Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine XIV
51 - Improving physical child abuse screening among children who present maltreatment warning signs
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 51
Publication Number: 51.407
Publication Number: 51.407
Andrea Rivera-Sepulveda, Nemours Children's Hospital, Orlando, FL, United States; Andrea Z. Ali-Panzanella, Nemours Children's Hospital, Orlando, FL, United States; Cara Harwell, Nemours Children’s Hospital, Polk City, FL, United States; Martin J. King, Nemours Children's Hospital, Kissimmee, FL, United States; Kathleen N. Adragna, Nemours Children's Hospital, Orlando, FL, United States; Lydia W. Boettner, Nemours Children's Hospital, Orlando, FL, United States; Maddilyn J. Genova, Nemours Children's Hospital, Cocoa, FL, United States; Brenda Marin-Rivera, Nemours Children's Hospital, Orlando, FL, United States; Sarah Woll, Nemours Children's Hospital, Orlando, FL, United States; Vi Ngo, Nemours Children's Hospital, Orlando, FL, United States; Lisa Spector, Nemours Children's Hospital, Orlando, FL, United States

Andrea Rivera-Sepulveda, MD, MSc
Assistant Professor
Nemours Children's Hospital
ORLANDO, Florida, United States
Presenting Author(s)
Background: About 1 in 4 children experience some form of abuse or neglect in their lifetimes, and at least 1 in 7 children have experienced it in the past year. Younger children are at higher risk, with an incidence of 25 in 1,000 with most fatalities occurring in children younger than 3 years of age. All children’s hospitals see child abuse and neglect, and are responsible for providing immediate care. However, screening rates for suspected abuse range from 10-30%. Ultimately, child maltreatment is a public health problem with lifelong consequences for survivors and their families.
Objective: To improve physical abuse screening rates by using an appropriate, criteria-based tool in children, ages 0 to 2 years, presenting to the ED from median of 20% (baseline) to 50% within 6 months.
Design/Methods: We designed a child abuse initiative to standardize the identification, evaluation, and diagnosis of child physical maltreatment in the Emergency Department (ED) through a continuous improvement methodology with clinical standard work processes and deliverables with PDSA cycles. Target measures included skeletal survey and abdominal laboratories in children less than 2 years, and neuroimaging in children less than 1 year of age. Countermeasures included the 1) implementation of a clinical pathway with historical, physical, and diagnostic testing warning signs, 2) order set, 3) standardization of the reporting structure, 4) systematic review of cases, and 5) education. Balancing measures included the peer review of cases, disposition, and length of stay.
Results: The first PDSA cycle was a learning cycle, where we drew a process map and clarified the roles in the physical abuse screening process. We evaluated 75 patients for concerns of abuse, maltreatment or neglect, of which 16 (4.7%) were less than 2 years of age. Overall child abuse screening rate increased to 68%. Skeletal survey use increased from 80% to 83%; laboratory workup increased from 18% to 74%; and neuroimaging increased from 50% to 80%. Peer review of “near-miss” cases was 10%. Admission rate was 24%, and ED length of stay was 281 minutes.Conclusion(s): Data transparency and peer-review of cases were the most effective methods of promoting compliance and improvement. We performed a multi-pronged, multidisciplinary approach to engage stakeholders and promote buy-in from the hospital personnel, staff, and medical providers. Child abuse is preventable, and the implementation of strategies can increase institutional opportunities to perform early identifications and interventions.
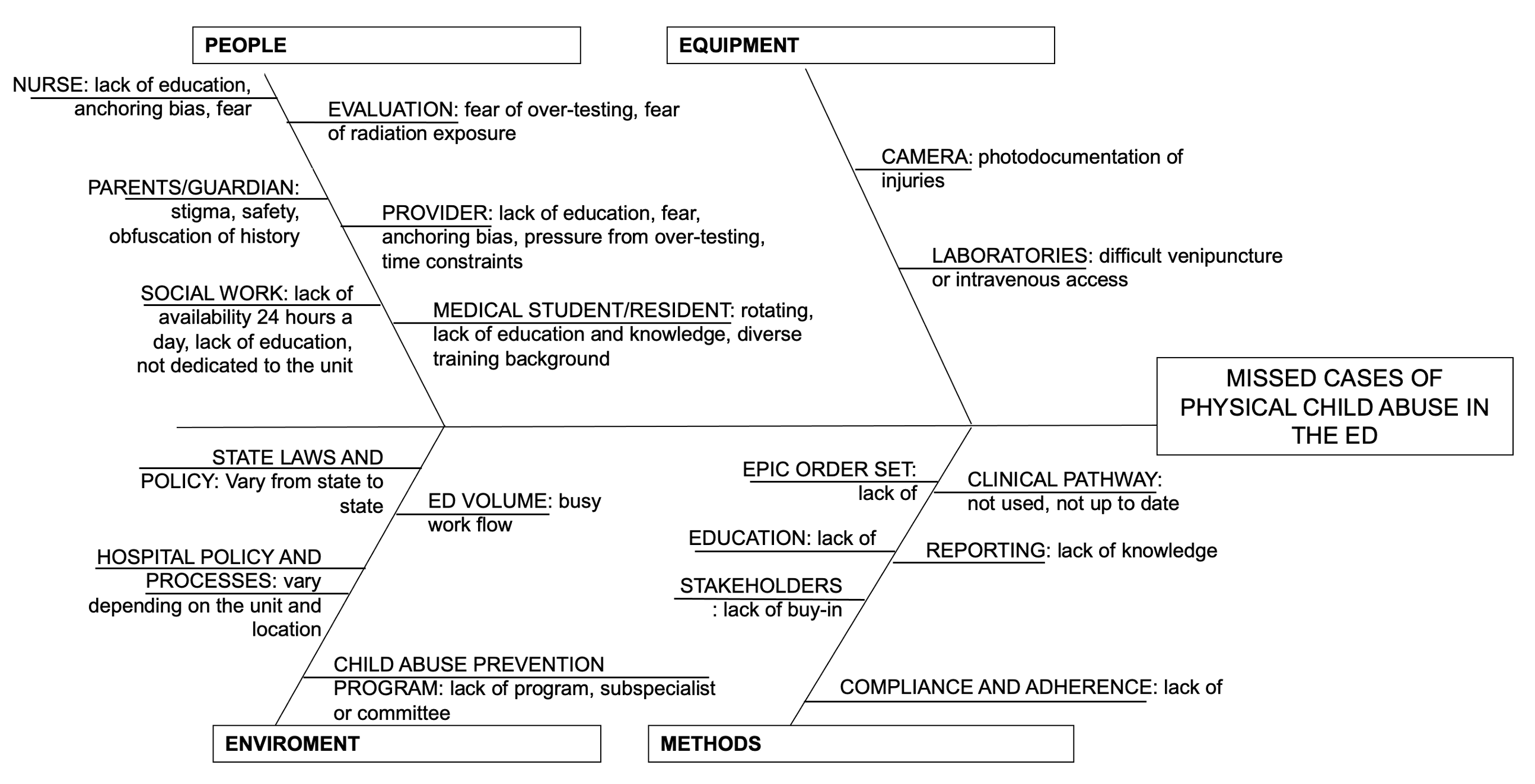
Cause and effect diagram for missed cases of physical child abuse in the emergency department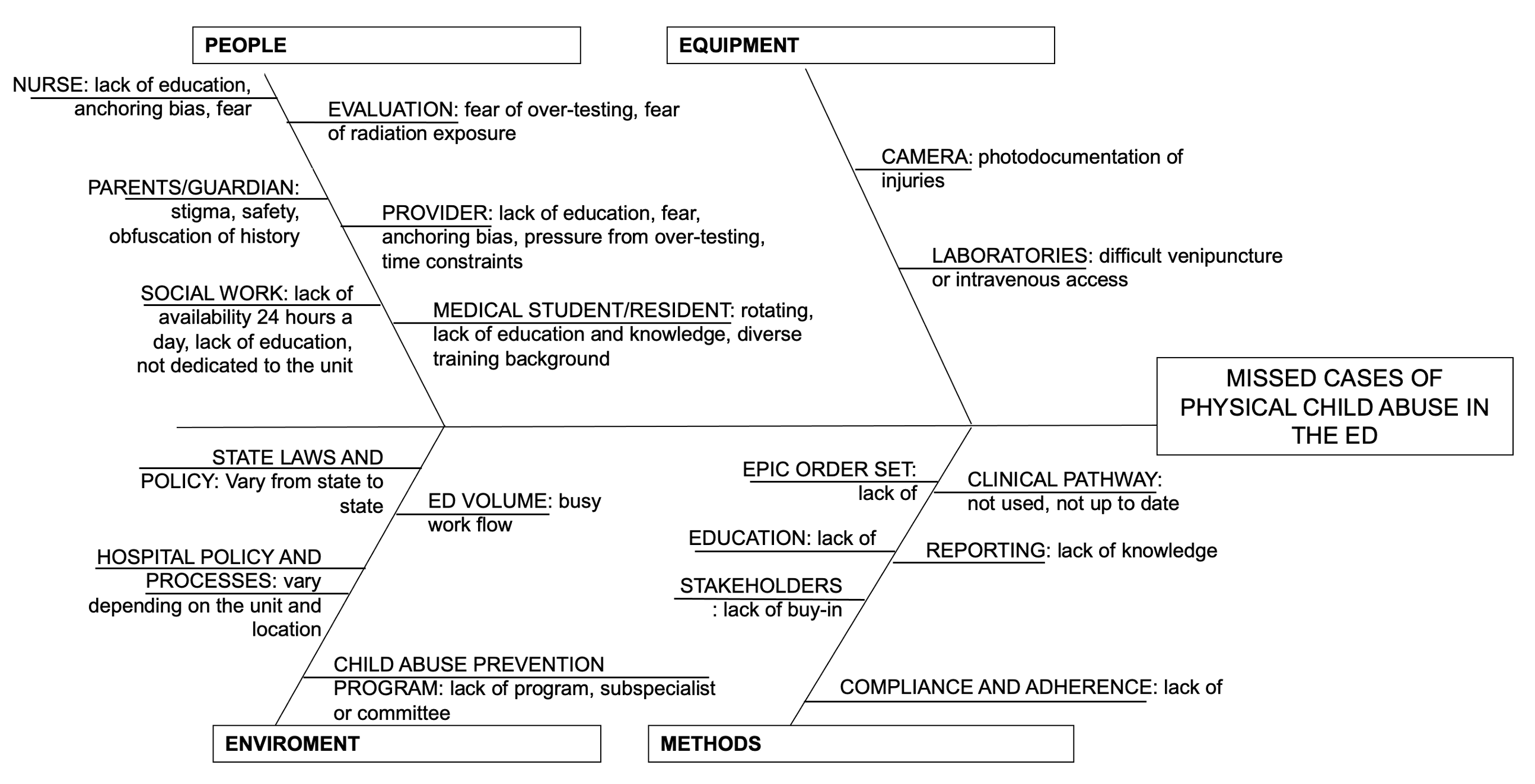
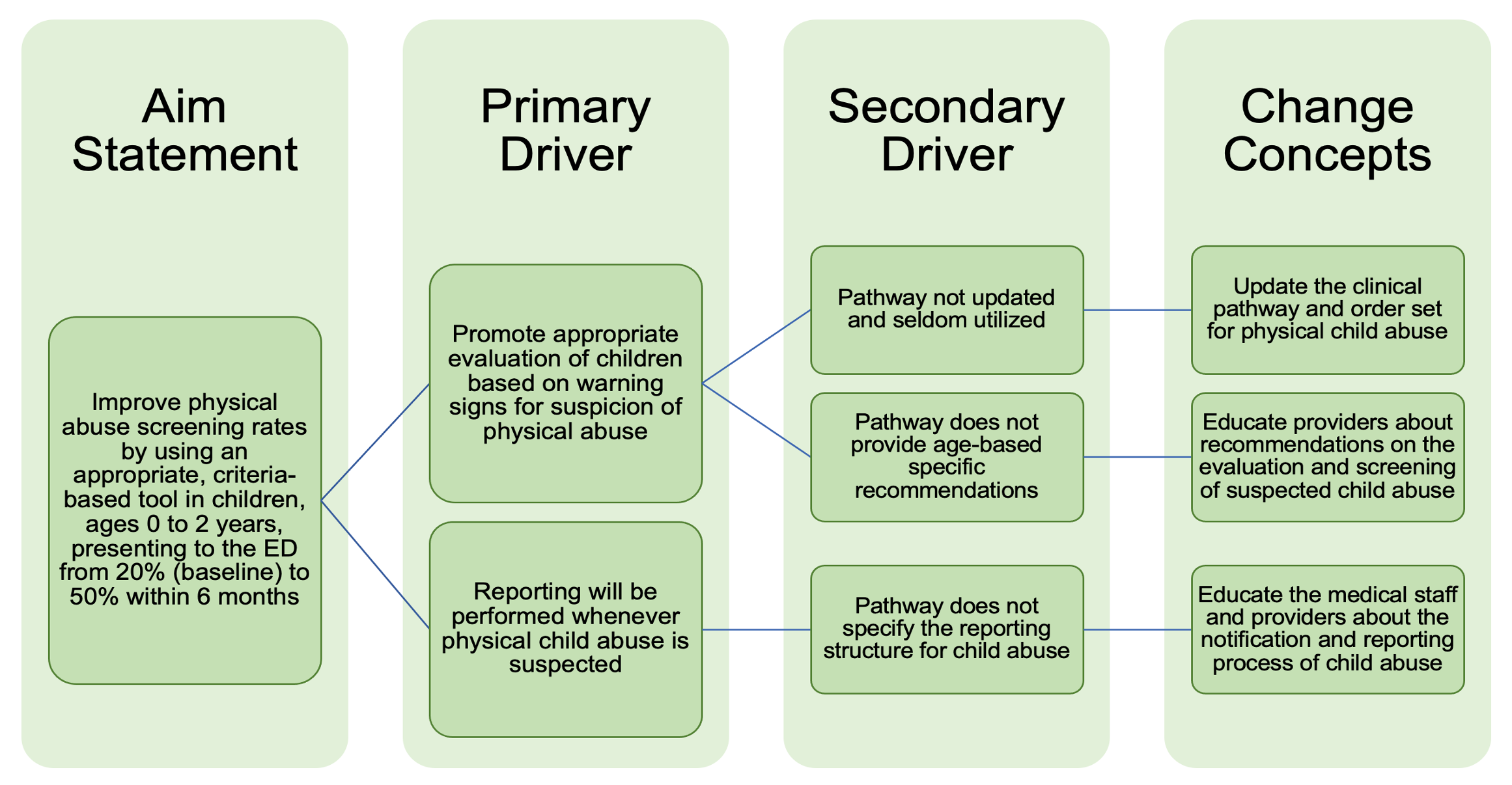
Driver diagram for the evaluation of physical child abuse in the emergency department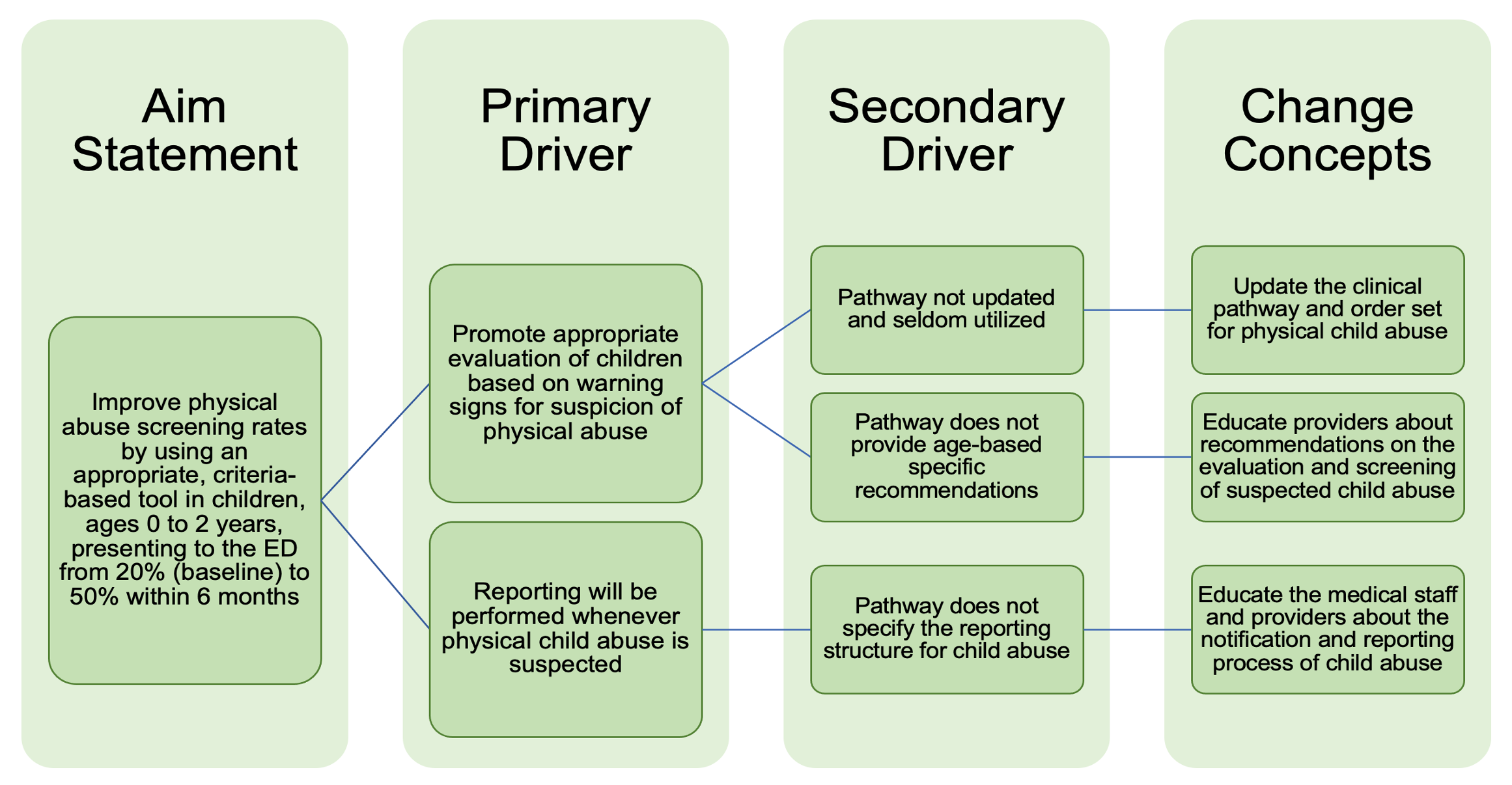
Objective: To improve physical abuse screening rates by using an appropriate, criteria-based tool in children, ages 0 to 2 years, presenting to the ED from median of 20% (baseline) to 50% within 6 months.
Design/Methods: We designed a child abuse initiative to standardize the identification, evaluation, and diagnosis of child physical maltreatment in the Emergency Department (ED) through a continuous improvement methodology with clinical standard work processes and deliverables with PDSA cycles. Target measures included skeletal survey and abdominal laboratories in children less than 2 years, and neuroimaging in children less than 1 year of age. Countermeasures included the 1) implementation of a clinical pathway with historical, physical, and diagnostic testing warning signs, 2) order set, 3) standardization of the reporting structure, 4) systematic review of cases, and 5) education. Balancing measures included the peer review of cases, disposition, and length of stay.
Results: The first PDSA cycle was a learning cycle, where we drew a process map and clarified the roles in the physical abuse screening process. We evaluated 75 patients for concerns of abuse, maltreatment or neglect, of which 16 (4.7%) were less than 2 years of age. Overall child abuse screening rate increased to 68%. Skeletal survey use increased from 80% to 83%; laboratory workup increased from 18% to 74%; and neuroimaging increased from 50% to 80%. Peer review of “near-miss” cases was 10%. Admission rate was 24%, and ED length of stay was 281 minutes.Conclusion(s): Data transparency and peer-review of cases were the most effective methods of promoting compliance and improvement. We performed a multi-pronged, multidisciplinary approach to engage stakeholders and promote buy-in from the hospital personnel, staff, and medical providers. Child abuse is preventable, and the implementation of strategies can increase institutional opportunities to perform early identifications and interventions.
Cause and effect diagram for missed cases of physical child abuse in the emergency department
Driver diagram for the evaluation of physical child abuse in the emergency department