Children with Chronic Conditions
Category: Abstract Submission
Children with Chronic Conditions IV
609 - Improving After Visit Communication in a Pediatric Multidisciplinary Neuromuscular Care Program
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 609
Publication Number: 609.404
Publication Number: 609.404
Elaine Lin, Icahn School of Medicine at Mount Sinai, Jersey City, NJ, United States; Skylar M. Hess, Icahn School of Medicine at Mount Sinai, New York, NY, United States; Brijen J. Shah, Mount Sinai Health System and Icahn School of Medicine at Mount Sinai, New York, NY, United States; Sheena Ranade, Mount Sinai Health System, New York, NY, United States; Robert W. Fields, Icahn School of Medicine at Mount Sinai, Larchmont, NY, United States; Cordelia R. Elaiho, Icahn School of Medicine at Mount Sinai, New York, NY, United States; Liam R. Butler, Icahn School of Medicine at Mount Sinai, New York, NY, United States; Kristin Shadman, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States
- EL
Elaine Lin, MD
Associate Professor of Pediatrics
Icahn School of Medicine at Mount Sinai
New York, New York, United States
Presenting Author(s)
Background: Multidisciplinary care team visits are an essential part of coordinated care for children with cerebral palsy and neuromuscular disorders. After visit summaries (AVS) from all specialty providers are critical in communication to families for care coordination and shared care planning.
Objective: Improve completion rate and quality of AVS for each subspecialty encounter of a pediatric multidisciplinary neuromuscular clinic.
Design/Methods: Our urban academic tertiary care institution’s comprehensive neuromuscular care program meets twice monthly and includes: orthopedics, neurology, pulmonology, nutrition, neurosurgery, endocrinology, urology, rehabilitation medicine, dentistry, and primary care. Each patient sees multiple providers per visit. A multidisciplinary stakeholder team noted large variation in completion and content of AVS in our collaborative visit. Using quality improvement methodology, our stakeholder team defined best practice as completion of AVS by all providers for each patient. The previously validated Family Experiences of Care Coordination (FECC) was chosen as a measure of quality care coordination for this population of children with medical complexity. A key driver diagram was constructed (Figure 1.) Plan-Do-Study-Act (PDSA) cycles included 1) creation of a smartphrase for use in the AVS to standardize information 2) review of critical elements of the AVS with providers at each clinic day. Process measures included AVS completion by all providers at a visit and selected quality indicators of the FECC (including follow-up plan and provider contact information). Data were tracked via run charts.
Results: Median of a 6 month baseline period of completed AVS (n= 29 patients) was 38.5% (Figure 2). After the initial intervention, median increased to 81% (n=40 patients). Inclusion of the follow up plan increased from 0 to 50% (Figure 3) during PDSA cycles. Inclusion of contact information for at least one provider also demonstrated improvement by 35% over a 6 month period.Conclusion(s): Implementation of a template summary was associated with improved completion and quality of AVS in a multidisciplinary neuromuscular clinic. Further efforts to understand patient-centered outcomes regarding our team’s communication are ongoing through FECC survey of participating families.
Figure 1. Key Driver Diagram.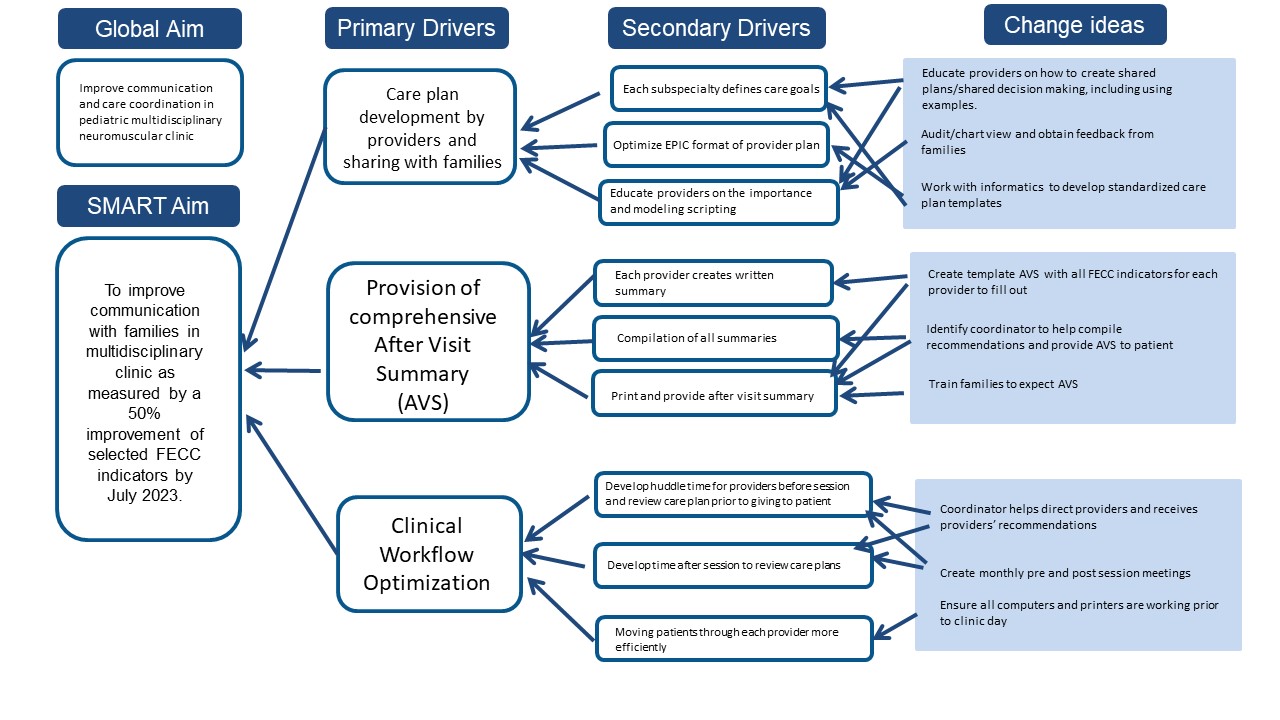
Figure 2. Run Chart of AVS completion.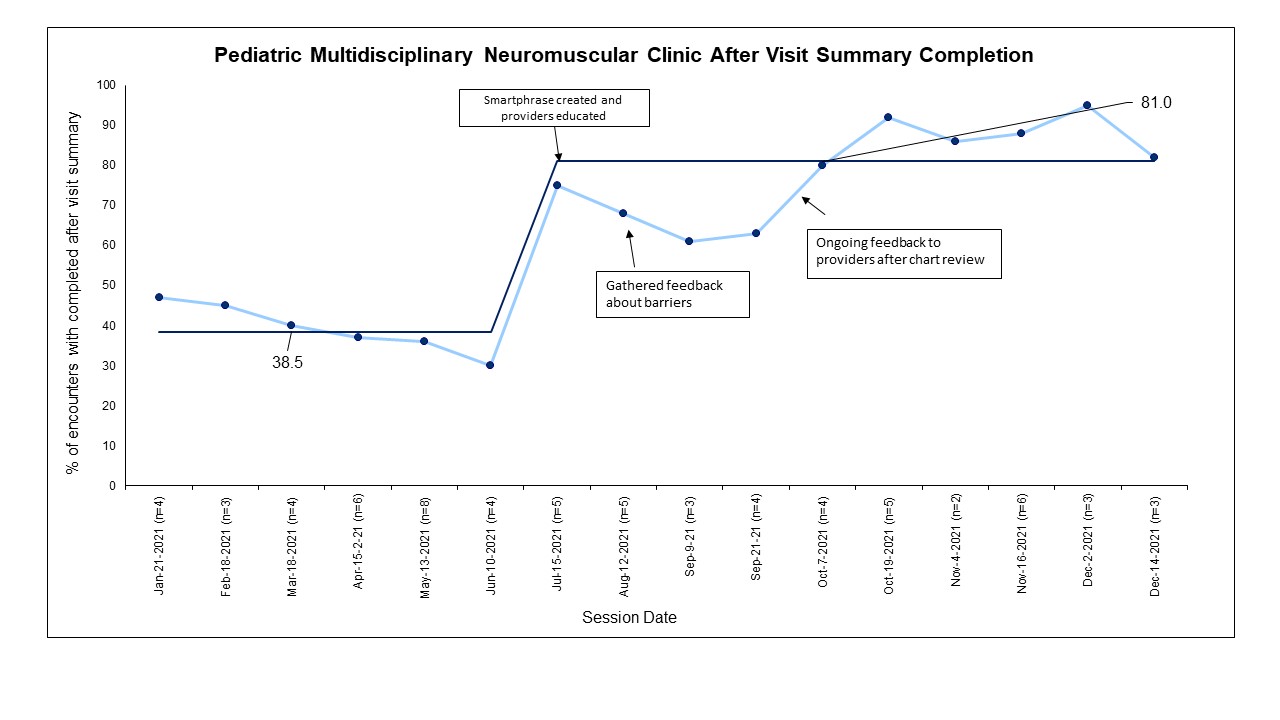 Medians are labeled for PDSA cycles.
Medians are labeled for PDSA cycles.
Objective: Improve completion rate and quality of AVS for each subspecialty encounter of a pediatric multidisciplinary neuromuscular clinic.
Design/Methods: Our urban academic tertiary care institution’s comprehensive neuromuscular care program meets twice monthly and includes: orthopedics, neurology, pulmonology, nutrition, neurosurgery, endocrinology, urology, rehabilitation medicine, dentistry, and primary care. Each patient sees multiple providers per visit. A multidisciplinary stakeholder team noted large variation in completion and content of AVS in our collaborative visit. Using quality improvement methodology, our stakeholder team defined best practice as completion of AVS by all providers for each patient. The previously validated Family Experiences of Care Coordination (FECC) was chosen as a measure of quality care coordination for this population of children with medical complexity. A key driver diagram was constructed (Figure 1.) Plan-Do-Study-Act (PDSA) cycles included 1) creation of a smartphrase for use in the AVS to standardize information 2) review of critical elements of the AVS with providers at each clinic day. Process measures included AVS completion by all providers at a visit and selected quality indicators of the FECC (including follow-up plan and provider contact information). Data were tracked via run charts.
Results: Median of a 6 month baseline period of completed AVS (n= 29 patients) was 38.5% (Figure 2). After the initial intervention, median increased to 81% (n=40 patients). Inclusion of the follow up plan increased from 0 to 50% (Figure 3) during PDSA cycles. Inclusion of contact information for at least one provider also demonstrated improvement by 35% over a 6 month period.Conclusion(s): Implementation of a template summary was associated with improved completion and quality of AVS in a multidisciplinary neuromuscular clinic. Further efforts to understand patient-centered outcomes regarding our team’s communication are ongoing through FECC survey of participating families.
Figure 1. Key Driver Diagram.
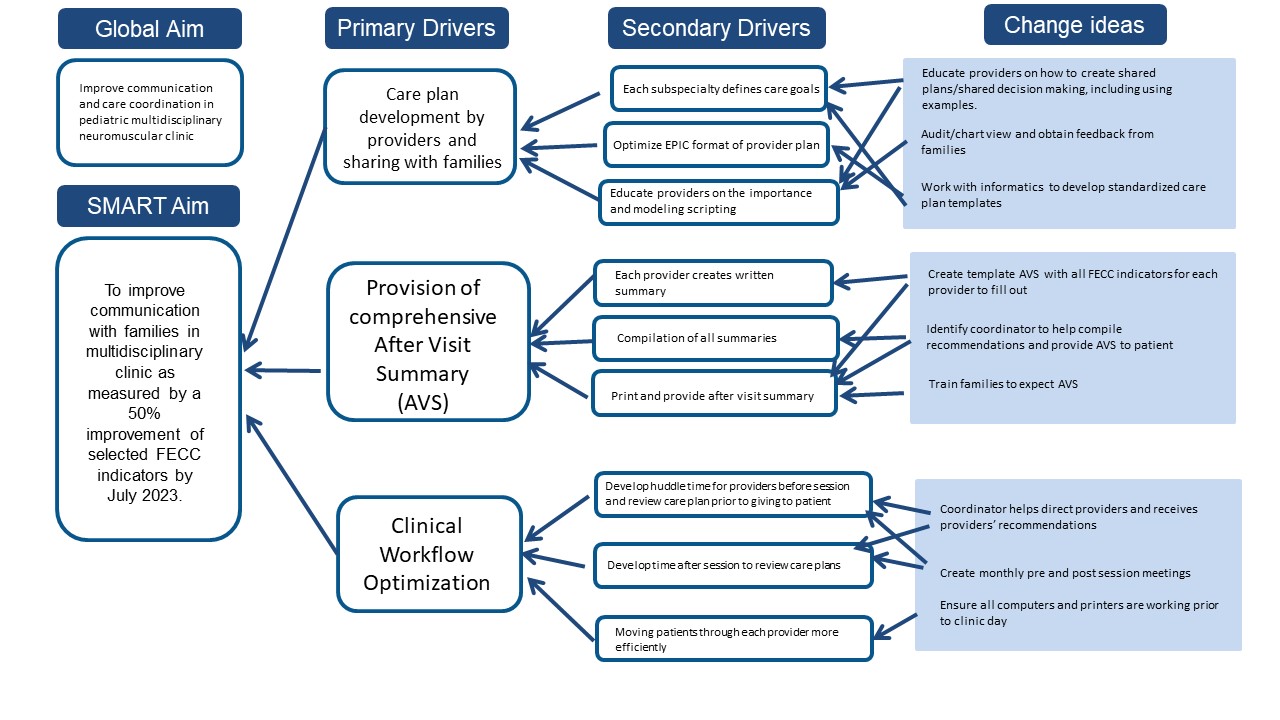
Figure 2. Run Chart of AVS completion.
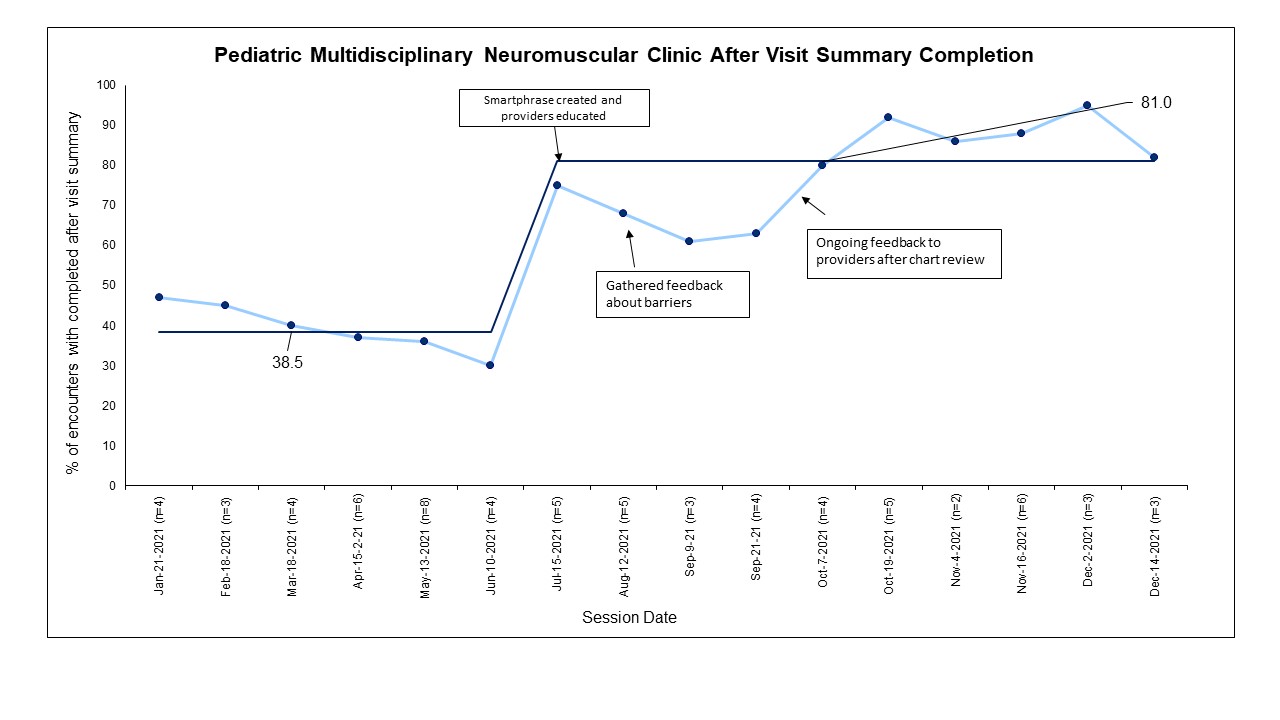 Medians are labeled for PDSA cycles.
Medians are labeled for PDSA cycles.