Neonatal General
Category: Abstract Submission
Neonatology General 9: Congenital Anomalies - CV
302 - Earlier screening echocardiogram for patent ductus arteriosus in extremely preterm infants results in increased medical and surgical treatment
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 302
Publication Number: 302.441
Publication Number: 302.441
Kookjae Lee, Kapi'olani Medical Center for Women and Children, Honolulu, HI, United States; Min J. Hwang, Walter Reed National Military Medical Center, FALLS CHURCH, VA, United States; Lynn Iwamoto, University of Hawaii, John A. Burns School of Medicine, Honolulu, HI, United States
Kookjae Lee, MD
NICU Hospitalist
Kapi'olani Medical Center for Women and Children
Honolulu, Hawaii, United States
Presenting Author(s)
Background: Over the past decades, there have been major shifts in the management of patent ductus arteriosus (PDA) in preterm infants. Due to the lack of clear outcomes related to an open ductus, there is no national consensus for screening and treatment. At Kapiolani Medical Center for Women and Children (KMCWC), we started a quality improvement (QI) project to standardize the PDA management in preterm infants in 2018.
Objective: The main objective was to evaluate changes in management and clinical outcomes as a result of the practice standardization.
Design/Methods: The population included all infants born < 28 weeks GA admitted to the NICU at KMCWC who survived > 7 days. Retrospective chart review for demographics, type of treatment, and clinical outcomes was performed. Outcomes included treatment success, chronic lung disease (CLD), mortality, necrotizing enterocolitis (NEC), severe retinopathy of prematurity (ROP), and length of stay (LOS). Patients were grouped by year of birth, annual trends in outcomes were compared using one-way ANOVA with multiple comparisons or Chi-square analysis.
Results: From Jan 2018 – Jun 2021, 191 preterm infants < 28 weeks GA admitted to NICU survived more than 7 days. Annually from 2018 through the 1st half of 2021, there were no significant changes in mean GA (25 ± 1.5 weeks), birthweight (841 ± 229 g), gender (47% female), c-section delivery (68%), or percent outborn (9%) (all p > 0.05). Although the first echocardiogram was performed at a significantly earlier age (median 27 d [11-31] in 2018 vs 8.5 d [6-15] in 2021, p < 0.01, Figure 1), no difference was seen in the presence of PDA (p = 0.14); also, more infants received medical treatment (p < 0.01) (Figure 2) and underwent surgical ligation (3% in 2018 vs 17% in 2021, p = 0.04). There was no improvement in mortality, NEC, severe ROP, LOS or treatment success (all p > 0.05); however the rate of CLD/Death and CLD in survivors increased (p < 0.01) (Table 1). Conclusion(s): In summary, in this QI project, the decreased variation in practice led to earlier identification of PDAs in our extremely preterm infants. This was associated with increased medical and surgical treatment to attempt closure, however without a clear improvement in clinical outcomes and possibly worse CLD. Recent trends favor obtaining early echocardiograms in this population. Our findings suggest that a more targeted approach is needed to identify the infants who will benefit from early closure. As new technologies to treat the PDA are implemented, this continues to highlight the need for clinical equipoise.
Figure 1. Timing of screening echocardiogram in preterm infants less than 28 weeks.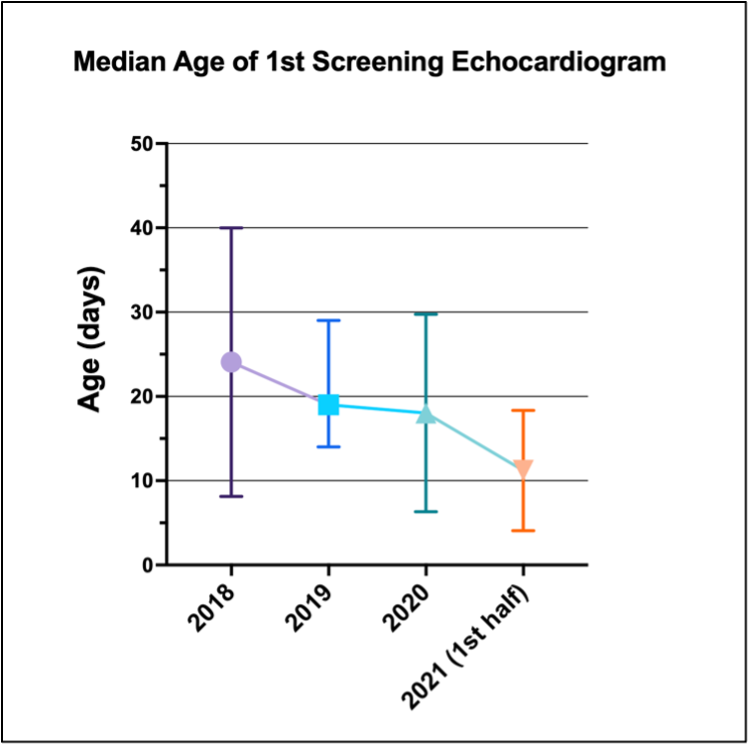 Symbols and error lines are presented as medians and interquartile ranges.
Symbols and error lines are presented as medians and interquartile ranges.
Figure 2. PDA cases and management changes from 2018 to 2021 1st half.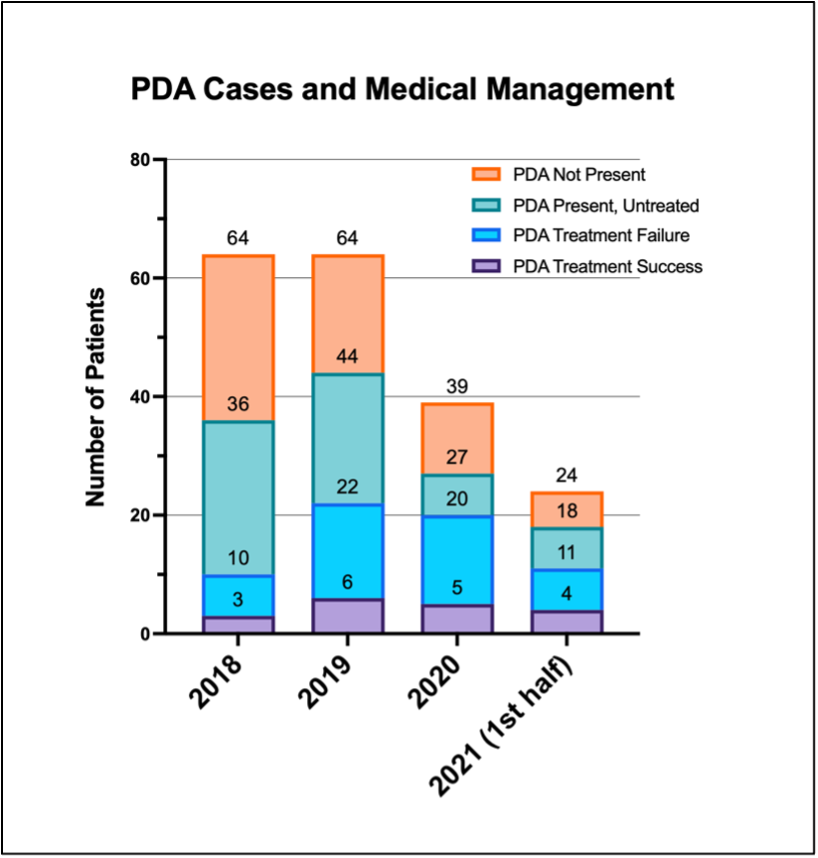 Annotations above bars are the stacked numbers of each group.
Annotations above bars are the stacked numbers of each group.
Objective: The main objective was to evaluate changes in management and clinical outcomes as a result of the practice standardization.
Design/Methods: The population included all infants born < 28 weeks GA admitted to the NICU at KMCWC who survived > 7 days. Retrospective chart review for demographics, type of treatment, and clinical outcomes was performed. Outcomes included treatment success, chronic lung disease (CLD), mortality, necrotizing enterocolitis (NEC), severe retinopathy of prematurity (ROP), and length of stay (LOS). Patients were grouped by year of birth, annual trends in outcomes were compared using one-way ANOVA with multiple comparisons or Chi-square analysis.
Results: From Jan 2018 – Jun 2021, 191 preterm infants < 28 weeks GA admitted to NICU survived more than 7 days. Annually from 2018 through the 1st half of 2021, there were no significant changes in mean GA (25 ± 1.5 weeks), birthweight (841 ± 229 g), gender (47% female), c-section delivery (68%), or percent outborn (9%) (all p > 0.05). Although the first echocardiogram was performed at a significantly earlier age (median 27 d [11-31] in 2018 vs 8.5 d [6-15] in 2021, p < 0.01, Figure 1), no difference was seen in the presence of PDA (p = 0.14); also, more infants received medical treatment (p < 0.01) (Figure 2) and underwent surgical ligation (3% in 2018 vs 17% in 2021, p = 0.04). There was no improvement in mortality, NEC, severe ROP, LOS or treatment success (all p > 0.05); however the rate of CLD/Death and CLD in survivors increased (p < 0.01) (Table 1). Conclusion(s): In summary, in this QI project, the decreased variation in practice led to earlier identification of PDAs in our extremely preterm infants. This was associated with increased medical and surgical treatment to attempt closure, however without a clear improvement in clinical outcomes and possibly worse CLD. Recent trends favor obtaining early echocardiograms in this population. Our findings suggest that a more targeted approach is needed to identify the infants who will benefit from early closure. As new technologies to treat the PDA are implemented, this continues to highlight the need for clinical equipoise.
Figure 1. Timing of screening echocardiogram in preterm infants less than 28 weeks.
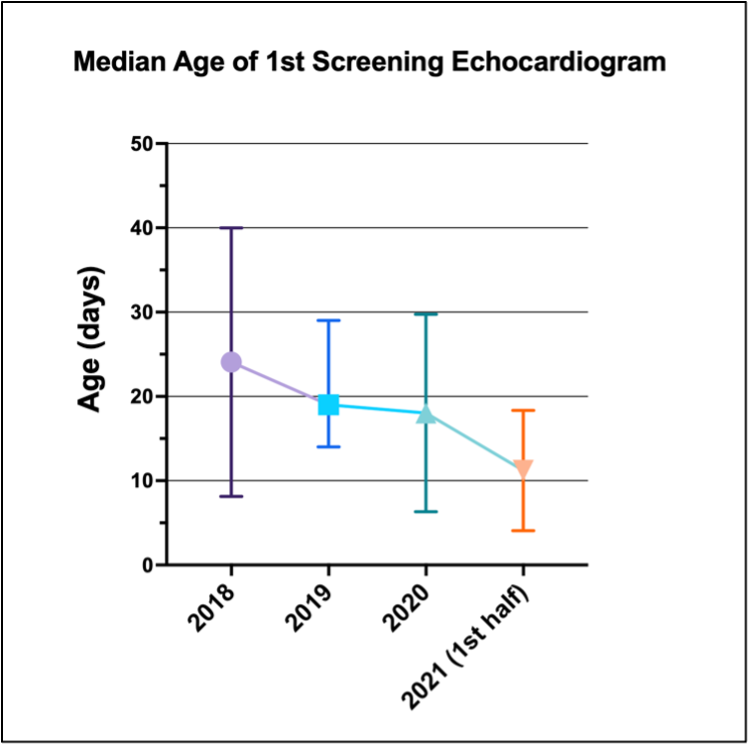 Symbols and error lines are presented as medians and interquartile ranges.
Symbols and error lines are presented as medians and interquartile ranges.Figure 2. PDA cases and management changes from 2018 to 2021 1st half.
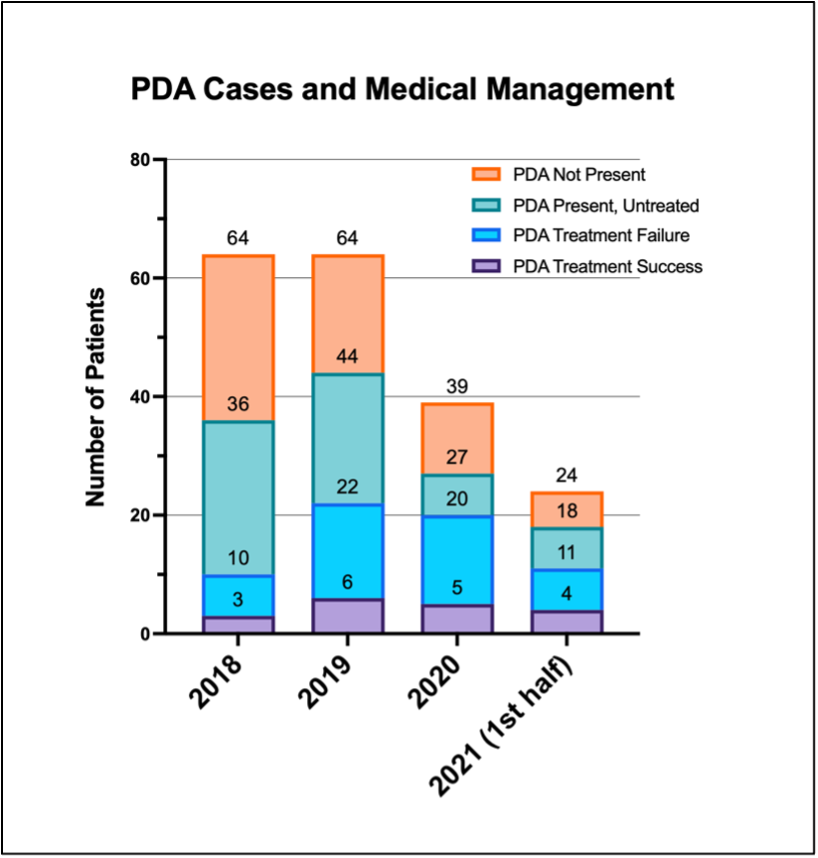 Annotations above bars are the stacked numbers of each group.
Annotations above bars are the stacked numbers of each group.