Neonatal/Infant Resuscitation
Category: Abstract Submission
Neonatal/Infant Resuscitation III
501 - Utility of Low Apgar Score for Identifying Neonates with Short-term Morbidities in a Large Single Center Cohort
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 501
Publication Number: 501.232
Publication Number: 501.232
Henry Rozycki, Children's Hospital of Richmond at VCU, Richmond, VA, United States; Miheret Yitayew, Children's Hospital of Richmond, Richmond, VA, United States; Samuel Huang, Children's Hospital of Richmond at VCU, Basking Ridge, NJ, United States
Henry J. Rozycki, MD (he/him/his)
Vice-Chair
Children's Hospital of Richmond at VCU
Richmond, Virginia, United States
Presenting Author(s)
Background: Beyond simply assessing the newborn at delivery, the Apgar score is frequently used/studied as a risk factor for subsequent outcomes. Studies continue to indicate its association with long-term neurodevelopmental morbidities, but its utility as a predictor of significant short term neonatal morbidities is lacking. Despite this, all studies to modify or replace the Apgar score have used short-term outcomes.
Objective: The objective of this study was to examine the utility of the 1- and 5- minute Apgar score for identifying newborns at risk for clinically significant short-term morbidities.
Design/Methods: We conducted a retrospective study of data from infants with gestational age > 23 weeks born between 9/1/2013 and 3/30/2020 from a single academic medical center. Demographic data, 1- and 5-min Apgar scores, and discharge ICD-9 codes from initial hospitalization were retrieved. We focused on eight short-term morbidities: sepsis, hypoxic ischemic encephalopathy (HIE), transient tachypnea of the newborn (TTNB), respiratory distress syndrome (RDS), meconium aspiration syndrome (MAS), hypoglycemia, necrotizing enterocolitis (NEC) and intraventricular hemorrhage (IVH). Individual risks for each outcome were assessed by chi-square or t-test. Logistic regression modeling was performed and the contribution of Low (0-3) Apgar score determined by analyzing R2 values.
Results: Of the 17,080 infants born during the study period, complete data were available from 91% (15543). Low Apgars were recorded in 4.4% and 0.8% at 1 and 5-minutes. Outcomes frequency ranged from 0.3% for NEC and HIE to 6.8% for TTNB. All outcomes were associated with Low Apgar, with p values < 1-10. Table 1 shows that only a minority of infants had Low Apgar, especially at 5 mins. The number falsely identified by Low Apgar for each true case ranged from 3.7 (RDS, 5 min) to 41.7 (NEC at 5 min) (Table 2.) Logistic regression modeling demonstrated. Low Apgar score made negligible contributions to all the outcomes except HIE and to a lesser extent, RDS (Table 3). Conclusion(s): Using standard discharge codes in a large cohort of newborns, we found an Apgar score of 0-3, while statistically significant, would miss more than half of the affected infants, and have a high false positive rate, thereby over-identifying a substantial proportion of infants. These results reinforce concerns for relying on the score for individual patient selection in the short term.
Table 1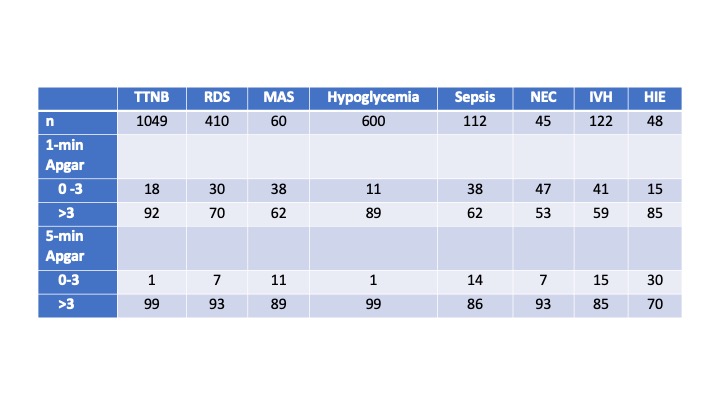 Incidence (n) and distribution (%) of low Apgar score in short-term morbidities.
Incidence (n) and distribution (%) of low Apgar score in short-term morbidities.
Table 2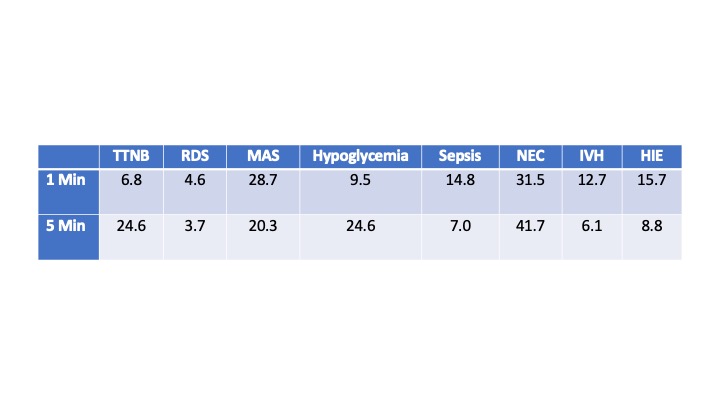 Ratio of false positive to true positive by Low Apgar for short-term outcomes
Ratio of false positive to true positive by Low Apgar for short-term outcomes
Objective: The objective of this study was to examine the utility of the 1- and 5- minute Apgar score for identifying newborns at risk for clinically significant short-term morbidities.
Design/Methods: We conducted a retrospective study of data from infants with gestational age > 23 weeks born between 9/1/2013 and 3/30/2020 from a single academic medical center. Demographic data, 1- and 5-min Apgar scores, and discharge ICD-9 codes from initial hospitalization were retrieved. We focused on eight short-term morbidities: sepsis, hypoxic ischemic encephalopathy (HIE), transient tachypnea of the newborn (TTNB), respiratory distress syndrome (RDS), meconium aspiration syndrome (MAS), hypoglycemia, necrotizing enterocolitis (NEC) and intraventricular hemorrhage (IVH). Individual risks for each outcome were assessed by chi-square or t-test. Logistic regression modeling was performed and the contribution of Low (0-3) Apgar score determined by analyzing R2 values.
Results: Of the 17,080 infants born during the study period, complete data were available from 91% (15543). Low Apgars were recorded in 4.4% and 0.8% at 1 and 5-minutes. Outcomes frequency ranged from 0.3% for NEC and HIE to 6.8% for TTNB. All outcomes were associated with Low Apgar, with p values < 1-10. Table 1 shows that only a minority of infants had Low Apgar, especially at 5 mins. The number falsely identified by Low Apgar for each true case ranged from 3.7 (RDS, 5 min) to 41.7 (NEC at 5 min) (Table 2.) Logistic regression modeling demonstrated. Low Apgar score made negligible contributions to all the outcomes except HIE and to a lesser extent, RDS (Table 3). Conclusion(s): Using standard discharge codes in a large cohort of newborns, we found an Apgar score of 0-3, while statistically significant, would miss more than half of the affected infants, and have a high false positive rate, thereby over-identifying a substantial proportion of infants. These results reinforce concerns for relying on the score for individual patient selection in the short term.
Table 1
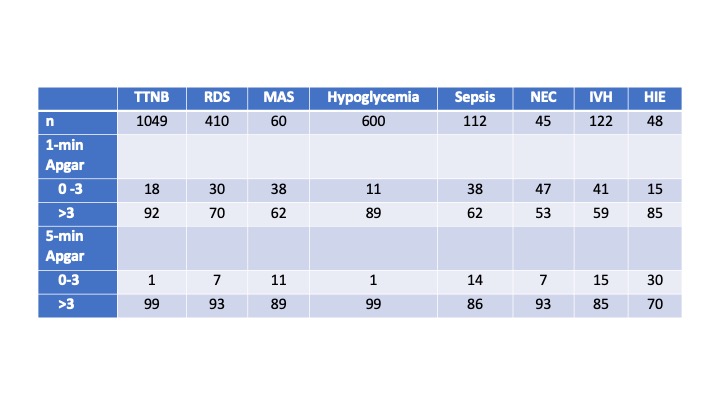 Incidence (n) and distribution (%) of low Apgar score in short-term morbidities.
Incidence (n) and distribution (%) of low Apgar score in short-term morbidities.Table 2
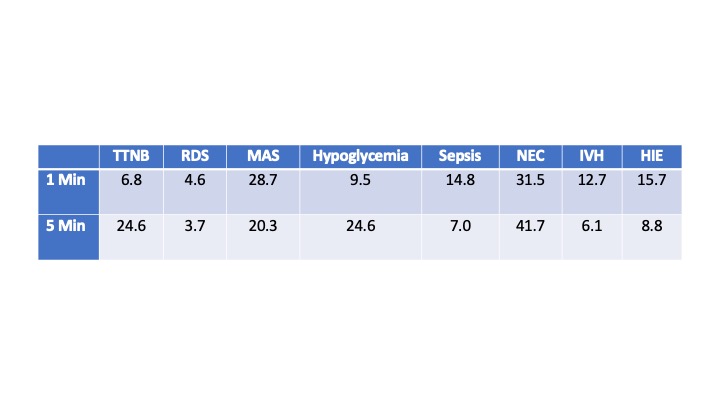 Ratio of false positive to true positive by Low Apgar for short-term outcomes
Ratio of false positive to true positive by Low Apgar for short-term outcomes