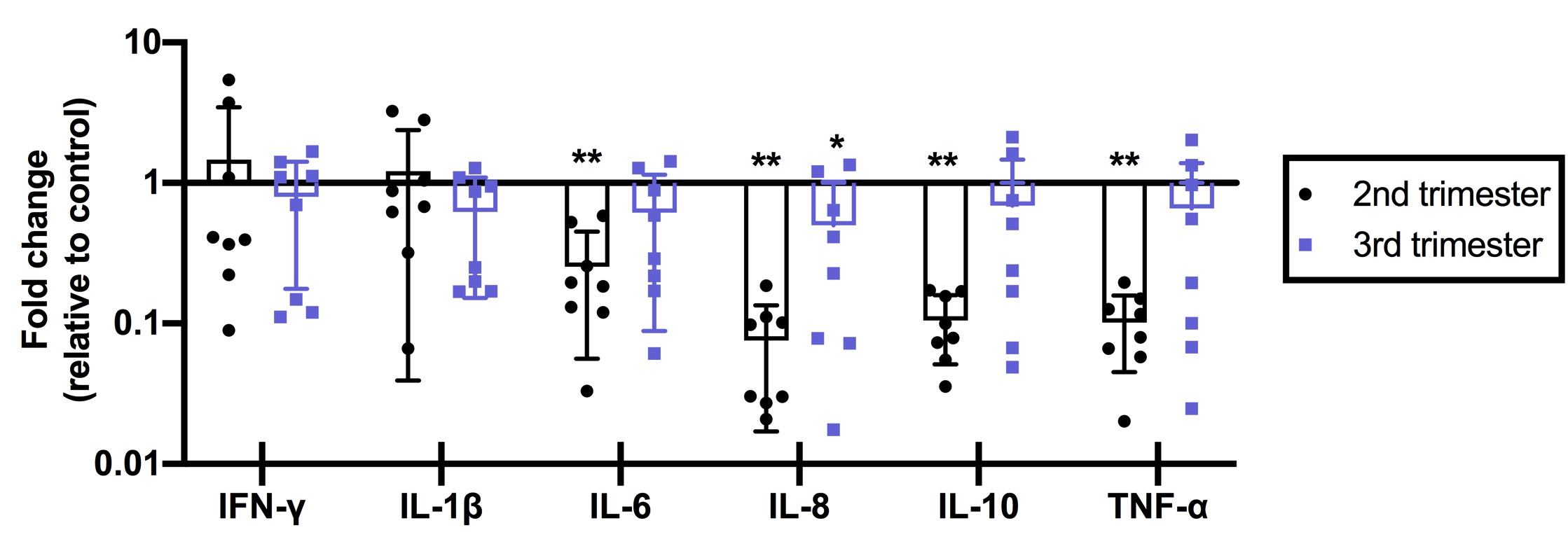 Fold-changes in cytokine abundance for IFN-, IL-1, IL-6, IL-8, IL-10, and TNF- by qRT-PCR of placental tissues from women with 2nd or 3nd trimester COVID infection (n = 8/group) calculated as fold-change compared to control (n = 8). ** p < 0.01; * p < 0.05.
Fold-changes in cytokine abundance for IFN-, IL-1, IL-6, IL-8, IL-10, and TNF- by qRT-PCR of placental tissues from women with 2nd or 3nd trimester COVID infection (n = 8/group) calculated as fold-change compared to control (n = 8). ** p < 0.01; * p < 0.05.
Objective: To assess how the timing of maternal SARS-CoV-2 infection in pregnancy impacts placental immune cell and cytokine responses, and to correlate placental immune responses with maternal and infant serum cytokines at delivery.
Design/Methods: Placental tissue, maternal blood, and cord/infant blood were collected from maternal-fetal dyads following pregnancies with symptomatic COVID-19 during the 2nd (2nd Tri COVID, n=8) or 3rd trimester (3rd Tri COVID, n=8) and from SARS-CoV-2-negative controls (Control, n=8). Decidual natural killer (NK) cells, macrophages, and T cells were evaluated using quantitative microscopy, and placental cytokine mRNA expression was evaluated using quantitative reverse transcriptase PCR (qRT-PCR). Serum cytokine levels were quantified by LegendPlex assay.
Results: Compared with Controls, 3rd Tri COVID placentas had significantly increased macrophages, NK cells and T cells, while 2nd Tri COVID only had significantly increased T cells (Figure 1). IL-6, IL-8, IL-10 and TNF- were significantly downregulated in 2nd Tri COVID placentas compared to controls, whereas only IL-8 was significantly changed in 3rd Tri COVID placentas (Figure 2). In correlation analysis between placental immune cells and maternal/infant serum cytokines, the strongest correlations were between placental T cell abundance and infant levels of IL-6, IL-8, and IP-10, as well as maternal IP-10 (Figure 3).Conclusion(s): Maternal 3rd trimester COVID-19 was associated with both innate and adaptive immune cell responses. Maternal 2nd trimester COVID-19 showed evidence of a resolving placental immune response, with cytokine downregulation and normalization of innate immune cells. T cell abundance in the placenta was associated with maternal and infant serum proinflammatory cytokines. Further studies are warranted to characterize the impact of COVID-induced placental inflammation on neonatal outcomes.
Figure 1: Immune cell infiltrates in the placenta vary by timing of maternal COVID-19 infection during pregnancy.
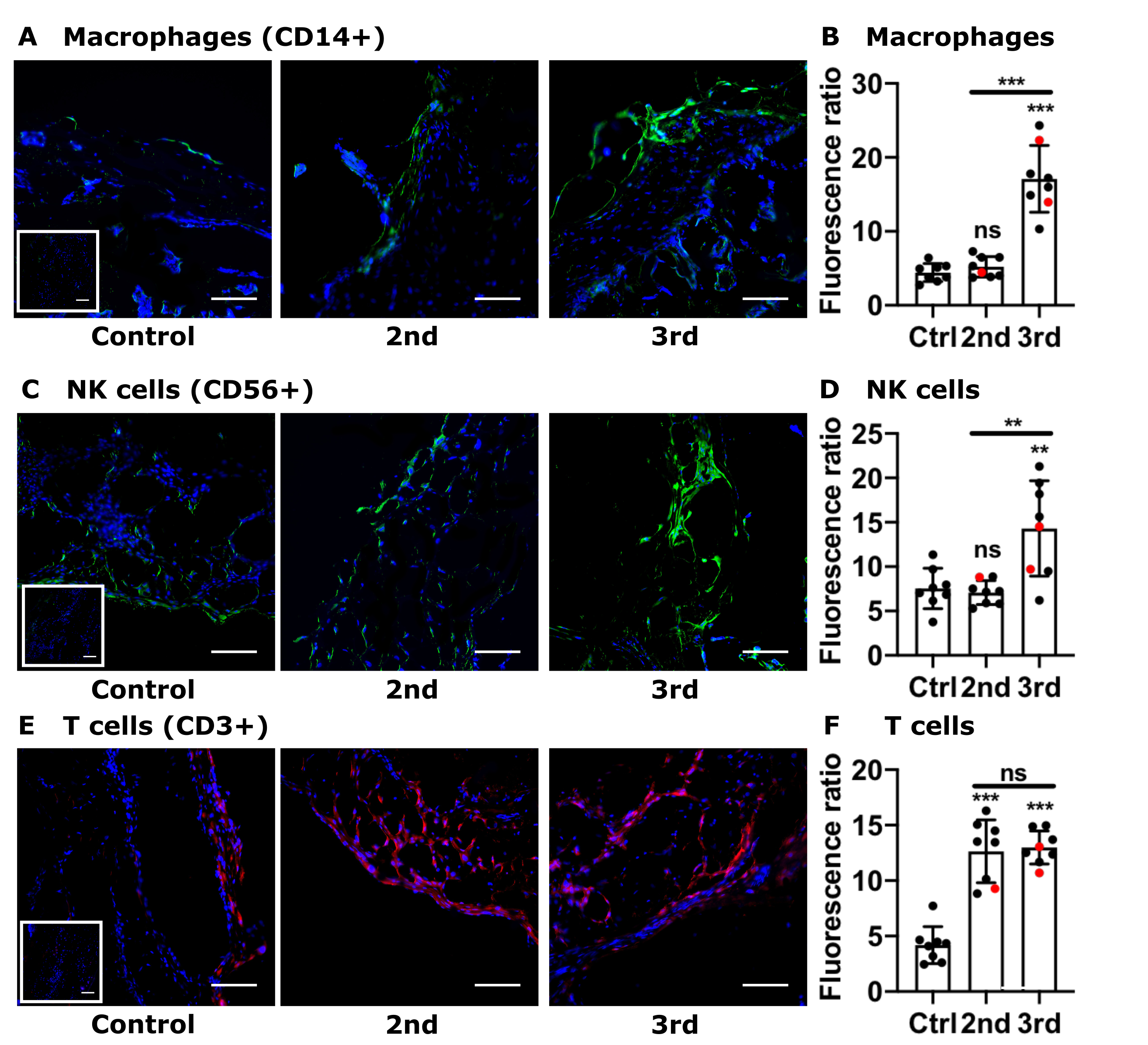 (A, C, E) Representative images (200x) of placental decidual areas stained for (A) CD14 (macrophage marker, green), (C) CD56 (NK cell marker, green), or (E) CD3 (T cell marker, red) immunofluorescence. (B, D, F) Graphical analysis of comparative fluorescence quantitation of (B) macrophages (CD14+), (E) NK cells (CD56+), or (F) T cells (CD3+). Red circles indicate placentas with positive staining for SARS-CoV-2 Spike protein. 2nd = 2nd Trimester COVID (n = 8); 3rd = 3rd Trimester COVID (n = 8); control/ctrl = negative for COVID (n = 8). ns = not significant; ** p < 0.01; ** p < 0.001 by ANOVA. Scale bar: 50µm; insets: secondary-only negative controls.
(A, C, E) Representative images (200x) of placental decidual areas stained for (A) CD14 (macrophage marker, green), (C) CD56 (NK cell marker, green), or (E) CD3 (T cell marker, red) immunofluorescence. (B, D, F) Graphical analysis of comparative fluorescence quantitation of (B) macrophages (CD14+), (E) NK cells (CD56+), or (F) T cells (CD3+). Red circles indicate placentas with positive staining for SARS-CoV-2 Spike protein. 2nd = 2nd Trimester COVID (n = 8); 3rd = 3rd Trimester COVID (n = 8); control/ctrl = negative for COVID (n = 8). ns = not significant; ** p < 0.01; ** p < 0.001 by ANOVA. Scale bar: 50µm; insets: secondary-only negative controls.Figure 2: Placental cytokine expression varies by timing of maternal infection.
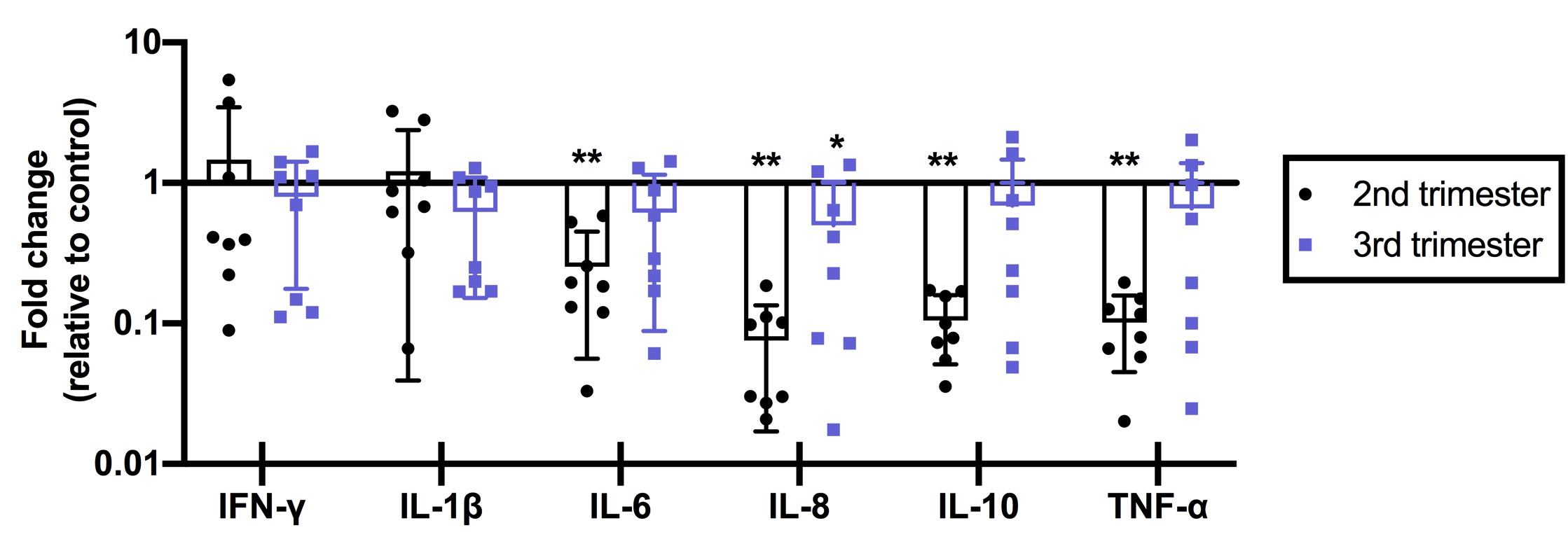 Fold-changes in cytokine abundance for IFN-, IL-1, IL-6, IL-8, IL-10, and TNF- by qRT-PCR of placental tissues from women with 2nd or 3nd trimester COVID infection (n = 8/group) calculated as fold-change compared to control (n = 8). ** p < 0.01; * p < 0.05.
Fold-changes in cytokine abundance for IFN-, IL-1, IL-6, IL-8, IL-10, and TNF- by qRT-PCR of placental tissues from women with 2nd or 3nd trimester COVID infection (n = 8/group) calculated as fold-change compared to control (n = 8). ** p < 0.01; * p < 0.05.