Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up II
257 - Placental lesions and referral for early developmental delay
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 257
Publication Number: 257.224
Publication Number: 257.224
Victoria Tan, NorthShore University Health Systems, Chicago, IL, United States; Andrew Franklin, Northshore university healthsysten, Evanston, IL, United States; Matthew Pellerite, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Chicago, IL, United States; Alexa Freedman, Northwestern University, Evanston, IL, United States; Gregory E. Miller, Northwestern University, Evanston, IL, United States; Ann Borders, Northshore University HealthSystem, Evanston, IL, United States; Adriana Weisleder, Northwestern University, Evanston, IL, United States; Linda M. Ernst, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Evanston, IL, United States

Victoria Tan, B.A.
Research Assistant
NorthShore University Health Systems
Chicago, Illinois, United States
Presenting Author(s)
Background: An adverse in-utero environment has been associated with neurodevelopmental impairment, and placental inflammatory or vascular lesions may play a role in the underlying mechanism of these impairments. Abnormal placental pathology has been associated with major developmental impairments including cerebral palsy, autism spectrum disorder, and schizophrenia. However, there remains a gap in understanding the link between placental pathology and more prevalent neurodevelopmental delays in early childhood.
Objective: We aim to examine the impact of abnormal placental histopathology (inflammation and vascular malperfusion) on neurodevelopmental delays by examining its links with referral to early intervention (EI).
Design/Methods: This study utilized an ongoing prospective cohort from a suburban Chicago hospital from 2017 to present. At delivery, placentas were collected and evaluated by an experienced placental pathologist. These were classified using the Amsterdam criteria using 4 major domains of placental pathology (acute inflammation, chronic inflammation, fetal vascular pathology (FVM), and maternal vascular malperfusion (MVM)). Placental lesions were further classified as none, low, and high grade based on previous publications from this group. Infant referral to EI and reason for referral through age 3 were collected from medical records using the Enterprise Data Warehouse. Data were analyzed using chi-squared tests.
Results: 339 children were included. Forty-nine of those (14.5%) were referred to EI for developmental delay before age three (see table 1). Higher rates of speech-language delay were observed in children exposed to high-grade placental MVM vs those not exposed (16.6% vs 7.6%; p=0.04) and in those with any high-grade vascular pathology (FVM or MVM; 15.1% vs 7.1%; p=0.035) vs those without these pathologies. Conclusion(s): We show that exposure to in-utero placental vascular malperfusion is associated with increased referral to EI by age 3, specifically for speech-language delay. Identifying infants who are at early risk for language delay may help improve access to therapies. Further understanding of the underlying mechanisms in placental vascular malperfusion may help to target interventions and therapies for pregnant persons and neonates.
Developmental Delays by High Grade Placental Pathology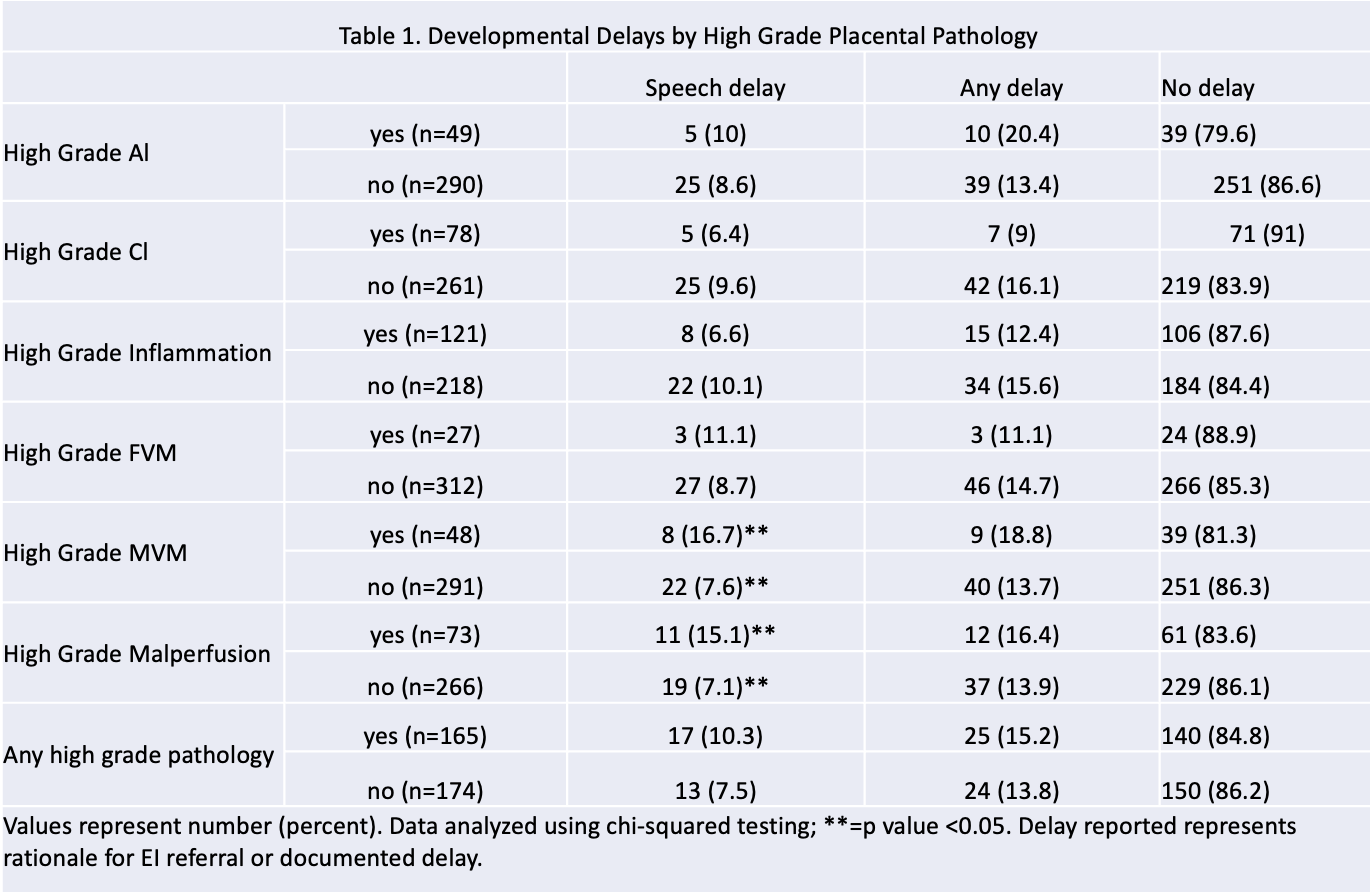 Table 1. Infant referral to EI and reason for referral through age 3 categorized by the Amsterdam criteria using four major domains of placental pathology.
Table 1. Infant referral to EI and reason for referral through age 3 categorized by the Amsterdam criteria using four major domains of placental pathology.
Objective: We aim to examine the impact of abnormal placental histopathology (inflammation and vascular malperfusion) on neurodevelopmental delays by examining its links with referral to early intervention (EI).
Design/Methods: This study utilized an ongoing prospective cohort from a suburban Chicago hospital from 2017 to present. At delivery, placentas were collected and evaluated by an experienced placental pathologist. These were classified using the Amsterdam criteria using 4 major domains of placental pathology (acute inflammation, chronic inflammation, fetal vascular pathology (FVM), and maternal vascular malperfusion (MVM)). Placental lesions were further classified as none, low, and high grade based on previous publications from this group. Infant referral to EI and reason for referral through age 3 were collected from medical records using the Enterprise Data Warehouse. Data were analyzed using chi-squared tests.
Results: 339 children were included. Forty-nine of those (14.5%) were referred to EI for developmental delay before age three (see table 1). Higher rates of speech-language delay were observed in children exposed to high-grade placental MVM vs those not exposed (16.6% vs 7.6%; p=0.04) and in those with any high-grade vascular pathology (FVM or MVM; 15.1% vs 7.1%; p=0.035) vs those without these pathologies. Conclusion(s): We show that exposure to in-utero placental vascular malperfusion is associated with increased referral to EI by age 3, specifically for speech-language delay. Identifying infants who are at early risk for language delay may help improve access to therapies. Further understanding of the underlying mechanisms in placental vascular malperfusion may help to target interventions and therapies for pregnant persons and neonates.
Developmental Delays by High Grade Placental Pathology
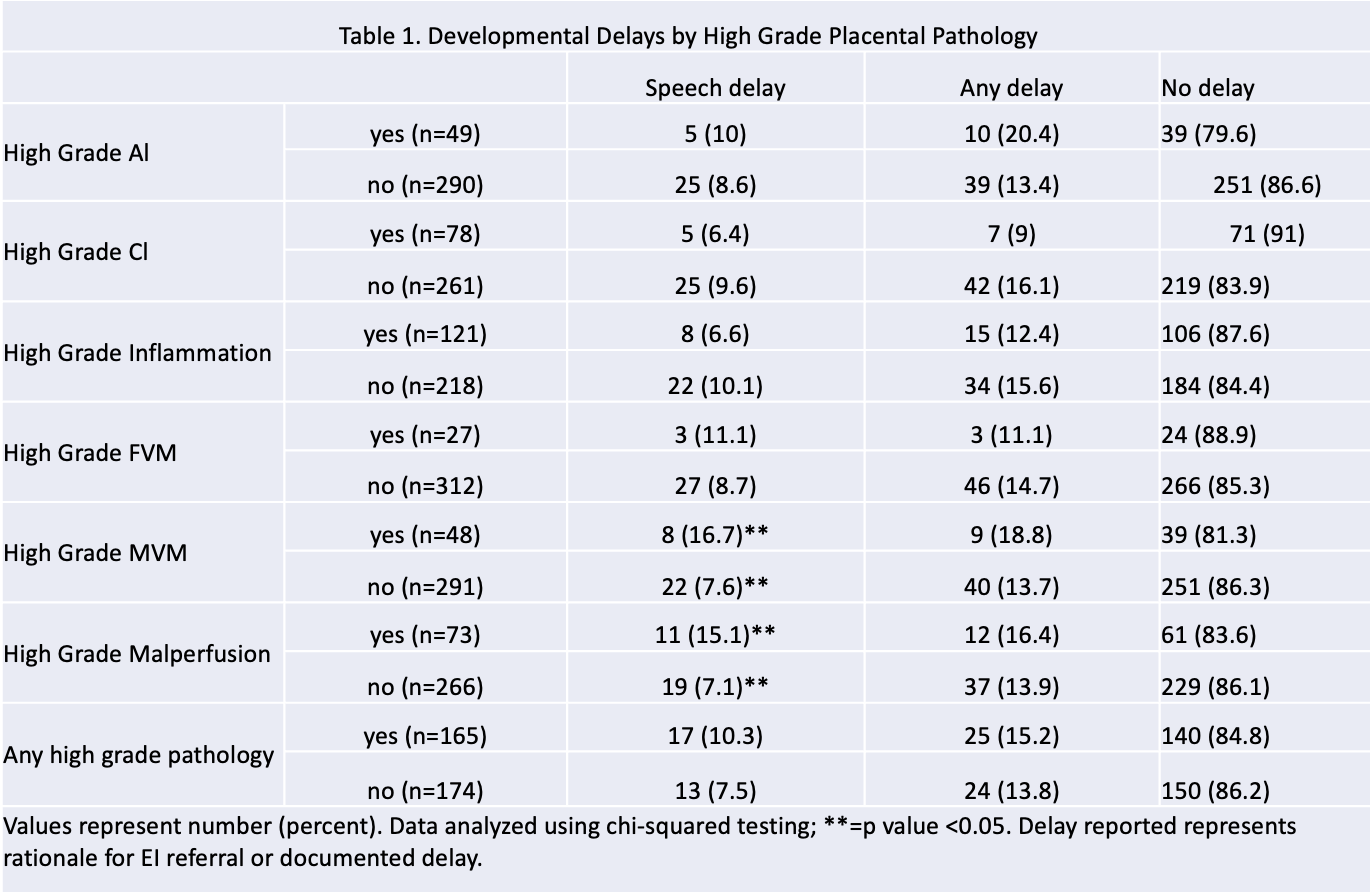 Table 1. Infant referral to EI and reason for referral through age 3 categorized by the Amsterdam criteria using four major domains of placental pathology.
Table 1. Infant referral to EI and reason for referral through age 3 categorized by the Amsterdam criteria using four major domains of placental pathology.