Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine XIV
52 - Improving Pregnancy Screening in the Pediatric Emergency Department
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 52
Publication Number: 52.407
Publication Number: 52.407
Grace Ye, Boston Medical Center, Weston, MA, United States; Bethsabee Stone, Texas Children's Hospital, Houston, TX, United States; Aisling Wright, Boston University School of Medicine, Boston, MA, United States; Joseph Shapiro, Boston Medical Center, Boston, MA, United States; Maria A. Sacta, Boston University School of Medicine, Boston, MA, United States; Charise Freundlich, Boston University School of Medicine/Boston Medical Center, Somerville, MA, United States

Maria A. Sacta, MD-PhD
Resident
Boston University School of Medicine
Boston, Massachusetts, United States
Presenting Author(s)
Background: Adolescents have the highest rates of unintended pregnancy among all age groups 1 and they comprise ~33% of patient visits to the Boston Medical Center (BMC) Pediatric Emergency Department (PED) . Screening for pregnancy in the PED can expedite patient care, narrow differential diagnoses and improve patient safety by reducing missed diagnoses and exposure to teratogens.2,3 The timely diagnosis of pregnancy is also paramount to providing sexual health counseling and referral to time-sensitive family planning services. The BMC PED has no standardized protocol for pregnancy testing and only ~50% of all 15-19 year old females seen receive screening for pregnancy. Creating a protocol to increase pregnancy testing could make patient care safer and more equitable, as well as improve timeliness and efficiency critical in this era of ED overcrowding and legislative changes affective abortion access.
Objective: This initiative aims to increase pregnancy testing in 15-19 year old females in the PED to 80% during the study period.
Design/Methods: Process mapping and driver diagrams were used to reveal and address barriers to pregnancy screening (Figure 1). The primary outcome measure was percentage of 15-19 year old females who received pregnancy testing during their PED visit. The process measure was the percentage of pregnancy tests ordered prior to provider assignment. The balancing measures were pregnancy test positivity rate. Baseline data were collected using random convenience sampling from May to September 2021. Plan-Do-Study-Act cycle 1 (PDSA 1) (September 22 to December 25, 2021) included educating PED staff on new protocols, meeting with key stakeholders, posting pregnancy test related signage in key clinical areas, and sending reminder emails (Figure 2). PDSA 2 is ongoing, focusing on dispersing the protocol more widely, meeting with nurse leadership to understand barriers, and verbal reminders to follow protocol at shift change.
Results: There were 963 and 727 patient encounters in the baseline and PDSA 1 phases, respectively. Comparing the PDSA 1 to the baseline, the median percentage who were tested increased from 50% to 59% (Figure 3), the pregnancy test positivity rate decreased from 8.6% to 5.7%. During PDSA 1, the percentage of pregnancy tests ordered prior to provider assignment ranged from 26%-87% with a median of 47%. Data collection for PDSA 2 is ongoing.Conclusion(s): A new clinical protocol paired with targeted staff education can improve pregnancy testing rates in an urban PED. Further PDSA cycles are needed to find the most effective and sustainable interventions to meet the goal.
Figure 1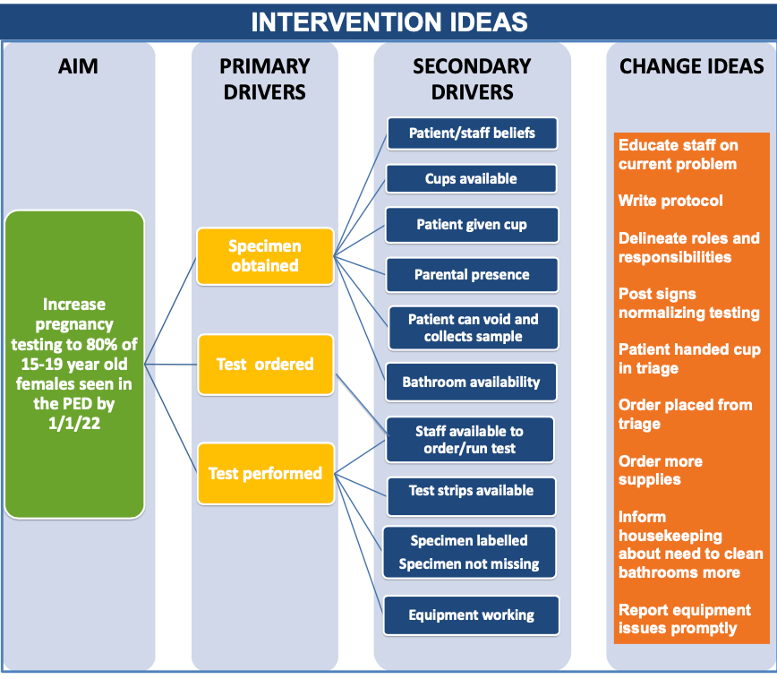 Process mapping and driver diagrams were used to select interventions to address barriers to screening
Process mapping and driver diagrams were used to select interventions to address barriers to screening
Figure 2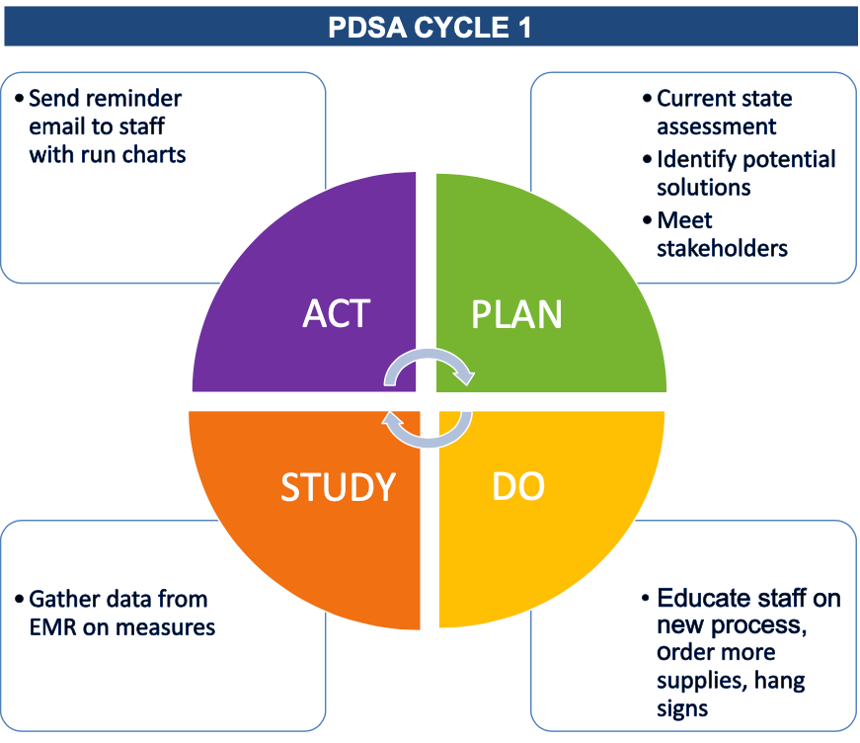 PDSA cycle 1 beginning September 2021
PDSA cycle 1 beginning September 2021
Objective: This initiative aims to increase pregnancy testing in 15-19 year old females in the PED to 80% during the study period.
Design/Methods: Process mapping and driver diagrams were used to reveal and address barriers to pregnancy screening (Figure 1). The primary outcome measure was percentage of 15-19 year old females who received pregnancy testing during their PED visit. The process measure was the percentage of pregnancy tests ordered prior to provider assignment. The balancing measures were pregnancy test positivity rate. Baseline data were collected using random convenience sampling from May to September 2021. Plan-Do-Study-Act cycle 1 (PDSA 1) (September 22 to December 25, 2021) included educating PED staff on new protocols, meeting with key stakeholders, posting pregnancy test related signage in key clinical areas, and sending reminder emails (Figure 2). PDSA 2 is ongoing, focusing on dispersing the protocol more widely, meeting with nurse leadership to understand barriers, and verbal reminders to follow protocol at shift change.
Results: There were 963 and 727 patient encounters in the baseline and PDSA 1 phases, respectively. Comparing the PDSA 1 to the baseline, the median percentage who were tested increased from 50% to 59% (Figure 3), the pregnancy test positivity rate decreased from 8.6% to 5.7%. During PDSA 1, the percentage of pregnancy tests ordered prior to provider assignment ranged from 26%-87% with a median of 47%. Data collection for PDSA 2 is ongoing.Conclusion(s): A new clinical protocol paired with targeted staff education can improve pregnancy testing rates in an urban PED. Further PDSA cycles are needed to find the most effective and sustainable interventions to meet the goal.
Figure 1
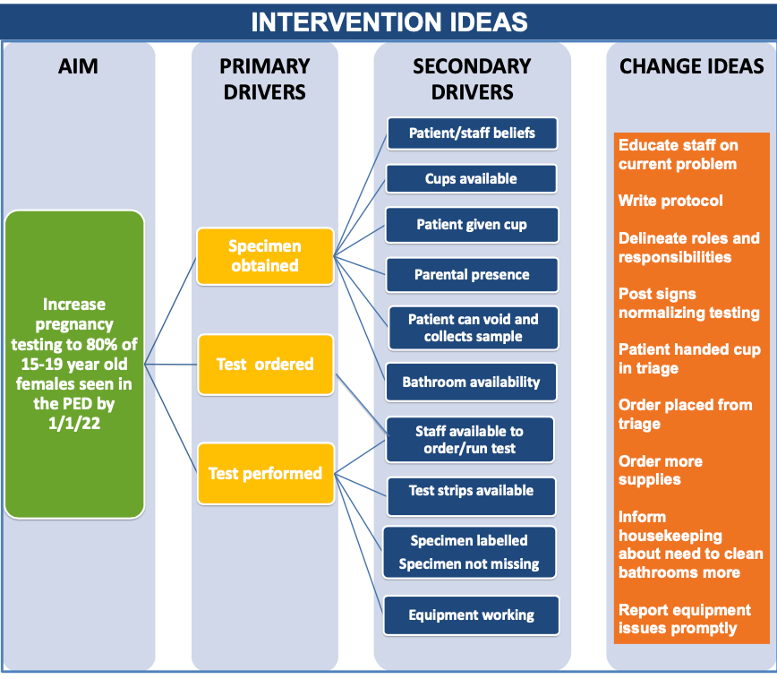 Process mapping and driver diagrams were used to select interventions to address barriers to screening
Process mapping and driver diagrams were used to select interventions to address barriers to screeningFigure 2
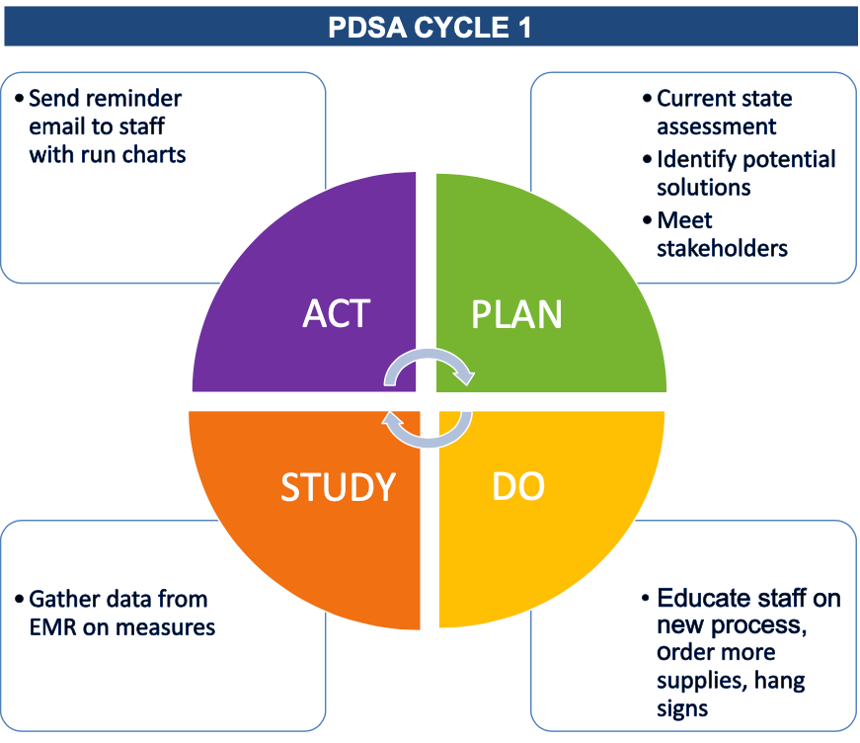 PDSA cycle 1 beginning September 2021
PDSA cycle 1 beginning September 2021