Back
Telemedicine/EHR/Medical Informatics
Category: Abstract Submission
Telemedicine/EHR/Medical Informatics II
298 - Implementing a Post-Discharge Telemedicine Visit to Improve Transition of Care from the NICU to Home in a Free Standing Children’s Hospital: A Pediatric Resident Quality Improvement Initiative.
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 298
Publication Number: 298.347
Publication Number: 298.347
Eric A. Tano, Nicklaus Children’s Hospital, Coral Gables, FL, United States; Pablo J. Napky Raudales, Nicklaus Children’s Hospital, Miami, FL, United States; Rodrigo Cardoso Cavalcante, Nicklaus Children’s Hospital, Miami, FL, United States; Larissa Romanow, Nicklaus Children’s Hospital, Miami, FL, United States; Ricardo Vega Auz, Nicklaus Children’s Hospital, Miami, FL, United States; Albert R. Tano, Kidz Medical Services, Coral Gables, FL, United States; Jorge E. Perez, Kidz Medical Services/Nicklaus Children's Hospital, Coral Gables, FL, United States; Magaly Diaz-Barbosa, Nicklaus Children's Hospital, Miami, FL, United States; Beatriz Cunill-De Sautu, Nicklaus Children’s Hospital, Miami, FL, United States; Adolfo Llanos-martinez, Nicklaus Children’s Hospital, Key Biscayne, FL, United States

Eric A. Tano, MD
Pediatric Resident
Nicklaus Children’s Hospital
Coral Gables, Florida, United States
Presenting Author(s)
Background:
Transition of care from the NICU to home generates significant issues that may lead not only to increase length of stay, but also higher post-discharge healthcare utilization. This transition is also recognized as a potentially high-risk time for errors and thus is a critical opportunity to address and promote patient safety and high-quality of care. Existing literature has demonstrated the benefits of using telemedicine after discharge from the NICU in achieving these goals.
Objective:
The medical team (neonatologist and pediatric resident) will conduct a post-discharge telemedicine visit (PDTV) with all patients discharged home from the NICU at Nicklaus Children’s Hospital (NCH) within a 24 to 72hr period.
Design/Methods: The NICU at NCH is a quaternary care unit located within a free standing Children’s Hospital. The unit is also currently participating in a quality improvement collaborative, “The Ins and Outs of Neonatal Care” sponsored by the Vermont Oxford Network, aimed at improving critical transition and clinical outcomes. The resident PDTV project was implemented in January 2021 and was designed to be aligned with the “Ins and Outs” project’s goal, primary and transition drivers (see figure 1). The PDTV project SMART aim is for the medical team (Neonatologist and Resident) to conduct a PDTV in 90% of infants within 24 to 72hr of being discharged home from the NICU. The telemedicine platform selected to conduct the video calls was Doxy.me. All caregivers were sent a satisfaction survey post PDTV.
Results:
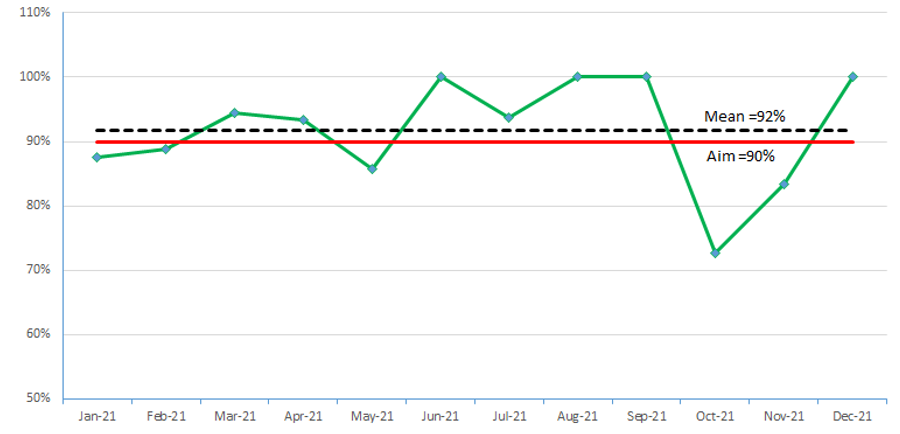
During the period of January to December 2021, a total of 143 PDTVs were conducted in 155 patients discharged home from the NICU. The run chart shown in figure 2 reveals the monthly rate of PDTV. In addition, the caregiver survey (n=63) showed that 95.2% were highly satisfied with the PDTV (Table 1).
Conclusion(s): A PDTV initiative using the Doxy.me platform was successfully implemented by the medical team and received high caregiver satisfaction results. The project positively contributed to the improvement in the transition from hospital to home by identifying and correcting gaps in caregiver’s education and by allowing the medical team to assess infant’s health condition after discharge. The PDTV has also been added to the interventions implemented for the VON “Ins and Outs” collaborative. Ongoing project goals include maintaining PDTV rates above SMART goal, identifying and discussing gaps in discharge planning with the NICU team, assessing impact on reducing post-discharge hospitalizations and visits to the ER, and improving the pediatric resident’s educational experience.
Figure 1. Key Driver Diagram: Post-Discharge Telemedicine.png) PDTV = Post-discharge telemedicine visit
PDTV = Post-discharge telemedicine visit
Figure 2. Run Chart of Post-Discharge Telemedicine Visits Conducted by Medical Team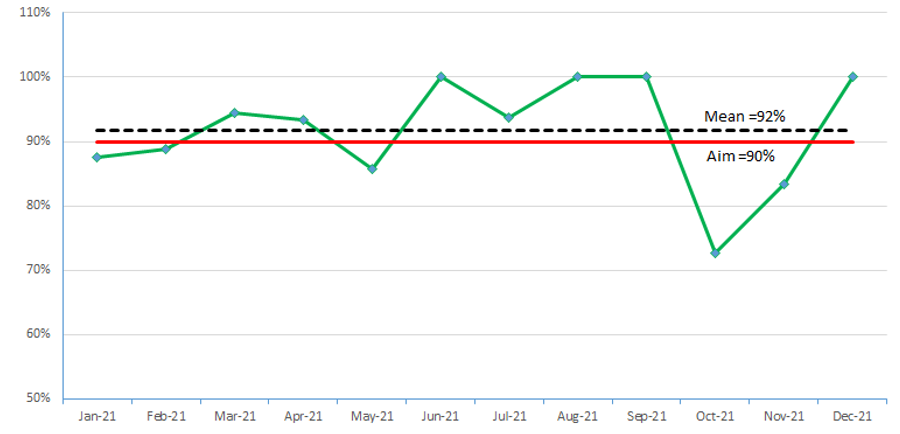
Transition of care from the NICU to home generates significant issues that may lead not only to increase length of stay, but also higher post-discharge healthcare utilization. This transition is also recognized as a potentially high-risk time for errors and thus is a critical opportunity to address and promote patient safety and high-quality of care. Existing literature has demonstrated the benefits of using telemedicine after discharge from the NICU in achieving these goals.
Objective:
The medical team (neonatologist and pediatric resident) will conduct a post-discharge telemedicine visit (PDTV) with all patients discharged home from the NICU at Nicklaus Children’s Hospital (NCH) within a 24 to 72hr period.
Design/Methods: The NICU at NCH is a quaternary care unit located within a free standing Children’s Hospital. The unit is also currently participating in a quality improvement collaborative, “The Ins and Outs of Neonatal Care” sponsored by the Vermont Oxford Network, aimed at improving critical transition and clinical outcomes. The resident PDTV project was implemented in January 2021 and was designed to be aligned with the “Ins and Outs” project’s goal, primary and transition drivers (see figure 1). The PDTV project SMART aim is for the medical team (Neonatologist and Resident) to conduct a PDTV in 90% of infants within 24 to 72hr of being discharged home from the NICU. The telemedicine platform selected to conduct the video calls was Doxy.me. All caregivers were sent a satisfaction survey post PDTV.
Results:
During the period of January to December 2021, a total of 143 PDTVs were conducted in 155 patients discharged home from the NICU. The run chart shown in figure 2 reveals the monthly rate of PDTV. In addition, the caregiver survey (n=63) showed that 95.2% were highly satisfied with the PDTV (Table 1).
Conclusion(s): A PDTV initiative using the Doxy.me platform was successfully implemented by the medical team and received high caregiver satisfaction results. The project positively contributed to the improvement in the transition from hospital to home by identifying and correcting gaps in caregiver’s education and by allowing the medical team to assess infant’s health condition after discharge. The PDTV has also been added to the interventions implemented for the VON “Ins and Outs” collaborative. Ongoing project goals include maintaining PDTV rates above SMART goal, identifying and discussing gaps in discharge planning with the NICU team, assessing impact on reducing post-discharge hospitalizations and visits to the ER, and improving the pediatric resident’s educational experience.
Figure 1. Key Driver Diagram: Post-Discharge Telemedicine
.png) PDTV = Post-discharge telemedicine visit
PDTV = Post-discharge telemedicine visitFigure 2. Run Chart of Post-Discharge Telemedicine Visits Conducted by Medical Team