Back
Medical Education: Resident
Category: Abstract Submission
Medical Education 13 - Medical Education: Resident IV
259 - Improving quality of evidence-based medicine discussions and resident engagement in an ambulatory teaching clinic
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 259
Publication Number: 259.419
Publication Number: 259.419
Kelly Jeu, Loma Linda University, Loma Linda, CA, United States; Vallent Lee, Loma Linda University, Loma Linda, CA, United States; Matthew Fong, Loma Linda University, Loma Linda, CA, United States
Kelly Jeu, MD
Instructor of Pediatrics
Loma Linda University
Loma Linda, California, United States
Presenting Author(s)
Background: Evidence-based medicine (EBM) is a key component of practice-based learning, consisting of the ability to critically appraise the literature and translate findings into prescriptive recommendations for specific patients. In our resident ambulatory clinic, learners are encouraged to share their practice-based inquiries and findings from the medical literature. However, residents' unfamiliarity with the skills and terminology of EBM contributes to a reluctance to share their findings or engage in discussion, and teaching such competencies is difficult to incorporate into a busy outpatient clinic setting.
Objective: To improve resident EBM presentations in our ambulatory clinic as measured by quality of presentation content and by audience engagement.
Design/Methods: We created a scoring rubric to evaluate the quality of residents' presentations (Figure 1). Audience engagement was defined as sufficient if at least 3 audience members contributed questions or comments. Over the 2020-2021 academic year, we identified areas of improvement and chose targeted interventions in 4 PDSA cycles: 1) We created and electronically distributed reference handouts on important EBM terminology and presentation format. 2) We provided hard copies of the suggested format and sample discussion questions for residents to use during the presentations. 3) Senior residents were given the responsibility of leading and facilitating audience discussions after presentations. 4) Intern participation was increased by assigning specific dates for their presentations instead of leaving their involvement as voluntary.
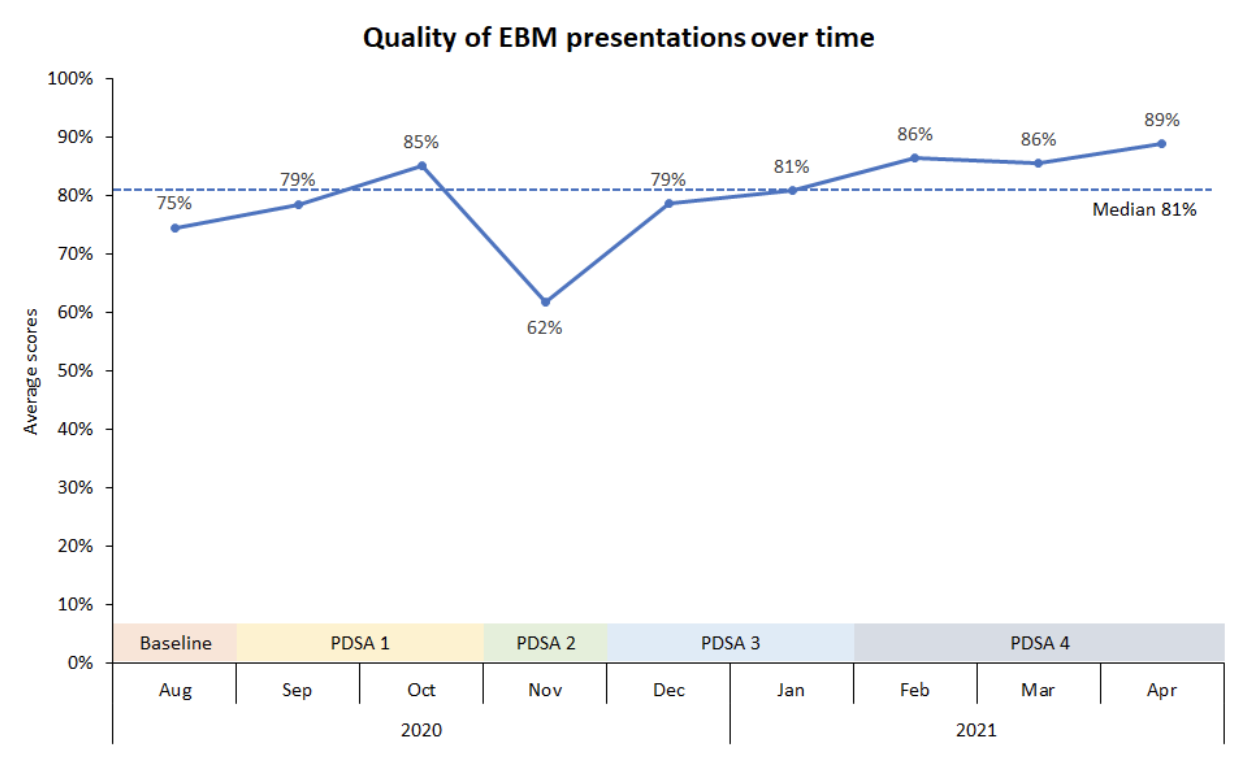
Results: Over 8 months, the quality of presentations increased from a baseline score of 75% to a monthly average of greater than 80% (Figure 2). Audience engagement was observed in 33% of presentations at baseline, increasing to more than 80% of presentations over the course of our interventions (Figure 3). However, it was difficult to shift the responsibility of facilitating discussion from chief residents to senior residents.Conclusion(s): Our interventions led to improvements in quality and audience discussion for resident EBM presentations in the ambulatory teaching clinic. Our handouts provided a shared mental model with structure and concrete expectations for residents to follow. While making presentations mandatory for all levels of training, engagement in discussion was variable, likely due to time constraints and background-level questions from interns. More work is needed to change the mindset of learners from "receiving information" to being responsible for planning and executing teaching conferences.
Figure 1: Scoring rubric for EBM presentations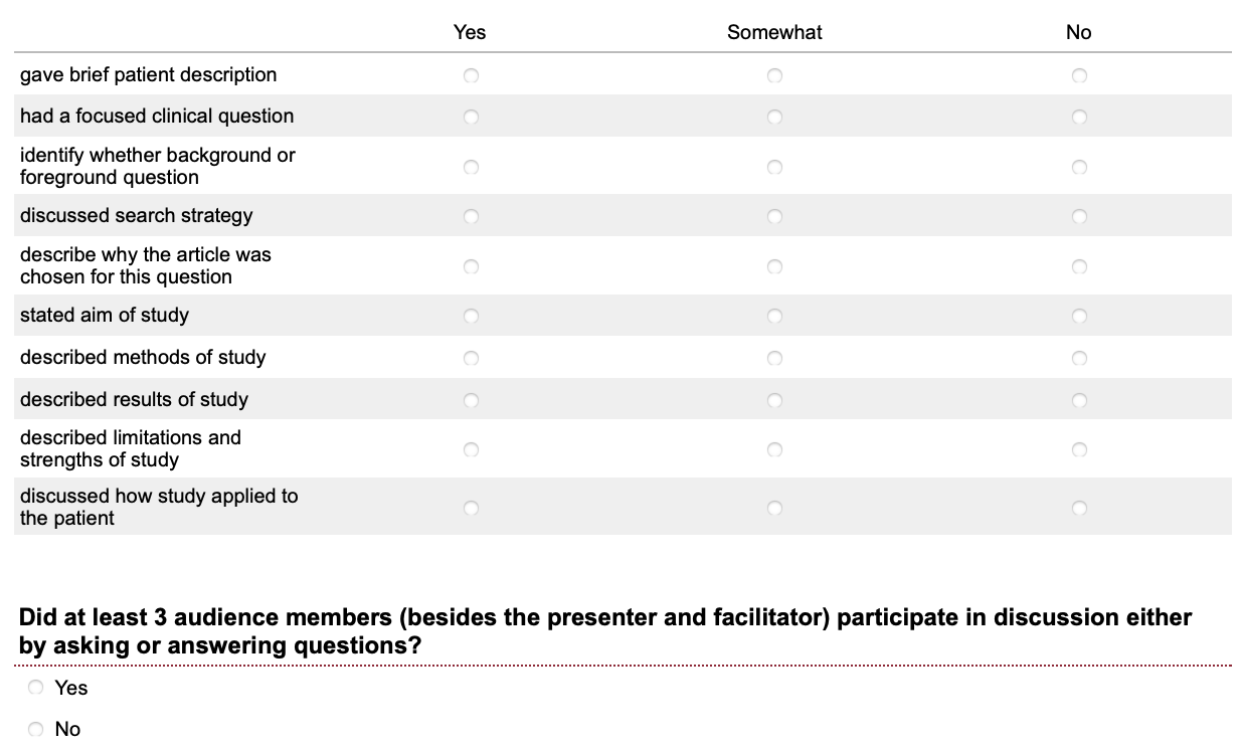
Figure 2: Run chart of quality of EBM presentations over time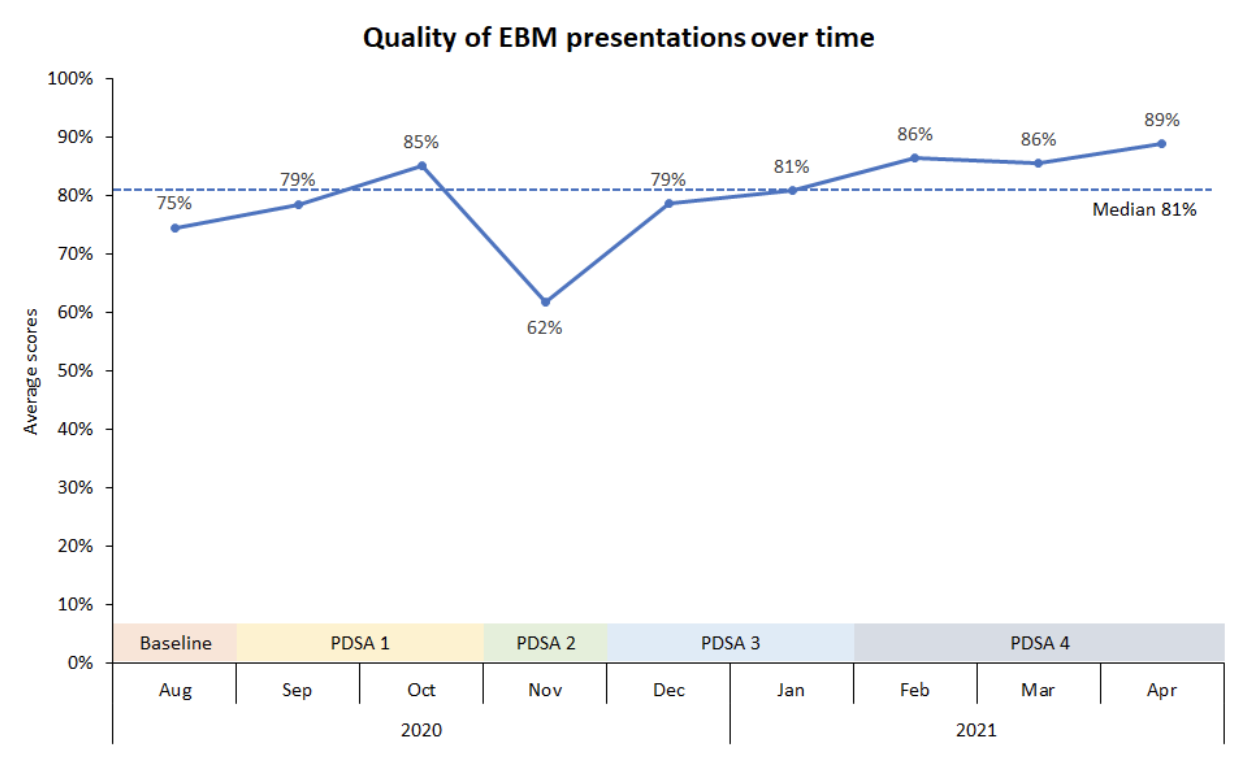
Objective: To improve resident EBM presentations in our ambulatory clinic as measured by quality of presentation content and by audience engagement.
Design/Methods: We created a scoring rubric to evaluate the quality of residents' presentations (Figure 1). Audience engagement was defined as sufficient if at least 3 audience members contributed questions or comments. Over the 2020-2021 academic year, we identified areas of improvement and chose targeted interventions in 4 PDSA cycles: 1) We created and electronically distributed reference handouts on important EBM terminology and presentation format. 2) We provided hard copies of the suggested format and sample discussion questions for residents to use during the presentations. 3) Senior residents were given the responsibility of leading and facilitating audience discussions after presentations. 4) Intern participation was increased by assigning specific dates for their presentations instead of leaving their involvement as voluntary.
Results: Over 8 months, the quality of presentations increased from a baseline score of 75% to a monthly average of greater than 80% (Figure 2). Audience engagement was observed in 33% of presentations at baseline, increasing to more than 80% of presentations over the course of our interventions (Figure 3). However, it was difficult to shift the responsibility of facilitating discussion from chief residents to senior residents.Conclusion(s): Our interventions led to improvements in quality and audience discussion for resident EBM presentations in the ambulatory teaching clinic. Our handouts provided a shared mental model with structure and concrete expectations for residents to follow. While making presentations mandatory for all levels of training, engagement in discussion was variable, likely due to time constraints and background-level questions from interns. More work is needed to change the mindset of learners from "receiving information" to being responsible for planning and executing teaching conferences.
Figure 1: Scoring rubric for EBM presentations
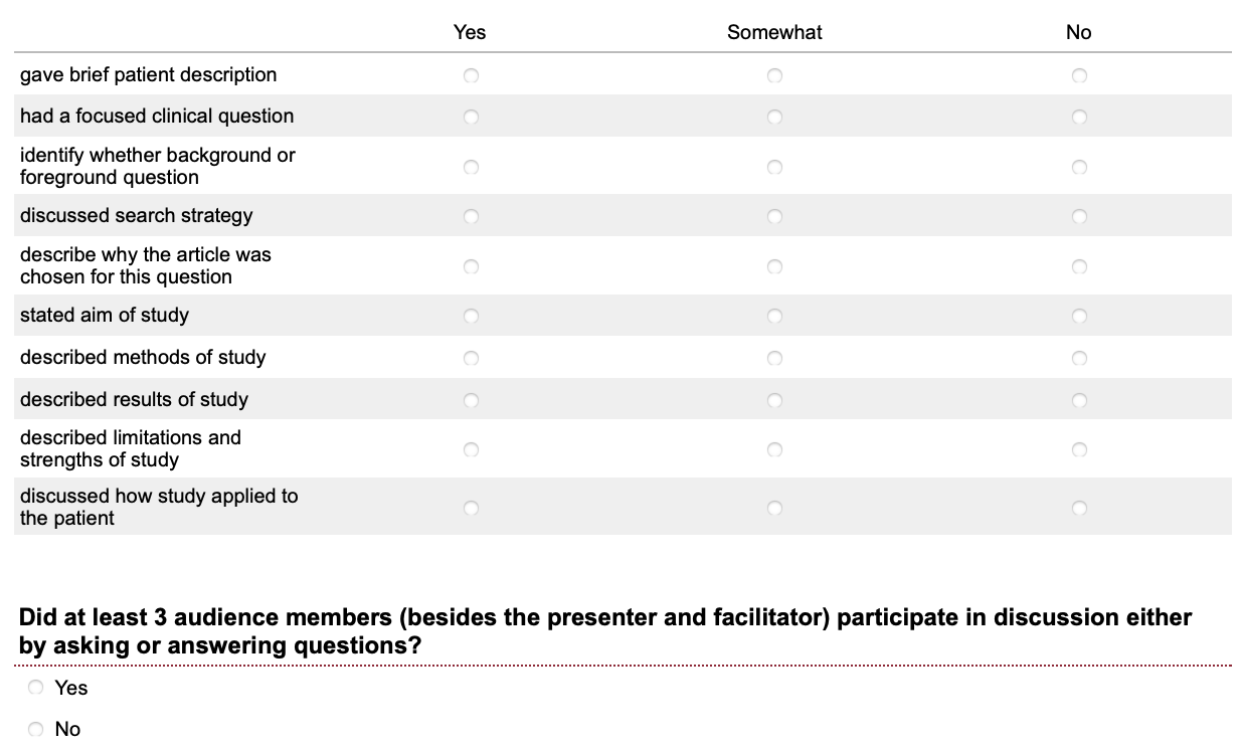
Figure 2: Run chart of quality of EBM presentations over time