Neonatal GI Physiology & NEC
Category: Abstract Submission
Neonatal GI Physiology & NEC III
507 - Medical and surgical necrotizing enterocolitis: Characteristics, progression, and outcomes
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 507
Publication Number: 507.426
Publication Number: 507.426
Maher Shahroor, Sunnybrook Health Sciences Center, Milton, ON, Canada; Mohamed Elkhouli, The Hospital for Sick Children, Toronto, ON, Canada; Niloofar Ganji, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Kyong-Soon Lee, The Hospital for Sick Children, Toronto, ON, Canada; Agostino Pierro, The Hospital for Sick Children, Toronto, ON, Canada; Prakesh Shah, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada
- MS
Maher Shahroor, MD
Neonatologist
Sunnybrook Health Sciences Center
Milton, Ontario, Canada
Presenting Author(s)
Background: Necrotizing enterocolitis (NEC) in preterm infants especially those require surgical intervention have higher morbidity and mortality. In most neonates, it is a progressive disease from Medical NEC (mNEC) to surgical NEC (sNEC); however, in some it presents as sNEC from onset. To develop strategies to intervene in the progression it is important to establish rate, timing of progression, and outcomes of NEC
Objective: To evaluate rate, timing of progression, and outcomes of mNEC as well as progression and outcomes of neonates who presents as sNEC in preterm neonates
Design/Methods: A retrospective cohort study of infants born at < 37 weeks’ gestation (GA), admitted between 2010-2020 to a tertiary perinatal center and a children’s hospital NICUs in Toronto was conducted. Charts of all neonates with diagnosis of NEC (excluding stage 1 NEC) were reviewed and data on clinical presentation, NEC progression, treatment received, and outcomes prior to discharge or death from NICU were abstracted. Surgical NEC was defined as those who had intestinal perforation detected via imaging or those who received surgical intervention. Infants were classified in 3 groups: mNEC, mNEC that progressed to sNEC, and sNEC at presentation. Mortality, post-NEC morbidities and resource utilization were compared between groups. Time interval from presentation to progression for mNEC to sNEC group was estimated. Student's t-test for continuous variables, Chi-square test for categorical variables, ANOVA were used to compare the groups
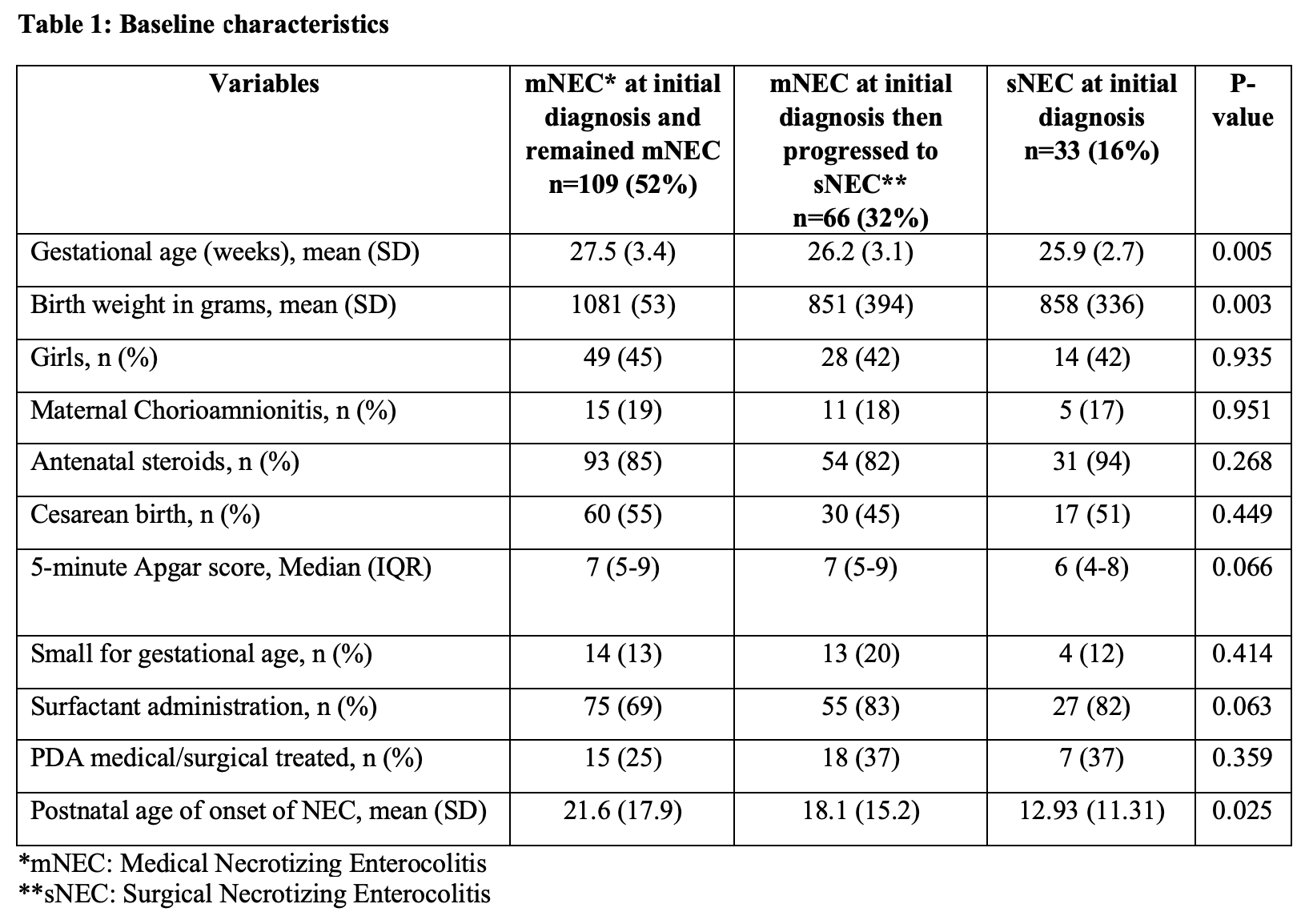
Results: The distribution of NEC stage at presentation in 208 included patients and their progress is shown in Figure 1. 52% of infants remained as mNEC, 32% progressed from mNEC to sNEC whereas 16% presented with sNEC. Progression from mNEC to sNEC occurred at median of 2.5 days (IQR 1- 4.25 days). Clinical characteristics of three groups are compared in Table 1. GA, birthweight (BW), and corrected postnatal age at first NEC episode were inversely associated with the development of sNEC. Data on clinical outcomes and resource utilization are reported in Table 2. sNEC infants stayed longer on antibiotics, inotropes, respiratory support, in the hospital, and had delay in reaching full feeds, had more strictures, frequent NEC episodes, higher BPD rates, and high mortality (table 2). Surgical management of those who developed sNEC is reported in Figure 1Conclusion(s): Among infants who present with mNEC, approximately one in 3 progressed to sNEC between 2-3 days after presentation. sNEC at presentation and progression to sNEC from mNEC were associated with higher mortality and neonatal morbidities
Figure 1: Flow diagram of patients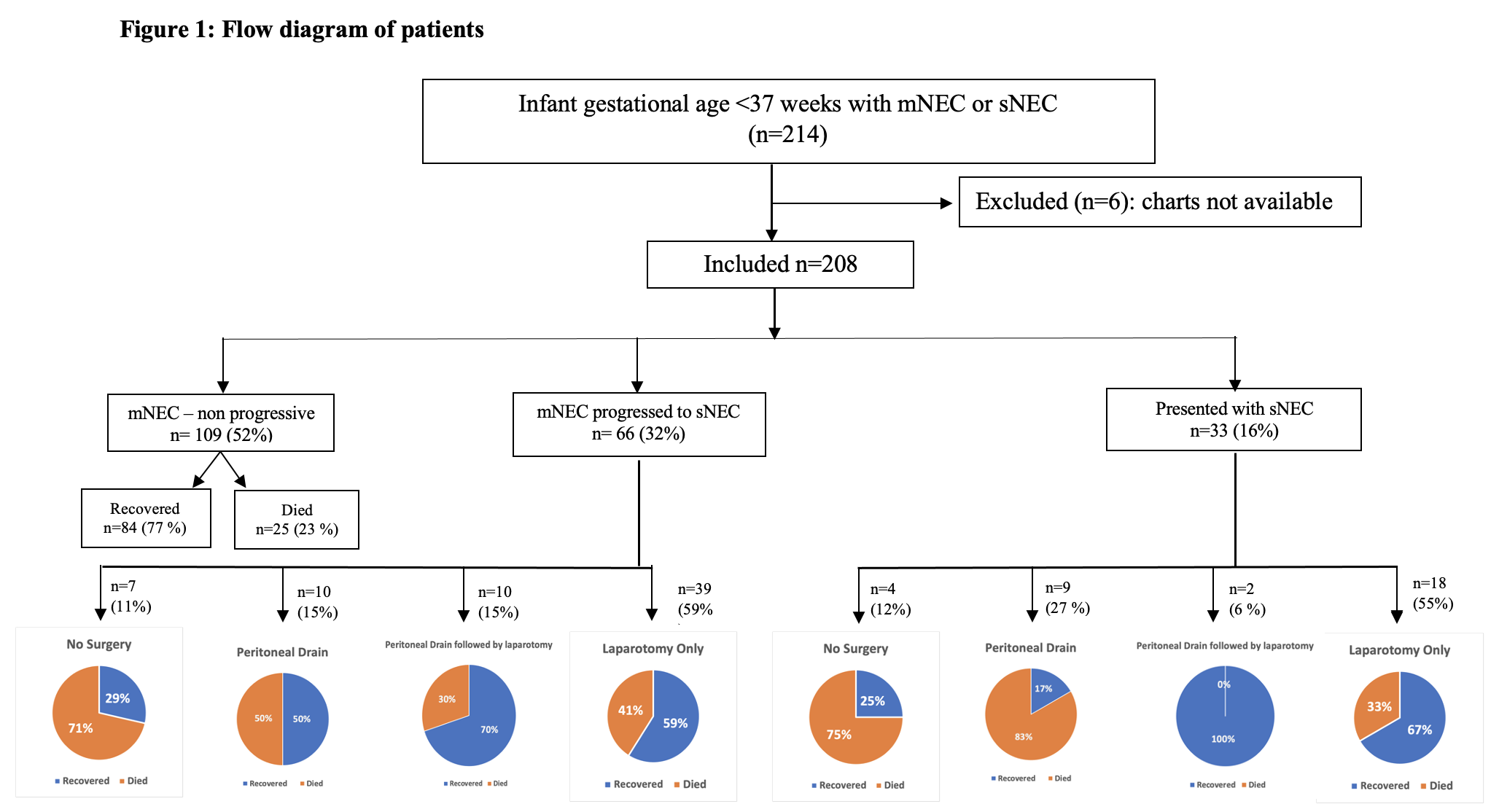
Table 1: Baseline characteristics of patients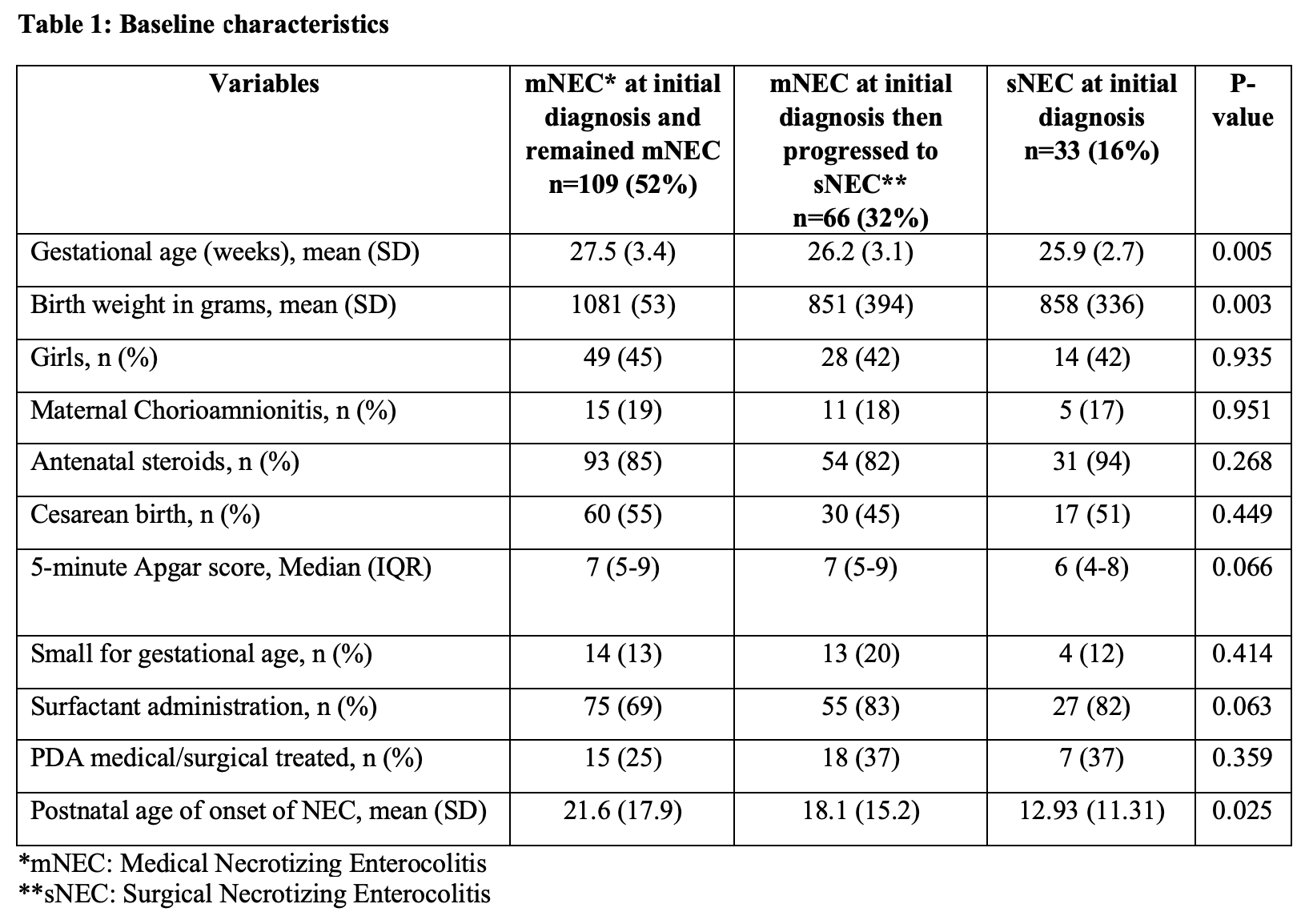
Objective: To evaluate rate, timing of progression, and outcomes of mNEC as well as progression and outcomes of neonates who presents as sNEC in preterm neonates
Design/Methods: A retrospective cohort study of infants born at < 37 weeks’ gestation (GA), admitted between 2010-2020 to a tertiary perinatal center and a children’s hospital NICUs in Toronto was conducted. Charts of all neonates with diagnosis of NEC (excluding stage 1 NEC) were reviewed and data on clinical presentation, NEC progression, treatment received, and outcomes prior to discharge or death from NICU were abstracted. Surgical NEC was defined as those who had intestinal perforation detected via imaging or those who received surgical intervention. Infants were classified in 3 groups: mNEC, mNEC that progressed to sNEC, and sNEC at presentation. Mortality, post-NEC morbidities and resource utilization were compared between groups. Time interval from presentation to progression for mNEC to sNEC group was estimated. Student's t-test for continuous variables, Chi-square test for categorical variables, ANOVA were used to compare the groups
Results: The distribution of NEC stage at presentation in 208 included patients and their progress is shown in Figure 1. 52% of infants remained as mNEC, 32% progressed from mNEC to sNEC whereas 16% presented with sNEC. Progression from mNEC to sNEC occurred at median of 2.5 days (IQR 1- 4.25 days). Clinical characteristics of three groups are compared in Table 1. GA, birthweight (BW), and corrected postnatal age at first NEC episode were inversely associated with the development of sNEC. Data on clinical outcomes and resource utilization are reported in Table 2. sNEC infants stayed longer on antibiotics, inotropes, respiratory support, in the hospital, and had delay in reaching full feeds, had more strictures, frequent NEC episodes, higher BPD rates, and high mortality (table 2). Surgical management of those who developed sNEC is reported in Figure 1Conclusion(s): Among infants who present with mNEC, approximately one in 3 progressed to sNEC between 2-3 days after presentation. sNEC at presentation and progression to sNEC from mNEC were associated with higher mortality and neonatal morbidities
Figure 1: Flow diagram of patients
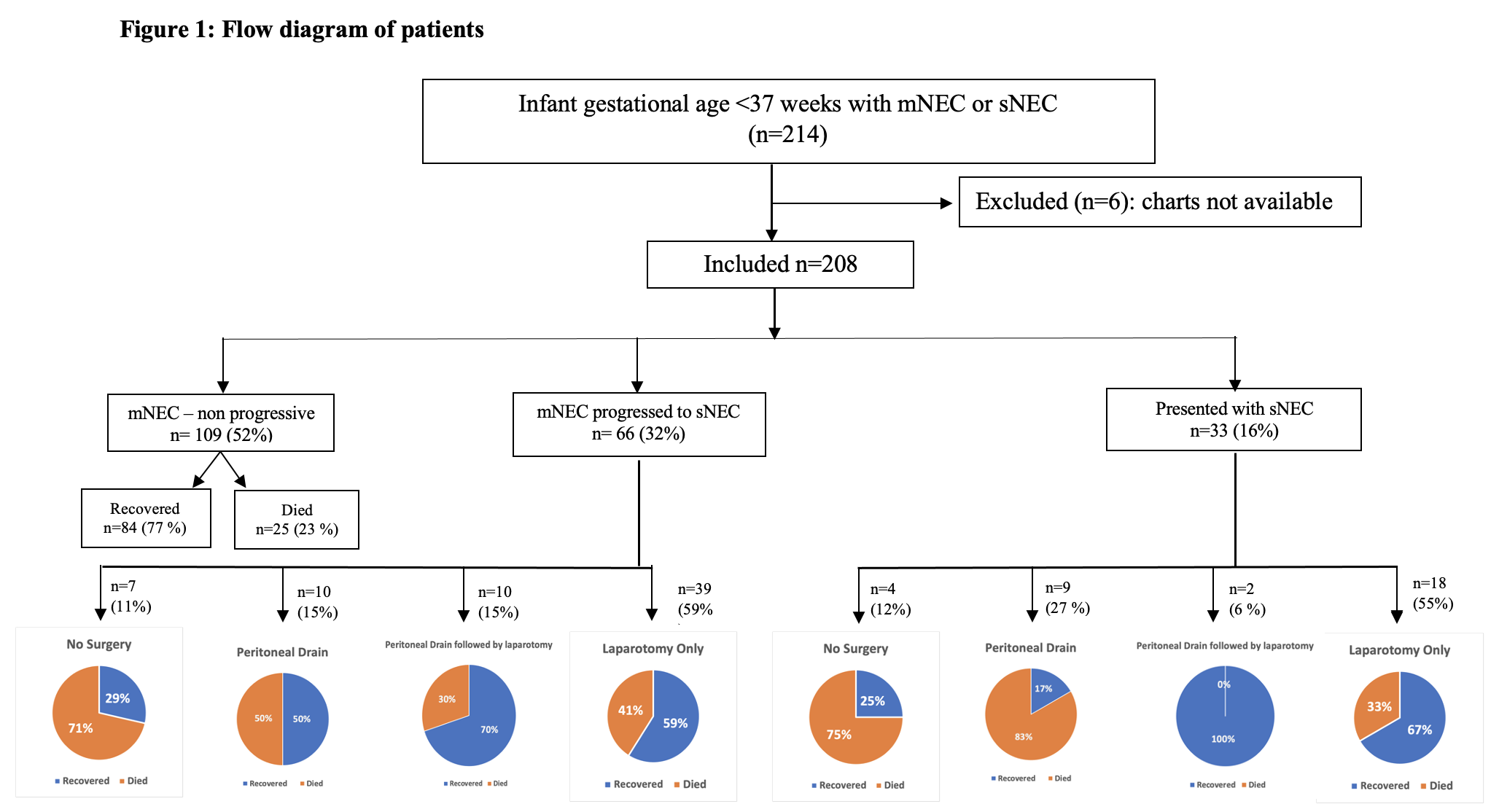
Table 1: Baseline characteristics of patients