Hospital Medicine: Clinical
Category: Abstract Submission
Hospital Medicine: Clinical NOS
323 - Does Self-Reported Pain scores Correlate With Vital Signs?
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 323
Publication Number: 323.214
Publication Number: 323.214
Maggie R. Donovan, University of Arizona College of Medicine - Phoenix, SCOTTSDALE, AZ, United States; Sandra Gage, University of Arizona College of Medicine - Phoenix, Phoenix, AZ, United States; Charlotte Bolch, Midwestern University, Glendale, AZ, United States; Maheshwor Kafle, Phoenix Children's Hospital, Phoenix, AZ, United States
Maheshwor Kafle, MD
Attending Hospitalist
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background: Migraine headaches (MHA) are common in children, with severe MHA leading to hospitalization. For children hospitalized with MHA, therapy is often directed by subjective descriptors like self-reported pain scores. While these have been shown to have some validity in children older than 6 years (1–4), additional assessment tools would be helpful in directing complex medical regimens required in MHA treatment. Sympathetic response to pain is known to elevate heart rate (HR) and blood pressure (BP); however limited studies have assessed the value of vital signs as an objective tool for pediatric pain assessment.
Objective: The objective of this study was to determine if the self-reported pain severity of MHAs in children correlates with fluctuations of HR, systolic BP (SBP), and/or diastolic BP (DBP), providing an objective means of confirming pain severity.
Design/Methods:
Retrospective chart review was conducted on patients age 6–18 years admitted to a children’s hospital between 2010 and 2018 with a primary discharge diagnosis of MHA. Patients with an infectious process or complex care needs were excluded. Associated HR, SBP, and DBP were collected within 1 hour of self-reported pain scores. To account for the differences in vital signs related to age and other individual factors, we assessed the variation in vital signs related to the highest and lowest pain scores separately for each individual. Cumulative results from this data were then analyzed using Pearson’s correlation test. Descriptive statistics (percentages and means) were calculated for population characteristics
Results:
A total of 1,201 patients met inclusion criteria for the study. These patients were predominantly female (76.9%), non-Hispanic ethnicity (76.7 %), and white race (90.9%), with a mean age of 14.1 years. The correlation between pain scores and all vital signs analyzed was weak, lacking statistical significance( Figures 1 and 2) ; change in HR and change in pain score r = 0.0166, P=0.5686; change in SBP and pain scores r = 0.0337, P=0.3417; change in DBP and pain scores r = -0.0324, P=0.3597.
Conclusion(s):
In this individually adjusted analysis, no significant association was found between changes in self-reported pain score and corresponding heart rate, systolic BP, or diastolic BP. This indicates that while fluctuations in vital signs, when identified, may provide additional information to guide therapy, vital signs are not a reliable determinant of subjective pain in children with migraine headaches.
Figure 1. Scatterplot for change in pain score versus associated change in heart rate (HR).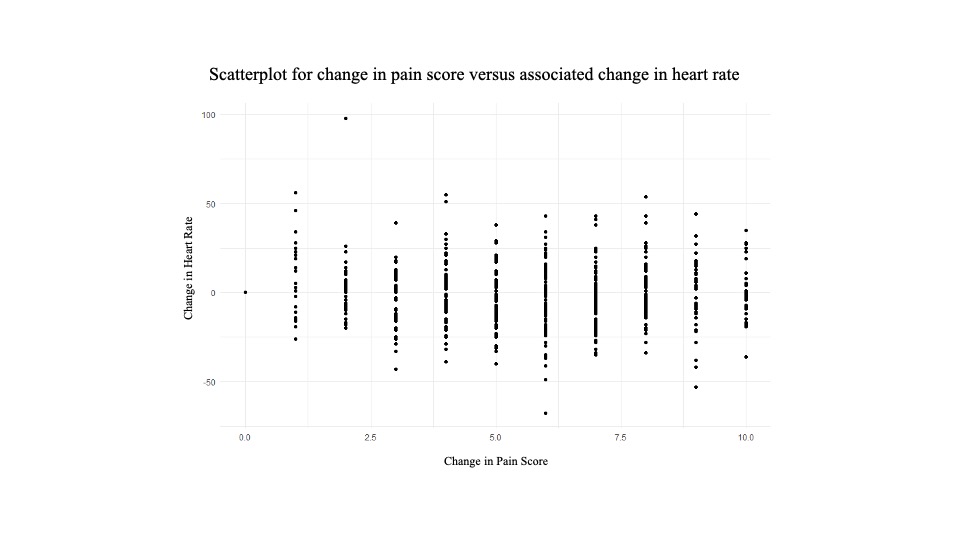 Each point represents an individual patient. Highest and lowest pain score values (among ten total recorded values) for each patient were used to calculate the change in pain score. Associated HRs within one-hour of these pain score values were used to calculate the corresponding change in HR.
Each point represents an individual patient. Highest and lowest pain score values (among ten total recorded values) for each patient were used to calculate the change in pain score. Associated HRs within one-hour of these pain score values were used to calculate the corresponding change in HR.
Figure 2. Scatterplots for change in pain score versus associated changes in systolic (SBP, left plot) and diastolic blood pressure (DBP, right plot)..jpg) Each point represents an individual patient. Highest and lowest pain score values (among ten total recorded values) for each patient were used to calculate the change in pain score. Associated SBPs and DBPs within one-hour of these pain score values were used to calculate the corresponding changes in blood pressure.
Each point represents an individual patient. Highest and lowest pain score values (among ten total recorded values) for each patient were used to calculate the change in pain score. Associated SBPs and DBPs within one-hour of these pain score values were used to calculate the corresponding changes in blood pressure.
Objective: The objective of this study was to determine if the self-reported pain severity of MHAs in children correlates with fluctuations of HR, systolic BP (SBP), and/or diastolic BP (DBP), providing an objective means of confirming pain severity.
Design/Methods:
Retrospective chart review was conducted on patients age 6–18 years admitted to a children’s hospital between 2010 and 2018 with a primary discharge diagnosis of MHA. Patients with an infectious process or complex care needs were excluded. Associated HR, SBP, and DBP were collected within 1 hour of self-reported pain scores. To account for the differences in vital signs related to age and other individual factors, we assessed the variation in vital signs related to the highest and lowest pain scores separately for each individual. Cumulative results from this data were then analyzed using Pearson’s correlation test. Descriptive statistics (percentages and means) were calculated for population characteristics
Results:
A total of 1,201 patients met inclusion criteria for the study. These patients were predominantly female (76.9%), non-Hispanic ethnicity (76.7 %), and white race (90.9%), with a mean age of 14.1 years. The correlation between pain scores and all vital signs analyzed was weak, lacking statistical significance( Figures 1 and 2) ; change in HR and change in pain score r = 0.0166, P=0.5686; change in SBP and pain scores r = 0.0337, P=0.3417; change in DBP and pain scores r = -0.0324, P=0.3597.
Conclusion(s):
In this individually adjusted analysis, no significant association was found between changes in self-reported pain score and corresponding heart rate, systolic BP, or diastolic BP. This indicates that while fluctuations in vital signs, when identified, may provide additional information to guide therapy, vital signs are not a reliable determinant of subjective pain in children with migraine headaches.
Figure 1. Scatterplot for change in pain score versus associated change in heart rate (HR).
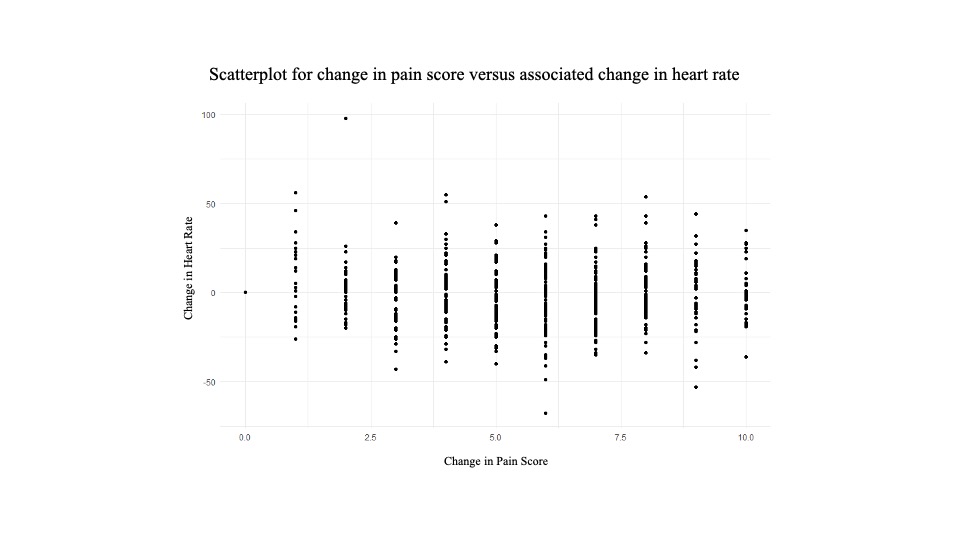 Each point represents an individual patient. Highest and lowest pain score values (among ten total recorded values) for each patient were used to calculate the change in pain score. Associated HRs within one-hour of these pain score values were used to calculate the corresponding change in HR.
Each point represents an individual patient. Highest and lowest pain score values (among ten total recorded values) for each patient were used to calculate the change in pain score. Associated HRs within one-hour of these pain score values were used to calculate the corresponding change in HR.Figure 2. Scatterplots for change in pain score versus associated changes in systolic (SBP, left plot) and diastolic blood pressure (DBP, right plot).
.jpg) Each point represents an individual patient. Highest and lowest pain score values (among ten total recorded values) for each patient were used to calculate the change in pain score. Associated SBPs and DBPs within one-hour of these pain score values were used to calculate the corresponding changes in blood pressure.
Each point represents an individual patient. Highest and lowest pain score values (among ten total recorded values) for each patient were used to calculate the change in pain score. Associated SBPs and DBPs within one-hour of these pain score values were used to calculate the corresponding changes in blood pressure.