Neonatal/Infant Resuscitation
Category: Abstract Submission
Neonatal/Infant Resuscitation I
473 - Direct Umbilical Vein Epinephrine Injection during Resuscitation with an Intact Cord in Asphyxiated Extremely Preterm Lambs
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 473
Publication Number: 473.230
Publication Number: 473.230
Lida I. Zeinali, University of California, Davis, School of Medicine, Sacramento, CA, United States; Heather Knych, University of California Davis, School of Veterinary Medicine, Davis, CA, United States; Houssam M. Joudi, University of California, Torrance, CA, United States; Amy Lesneski, University of California, Davis, School of Medicine, Davis, CA, United States; Evan Giusto, University of California Davis Children's Hospital, Sacramento, CA, United States; Deepika Sankaran, University of California Davis Children's Hospital, Sacramento, CA, United States; Satyan Lakshminrusimha, University of California Davis Children's Hospital, Sacramento, CA, United States; Payam Vali, University of California Davis Children's Hospital, Sacramento, CA, United States
- LZ
Lida I. Zeinali, MD
Neonatal-Perinatal Fellow
University of California, Davis, School of Medicine
Sacramento, California, United States
Presenting Author(s)
Background: Extremely preterm infants are more likely to have cardiorespiratory compromise leading to immediate cord clamping (ICC) with a greater incidence of epinephrine (EPI) use in the delivery room compared to term infants. Delayed umbilical cord clamping (DCC) during positive pressure ventilation (PPV) stabilizes left ventricular preload and cerebral blood flow but delays umbilical venous access. EPI administration directly into the umbilical vein (UV) during DCC in severely bradycardic newborns potentially combines the hemodynamic benefits of DCC and hastens EPI delivery.
Objective: Direct UV EPI injection during DCC (DCC+direct-EPI) before chest compressions (CC) has quicker return of spontaneous circulation (ROSC) compared to ICC and EPI administered through a UV catheter (UVC; ICC+cath-EPI). ROSC defined as HR >100/min.
Design/Methods: Ten extremely preterm lambs (125-128d gestation) were exteriorized, intubated, and instrumented prior to cord occlusion to induce asphyxia and fetal bradycardia (heart rate, HR < 30/min). Lambs were randomized to ICC+cath-EPI (control) or DCC+direct-EPI (intervention). In the ICC+cath-EPI group, the cord was clamped and the lamb was resuscitated following neonatal resuscitation program (NRP) guidelines. After 30s of PPV, CC were initiated if the HR was < 60/min. EPI (0.02 mg/kg) was administered once a UVC was placed (repeated every 3 min until ROSC or for a maximum of 3 doses). In the DCC+direct-EPI group, cord occlusion was released and PPV was initiated. If HR remained < 60/min, EPI was injected directly into the UV using a 24G needle. If ROSC was achieved, DCC was continued for a total of 2 min. If HR remained < 100/min, the umbilical cord was clamped and the lamb was delivered to continue resuscitation per NRP.
Results: Time to first EPI administration was shorter with DCC+direct-EPI (Table 1). All lambs (4/4) in the ICC+cath-EPI group and 2/6 lambs in the DCC+direct-EPI group received CC (p=0.07). ROSC was achieved in 3/4 in the control and 6/6 in the intervention group and time to ROSC was not different. All lambs received EPI, and one lamb in each group got >1 EPI. There was no significant difference in carotid blood flow, oxygen delivery or EPI plasma concentrations. Post-ROSC tachycardia and hypertension were more common in ICC+cath-EPI group.Conclusion(s): In the severely bradycardic perinatal asphyxiated preterm lamb, EPI injection directly into the UV during DCC is feasible and results in quicker EPI administration during resuscitation and may reduce the need for CC. A larger sample size and further studies are needed before consideration for clinical trials.
CV LZCV LZ.pdf
Lamb Characteristics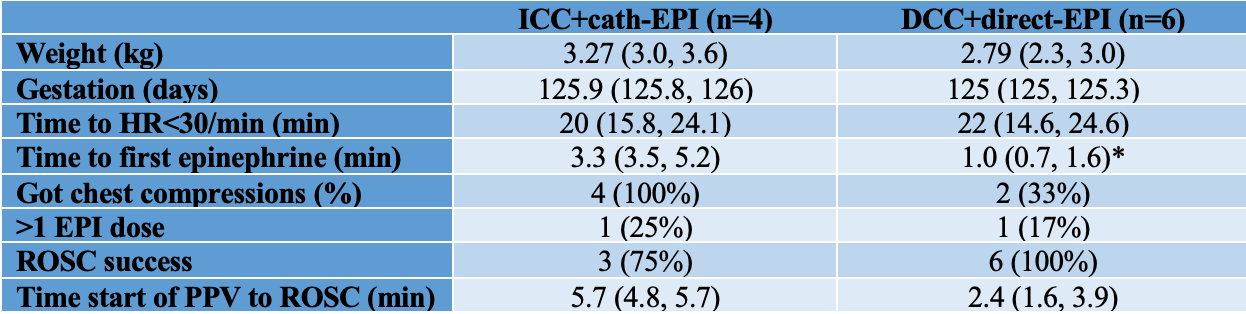 Table 1. Values represented as median (IQR). ROSC = return of spontaneous circulation. *p-value < 0.05
Table 1. Values represented as median (IQR). ROSC = return of spontaneous circulation. *p-value < 0.05
Objective: Direct UV EPI injection during DCC (DCC+direct-EPI) before chest compressions (CC) has quicker return of spontaneous circulation (ROSC) compared to ICC and EPI administered through a UV catheter (UVC; ICC+cath-EPI). ROSC defined as HR >100/min.
Design/Methods: Ten extremely preterm lambs (125-128d gestation) were exteriorized, intubated, and instrumented prior to cord occlusion to induce asphyxia and fetal bradycardia (heart rate, HR < 30/min). Lambs were randomized to ICC+cath-EPI (control) or DCC+direct-EPI (intervention). In the ICC+cath-EPI group, the cord was clamped and the lamb was resuscitated following neonatal resuscitation program (NRP) guidelines. After 30s of PPV, CC were initiated if the HR was < 60/min. EPI (0.02 mg/kg) was administered once a UVC was placed (repeated every 3 min until ROSC or for a maximum of 3 doses). In the DCC+direct-EPI group, cord occlusion was released and PPV was initiated. If HR remained < 60/min, EPI was injected directly into the UV using a 24G needle. If ROSC was achieved, DCC was continued for a total of 2 min. If HR remained < 100/min, the umbilical cord was clamped and the lamb was delivered to continue resuscitation per NRP.
Results: Time to first EPI administration was shorter with DCC+direct-EPI (Table 1). All lambs (4/4) in the ICC+cath-EPI group and 2/6 lambs in the DCC+direct-EPI group received CC (p=0.07). ROSC was achieved in 3/4 in the control and 6/6 in the intervention group and time to ROSC was not different. All lambs received EPI, and one lamb in each group got >1 EPI. There was no significant difference in carotid blood flow, oxygen delivery or EPI plasma concentrations. Post-ROSC tachycardia and hypertension were more common in ICC+cath-EPI group.Conclusion(s): In the severely bradycardic perinatal asphyxiated preterm lamb, EPI injection directly into the UV during DCC is feasible and results in quicker EPI administration during resuscitation and may reduce the need for CC. A larger sample size and further studies are needed before consideration for clinical trials.
CV LZCV LZ.pdf
Lamb Characteristics
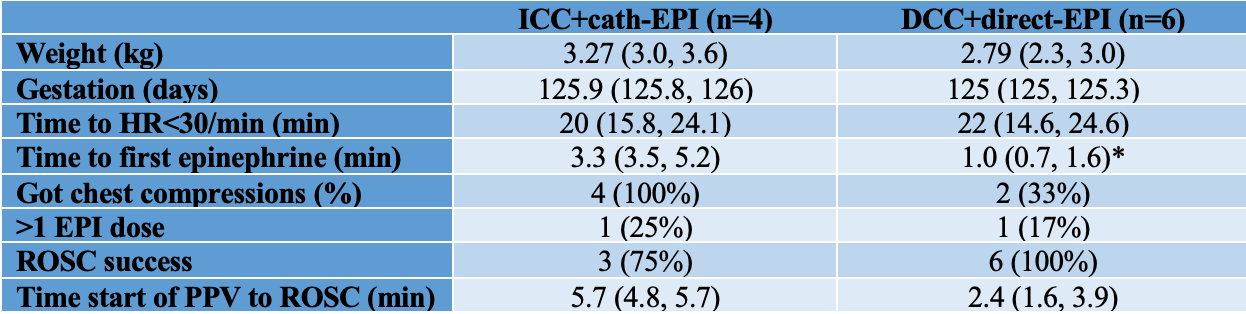 Table 1. Values represented as median (IQR). ROSC = return of spontaneous circulation. *p-value < 0.05
Table 1. Values represented as median (IQR). ROSC = return of spontaneous circulation. *p-value < 0.05