Hospital Medicine: Systems/Population-based Research
Category: Abstract Submission
Hospital Medicine: Systems/Population Health
147 - Increase in acute respiratory failure diagnosis among hospitalized infants – What does it mean?
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 147
Publication Number: 147.416
Publication Number: 147.416
Kathleen D. Snow, Boston Children's Hospital, Boston, MA, United States; Sarah C. McBride, Boston Children's Hospital, Boston, MA, United States; Jonathan Mansbach, Boston Children's Hospital, Boston, MA, United States

Kathleen Doherty Snow, MD
Clinical Fellow
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Acute respiratory infections in infants and young children account for over 10% of all pediatric inpatient admissions. Recent studies have identified respiratory failure as one of the most prevalent and expensive pediatric medical conditions, but little is known about this patient population or the underlying etiology for their hospitalization.
Objective: To evaluate patient characteristics, hospitalization details and trends for young children diagnosed with acute respiratory failure (ARF) from 2010-2019.
Design/Methods: We conducted a retrospective cross-sectional analysis of young children (ages 0-2 years) admitted for an inpatient or observation encounter with a primary diagnosis of ARF (ICD-9 518.81 or ICD-10 J96) from January 1, 2010 – December 31, 2019 at one of 36 children’s hospitals included in the Pediatric Health Information System (PHIS) database. Primary outcomes included number of encounters, patient demographics, ICU admission, hospitalization severity and costs. We also examined common secondary diagnostic codes assigned at time of discharge.
Results: There were a total of 44,673 encounters with a primary discharge diagnosis of ARF for children age < 2 years between 2010 and 2019. Median age was 7 months (IQR 3-13 months), 59% were male and 29% had complex chronic conditions. The most common secondary ICD-9 and ICD-10 diagnosis codes assigned at discharge were associated with bronchiolitis. Since 2016, ARF has been the second leading respiratory diagnosis after bronchiolitis in this age group (Figure 1). Between 2010-2019 hospitalizations for ARF increased almost 10-fold (p for trend < 0.001) and were less likely to be admitted to the ICU (96% to 57%) or require mechanical ventilation (84% to 16%). Average length of stay decreased from 15.7 days in 2010 to 5.2 days in 2019 with a corresponding drop in average APR-DRG severity level for hospitalization over time. Average adjusted costs per encounter decreased from $59,708 in 2010 to $20,062 in 2019 but remained higher than costs for other respiratory diagnoses (2019 costs per encounter: bronchiolitis $8,596; asthma $5,494; pneumonia $16,987).Conclusion(s): Acute respiratory failure is now one of the most common primary respiratory diagnoses for children age < 2 years at discharge and likely represents a spectrum of underlying diseases and illness severity. While this trend may be a result of changes in coding and billing practices, it remains important to better characterize this population of children that accrues high-cost care in the hospital.
CV_Kathleen SnowCV_KDohertySnow.pdf
Table 1: Characteristics of acute respiratory failure hospitalizations 2010-2019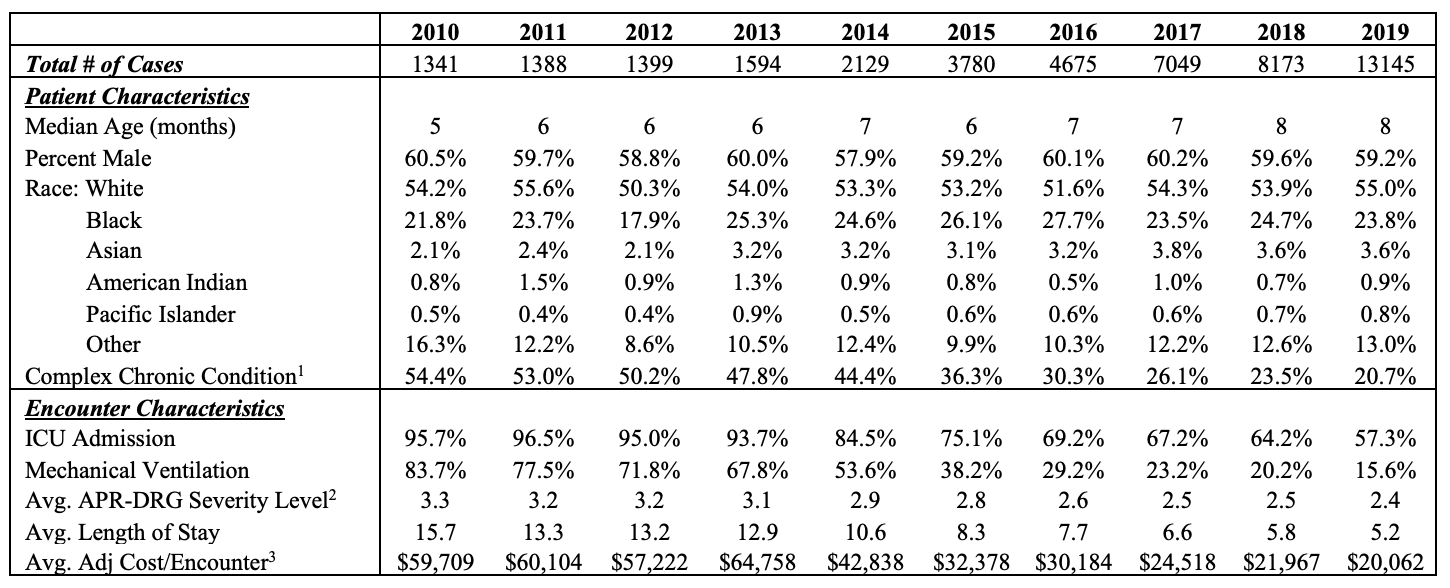 1. Complex Chronic Condition: As defined by Feudtner et al ‘Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation’ BMC Pediatrics 2014,14:199.
1. Complex Chronic Condition: As defined by Feudtner et al ‘Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation’ BMC Pediatrics 2014,14:199.
2. APR-DRG Severity Level: Assigned per 3M’s APR-DRG grouper. 0 = Not Applicable, 1=Minor, 2=Moderate, 3=Major, 4=Extreme
3. Average Adjusted Cost: The total patient costs based upon the Ratio of Costs to Charges submitted by hospitals on their respective Medicare cost reports. Charges were adjusted by the CMS wage/price index for the hospital’s location.
Objective: To evaluate patient characteristics, hospitalization details and trends for young children diagnosed with acute respiratory failure (ARF) from 2010-2019.
Design/Methods: We conducted a retrospective cross-sectional analysis of young children (ages 0-2 years) admitted for an inpatient or observation encounter with a primary diagnosis of ARF (ICD-9 518.81 or ICD-10 J96) from January 1, 2010 – December 31, 2019 at one of 36 children’s hospitals included in the Pediatric Health Information System (PHIS) database. Primary outcomes included number of encounters, patient demographics, ICU admission, hospitalization severity and costs. We also examined common secondary diagnostic codes assigned at time of discharge.
Results: There were a total of 44,673 encounters with a primary discharge diagnosis of ARF for children age < 2 years between 2010 and 2019. Median age was 7 months (IQR 3-13 months), 59% were male and 29% had complex chronic conditions. The most common secondary ICD-9 and ICD-10 diagnosis codes assigned at discharge were associated with bronchiolitis. Since 2016, ARF has been the second leading respiratory diagnosis after bronchiolitis in this age group (Figure 1). Between 2010-2019 hospitalizations for ARF increased almost 10-fold (p for trend < 0.001) and were less likely to be admitted to the ICU (96% to 57%) or require mechanical ventilation (84% to 16%). Average length of stay decreased from 15.7 days in 2010 to 5.2 days in 2019 with a corresponding drop in average APR-DRG severity level for hospitalization over time. Average adjusted costs per encounter decreased from $59,708 in 2010 to $20,062 in 2019 but remained higher than costs for other respiratory diagnoses (2019 costs per encounter: bronchiolitis $8,596; asthma $5,494; pneumonia $16,987).Conclusion(s): Acute respiratory failure is now one of the most common primary respiratory diagnoses for children age < 2 years at discharge and likely represents a spectrum of underlying diseases and illness severity. While this trend may be a result of changes in coding and billing practices, it remains important to better characterize this population of children that accrues high-cost care in the hospital.
CV_Kathleen SnowCV_KDohertySnow.pdf
Table 1: Characteristics of acute respiratory failure hospitalizations 2010-2019
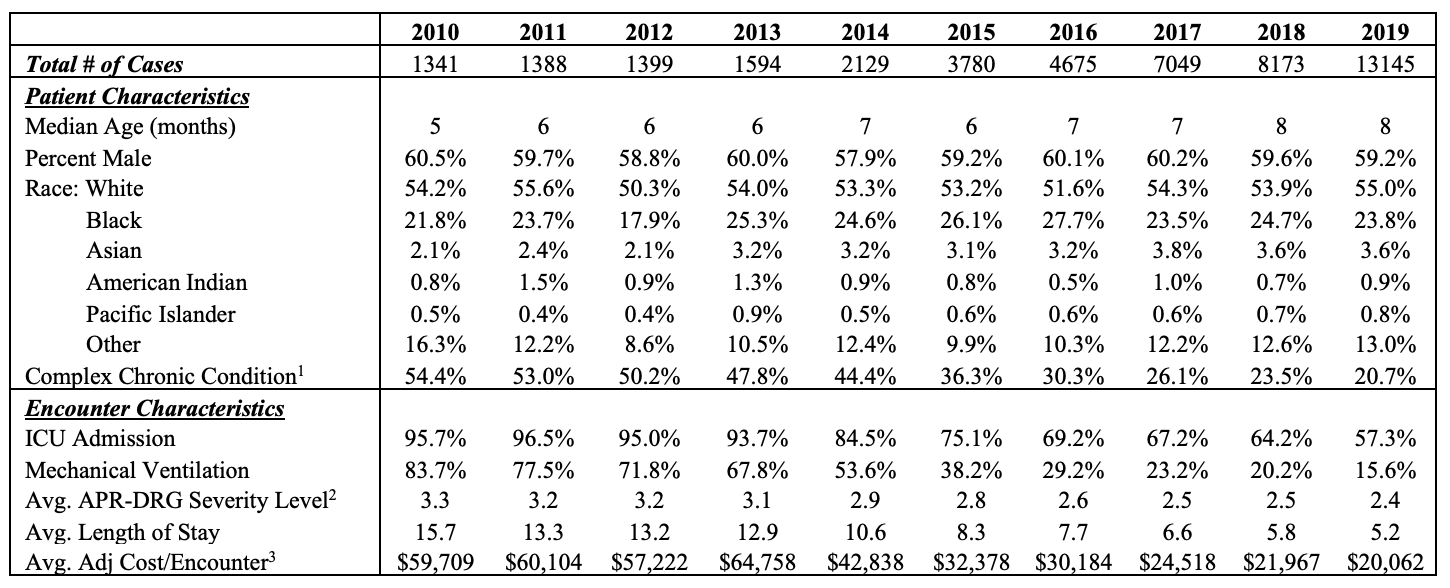 1. Complex Chronic Condition: As defined by Feudtner et al ‘Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation’ BMC Pediatrics 2014,14:199.
1. Complex Chronic Condition: As defined by Feudtner et al ‘Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation’ BMC Pediatrics 2014,14:199.2. APR-DRG Severity Level: Assigned per 3M’s APR-DRG grouper. 0 = Not Applicable, 1=Minor, 2=Moderate, 3=Major, 4=Extreme
3. Average Adjusted Cost: The total patient costs based upon the Ratio of Costs to Charges submitted by hospitals on their respective Medicare cost reports. Charges were adjusted by the CMS wage/price index for the hospital’s location.
