Back
Medical Education: Resident
Category: Abstract Submission
Medical Education 13 - Medical Education: Resident IV
260 - Moving Beyond Baseline Requirements to Maximize Impact: Improving Trainee QI Experience through Integration in a Multi-institutional Collaborative to Address Food Insecurity
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 260
Publication Number: 260.419
Publication Number: 260.419
Carolyn Avery, Duke, Durham, NC, United States; Kristina Gustafson, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Jane B. Amati, University of South Carolina School of Medicine Greenville, Greenville, SC, United States; Shivani Mehta, Atrium Health, Charlotte, NC, United States; Kimberly Montez, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, WINSTON-SALEM, NC, United States; Debra Best, Duke University School of Medicine, Durham, NC, United States; Kerry Sease, University of South Carolina School of Medicine Greenville, Greenville, SC, United States; Meredith Eicken, University of South Carolina School of Medicine Greenville, Greenville, SC, United States
- CA
Carolyn Sears Avery, MD, MHS
Associate Professor
Duke Pediatrics and Internal Medicine-Pediatrics
Durham, North Carolina, United States
Presenting Author(s)
Background: Pediatric residency programs are tasked to train and facilitate resident experiences in quality improvement (QI) processes including activities aimed at reducing health care disparities per ACGME requirements. Numerous barriers to successful resident QI project implementation have been documented in the literature including limited faculty expertise, time, and funding.
Objective: Identify opportunities to enhance resident participation in and scholarly output from QI by leveraging an existing multi-institution faculty collaborative.
Design/Methods: The Carolinas Collaborative provides faculty infrastructure for an academic QI collaborative across the 8 NC & SC pediatric residency programs to address food insecurity (FI) over a 2 year grant-funded period from Jan 2020-Dec 2022. The clinical aim of the QI project was to increase FI screening and referral rates to above 80% at all 8 sites with 3 sites initiating screening for first time. Plan-Do-Study-Act cycles were tracked in a central shared document. Residents from each institution were incorporated into site teams and invited to participate in monthly virtual meetings. The academic goal of the collaborative was to improve resident education and scholarly involvement in QI and advocacy.
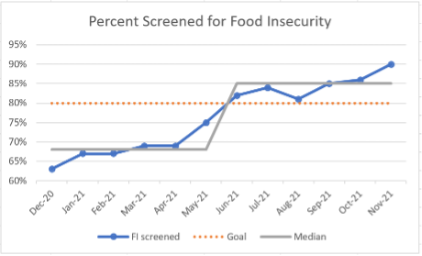
Results: 33 residents have participated in FI QI activities with the collaborative (Table 1). 26 didactics in FI QI by faculty have reached 418 residents. This QI support structure has resulted in 15 residents with QI scholarly work including regional or national presentations by residents at 3 of the 8 institutions. This has also resulted in significant impact to patients – outcome measures to attain 80% FI screening were met (Figure 1). In a chart review of a subset of patients across all institutions, 282/2380 (11.8%) were identified as having FI and 240/282 (85.1%) were referred to resources (Figure 2). Conclusion(s): There are numerous barriers to successful resident engagement in QI during training. This novel incorporation of trainees into a large multi-institutional faculty collaborative has demonstrated promising results in launching and sustaining resident QI initiatives. Through partnering with faculty mentors and sharing innovative solutions across institutions, individual QI projects achieve higher impact in scope, endurance, and scholarship. This model is replicable to other Pediatrics training programs.
Table 1. Resident Engagement and Scholarly Outputs from Food Insecurity (FI) Quality Improvement (QI)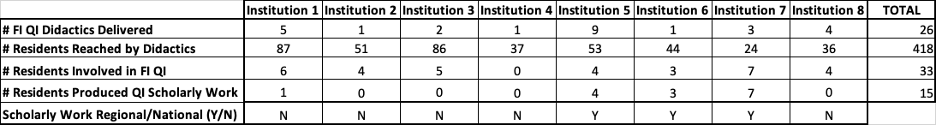
Figure 1. Rate of Screening for FI at Eligible Visits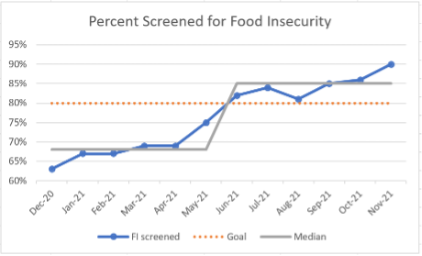
Objective: Identify opportunities to enhance resident participation in and scholarly output from QI by leveraging an existing multi-institution faculty collaborative.
Design/Methods: The Carolinas Collaborative provides faculty infrastructure for an academic QI collaborative across the 8 NC & SC pediatric residency programs to address food insecurity (FI) over a 2 year grant-funded period from Jan 2020-Dec 2022. The clinical aim of the QI project was to increase FI screening and referral rates to above 80% at all 8 sites with 3 sites initiating screening for first time. Plan-Do-Study-Act cycles were tracked in a central shared document. Residents from each institution were incorporated into site teams and invited to participate in monthly virtual meetings. The academic goal of the collaborative was to improve resident education and scholarly involvement in QI and advocacy.
Results: 33 residents have participated in FI QI activities with the collaborative (Table 1). 26 didactics in FI QI by faculty have reached 418 residents. This QI support structure has resulted in 15 residents with QI scholarly work including regional or national presentations by residents at 3 of the 8 institutions. This has also resulted in significant impact to patients – outcome measures to attain 80% FI screening were met (Figure 1). In a chart review of a subset of patients across all institutions, 282/2380 (11.8%) were identified as having FI and 240/282 (85.1%) were referred to resources (Figure 2). Conclusion(s): There are numerous barriers to successful resident engagement in QI during training. This novel incorporation of trainees into a large multi-institutional faculty collaborative has demonstrated promising results in launching and sustaining resident QI initiatives. Through partnering with faculty mentors and sharing innovative solutions across institutions, individual QI projects achieve higher impact in scope, endurance, and scholarship. This model is replicable to other Pediatrics training programs.
Table 1. Resident Engagement and Scholarly Outputs from Food Insecurity (FI) Quality Improvement (QI)
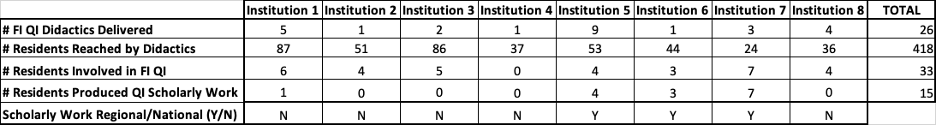
Figure 1. Rate of Screening for FI at Eligible Visits