Back
General Pediatrics: Primary Care/Prevention
Category: Abstract Submission
General Pediatrics III
174 - Preparedness for Pediatric Offices Emergencies: A Simulation Primed Qualitative Inquiry of Pediatric Primary Care Staff’s Perspectives on Office Based Emergencies
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 174
Publication Number: 174.316
Publication Number: 174.316
Rabia N. Malik, Yale School of Medicine, New Haven, CT, United States; Hannah L. Anderson, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Erin E. Montgomery, Riley Hospital for Children/Indiana University School of Medicine, Indianapolis, IN, United States; Kamal Abulebda, Riley Hospital for Children at Indiana University Health, indianapolis, IN, United States; Marc Auerbach, Yale School of Medicine, Milford, CT, United States; Matthew Yuknis, Indiana University School of Medicine, Indinapolis, IN, United States

Gunjan Tiyyagura, MD, MHS (she/her/hers)
Associate Professor of Pediatrics
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Caring for pediatric patients with medical emergencies can be challenging for outpatient primary care providers (PCPs) and interprofessional primary care staff (ICPs). As these emergencies require basic care and stabilization prior to emergency medical service (EMS) arrival, PCPs should be able to provide initial care prior to transport to a local hospital. The variable frequency, poor predictability, and high-stakes nature of emergencies likely contribute to issues that have been reported in the office setting. However, other characteristics of PCPs and settings may contribute to emergency readiness and quality of emergency care; these barriers have been described using checklists but remain largely unexplored.
Objective: The aim of this study was to describe pediatric primary care staff’s perspectives on office-based emergencies.
Design/Methods: A multidisciplinary team including PCPs, ICPs, and administrative staff at participating office sites completed two simulated emergency cases based on the most common pediatric outpatient emergencies. After each simulation, a semi-scripted debrief was conducted. A total of 100 debriefs were conducted, one at each site for both simulation cases. We recorded, transcribed, and deidentified debriefings sampled from participating office sites in the study group. We employed thematic analysis, a qualitative method, to understand the salient information in our data set. Multiple coders identified codes independently, then reached consensus on a final list before creating themes based on codes and patterns of codes in the dataset.
Results: Fourteen debriefs were reviewed; we reached theoretical saturation after analyzing seven asthma and seven seizure debriefs. We identified four themes that were described as barriers to providing high quality emergency care. The most prevalent was the discomfort associated with emergencies in this setting. Another theme was communication with the EMS team: less communication was perceived as a barrier, but communication strategies such as calling sooner to facilitate a transfer, providing a more succinct but detailed sign out were helpful. Two more barriers were regarding resources needed for emergencies: lack of knowledge of both medication and equipment availability, accessibility, and directions for use.Conclusion(s): We identified four themes that were barriers to providing high-quality emergency care to pediatric patients in outpatient offices. Future work should explore these themes further and how emergency education and preparedness can target these themes to improve readiness for medical emergencies in this setting.
Office Site Demographics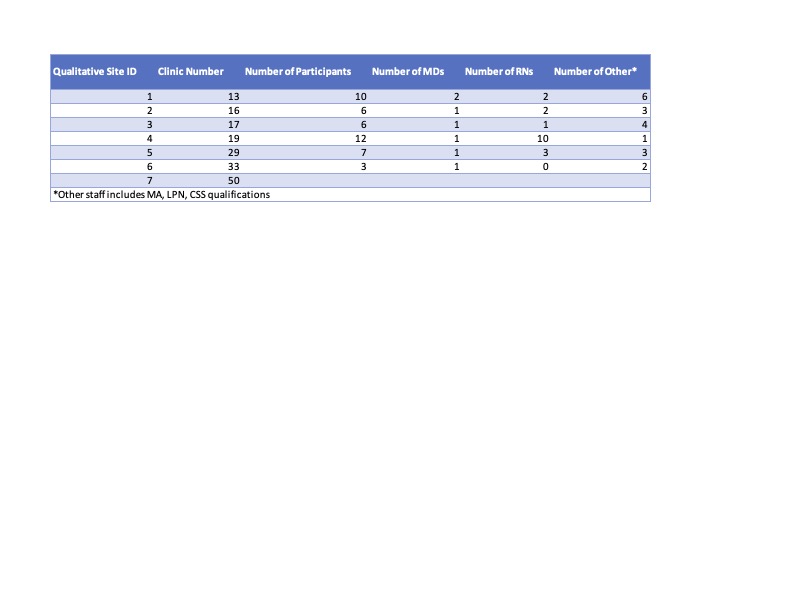 Demographics of participating study sites that were sampled for the analysis
Demographics of participating study sites that were sampled for the analysis
Objective: The aim of this study was to describe pediatric primary care staff’s perspectives on office-based emergencies.
Design/Methods: A multidisciplinary team including PCPs, ICPs, and administrative staff at participating office sites completed two simulated emergency cases based on the most common pediatric outpatient emergencies. After each simulation, a semi-scripted debrief was conducted. A total of 100 debriefs were conducted, one at each site for both simulation cases. We recorded, transcribed, and deidentified debriefings sampled from participating office sites in the study group. We employed thematic analysis, a qualitative method, to understand the salient information in our data set. Multiple coders identified codes independently, then reached consensus on a final list before creating themes based on codes and patterns of codes in the dataset.
Results: Fourteen debriefs were reviewed; we reached theoretical saturation after analyzing seven asthma and seven seizure debriefs. We identified four themes that were described as barriers to providing high quality emergency care. The most prevalent was the discomfort associated with emergencies in this setting. Another theme was communication with the EMS team: less communication was perceived as a barrier, but communication strategies such as calling sooner to facilitate a transfer, providing a more succinct but detailed sign out were helpful. Two more barriers were regarding resources needed for emergencies: lack of knowledge of both medication and equipment availability, accessibility, and directions for use.Conclusion(s): We identified four themes that were barriers to providing high-quality emergency care to pediatric patients in outpatient offices. Future work should explore these themes further and how emergency education and preparedness can target these themes to improve readiness for medical emergencies in this setting.
Office Site Demographics
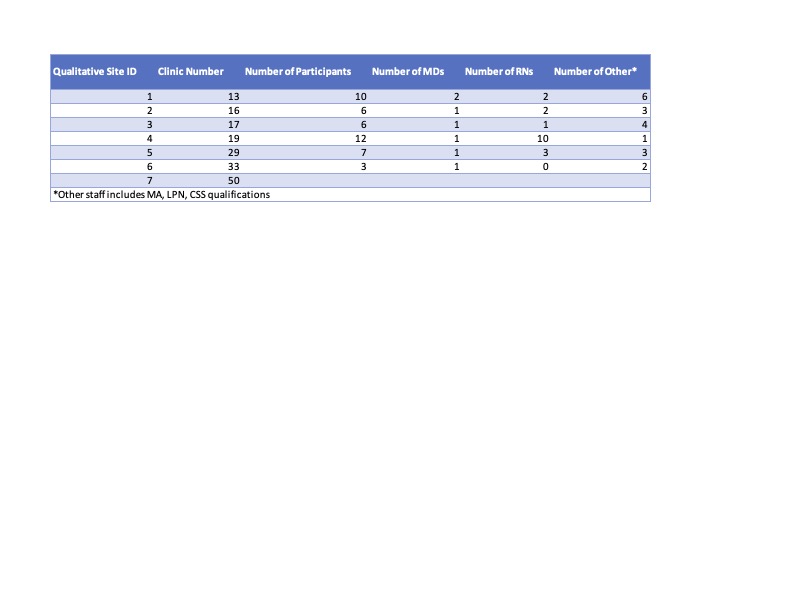 Demographics of participating study sites that were sampled for the analysis
Demographics of participating study sites that were sampled for the analysis