Hospital Medicine: Clinical
Category: Abstract Submission
Hospital Medicine: Clinical - Infectious Disease NOS
317 - Utilization Trends in Cerebrospinal Fluid Shunt Infection Prevention Techniques
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 317
Publication Number: 317.213
Publication Number: 317.213
Stacey Podkovik, Children's Hospital Los Angeles, Loma Linda, CA, United States; Chuan Zhou, Seattle Children's Research Institute, Seattle, WA, United States; Susan Coffin, Childrens' Hospital of Philadelphia, Philadelphia, PA, United States; Matthew Hall, Children's Hospital Association, Lenexa, Kansas, KS, United States; Jason Hauptman, University of Washington School of Medicine, Seattle, WA, United States; Matthew Kronman, University of Washington School of Medicine, Seattle, WA, United States; Francesco T. Mangano, CCHMC, Cincinnati, OH, United States; Ian Pollack, University of Pittsburgh, Pittsburgh, PA, United States; Sabrina Sedano, Children's Hospital Los Angeles, Los Angeles, CA, United States; Joshua K. Schaffzin, MD PhD, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Emily A. Thorell, University of Utah School of Medicine, Salt Lake City, UT, United States; Benjamin Warf, MD, Harvard Medical School/Boston Children’s Hospital, Boston, MA, United States; Kathryn B. Whitlock, New Harmony Statistical Consulting LLC, Clinton, WA, United States; Tamara D. Simon, Children's Hospital Los Angeles, Los Angeles, CA, United States
- SP
Stacey Podkovik, D.O.
Resident Physician
Riverside University Health System
Loma Linda, California, United States
Presenting Author(s)
Background: Cerebrospinal fluid (CSF) shunts allow children with hydrocephalus to survive and avoid ongoing brain injury; however, they are associated with revision surgeries and risk of infection. The Hydrocephalus Clinical Research Network (HCRN) instituted quality improvement protocols to decrease infection rates: intrathecal (IT) antibiotics between 2007-2009, followed by antibiotic impregnated catheters (AIC) in 2012-2013. However, no large-scale studies have compared the effectiveness of routine pre-operative prophylactic intravenous antibiotics (standard care) and these infection prevention techniques to each other.
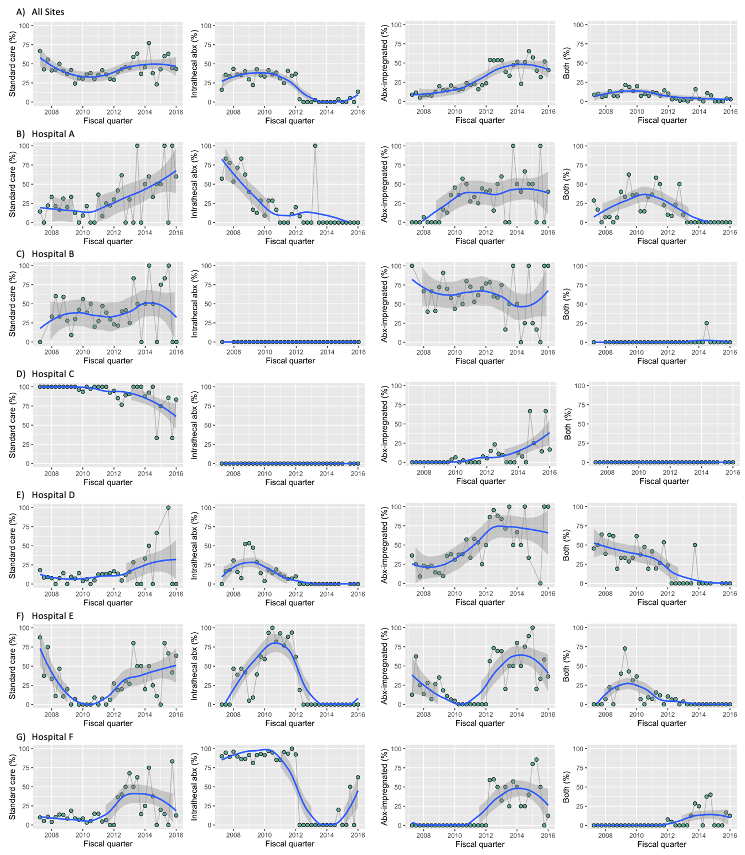
Objective: Ascertain trends over time in the utilization of infection prevention techniques (standard care, IT antibiotics, AIC, and both IT antibiotics and AIC) and infection rates among participating hospitals.
Design/Methods: This study is a retrospective observational cohort at 6 large children’s hospitals between 2007 and 2015. The study population includes children ≤ 18 years of age who underwent initial shunt placement between 2007 and 2012. Pediatric Health Information System + (PHIS+) data were augmented with chart review data for all shunt surgeries that occurred prior to the first shunt infection. The primary outcome was shunt infection within 6 months of prior surgery using the HCRN definition. Infection rates and 95% confidence intervals were generated overall, by hospital, by year, and by infection prevention technique. Pearson chi-square test was used to test for differences.
Results: A total of 1,752 eligible children had initial shunt placement between 2007-2012, with a total of 3,138 shunt surgeries through 2015. Differences were noted between hospitals in gestational age, etiology of hydrocephalus, and race and ethnicity, but not gender, weight at surgery and previous surgeries (Table 1). Utilization of infection prevention techniques varied across participating hospitals (Figure 2). HCRN hospitals used more IT antibiotics in 2007-2011, and most hospitals saw increasing adoption of AIC after 2012. A total of 129 shunt infections occurred within 6 months of placement. No significant differences were observed in infection rates between the hospitals (p =0.059) and between infection prevention techniques (p =0.5), but a significant difference was observed across years (p =0.004)(Table 2). Conclusion(s): Differences in use of shunt infection prevention techniques vary across children’s hospitals, with recent increases seen in the use of AICs. No difference in infection rates was observed, but additional adjustment for difference over time and between hospitals is warranted.
Table 1: Demographic characteristics of entire cohort of children (n=1752), overall and by hospital.png)
Figure 1: Trends over time in the utilization of infection prevention techniques (standard care, IT antibiotics, AIC, and both), overall and by hospital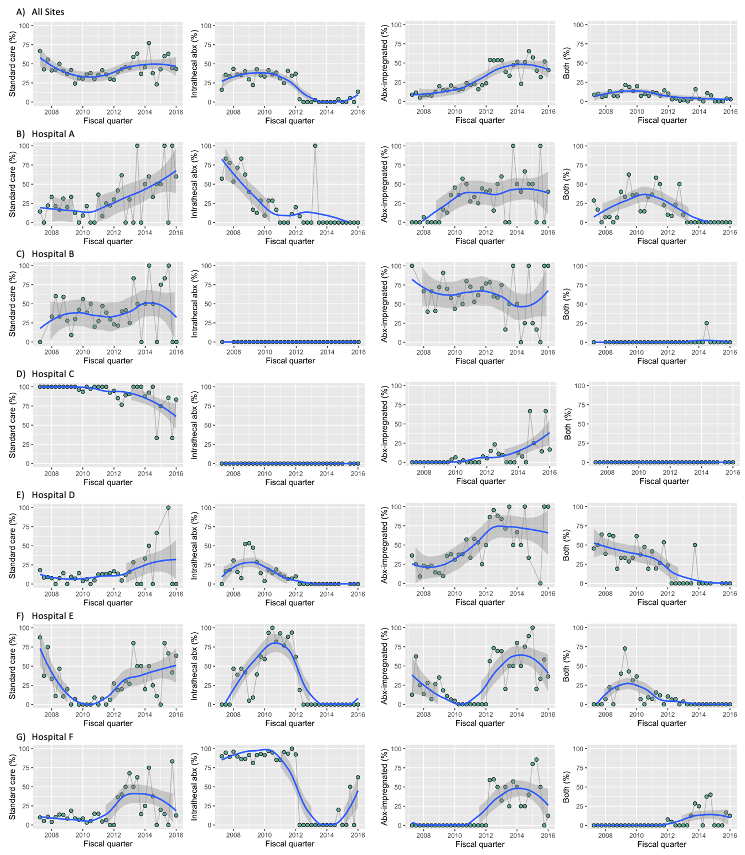
Objective: Ascertain trends over time in the utilization of infection prevention techniques (standard care, IT antibiotics, AIC, and both IT antibiotics and AIC) and infection rates among participating hospitals.
Design/Methods: This study is a retrospective observational cohort at 6 large children’s hospitals between 2007 and 2015. The study population includes children ≤ 18 years of age who underwent initial shunt placement between 2007 and 2012. Pediatric Health Information System + (PHIS+) data were augmented with chart review data for all shunt surgeries that occurred prior to the first shunt infection. The primary outcome was shunt infection within 6 months of prior surgery using the HCRN definition. Infection rates and 95% confidence intervals were generated overall, by hospital, by year, and by infection prevention technique. Pearson chi-square test was used to test for differences.
Results: A total of 1,752 eligible children had initial shunt placement between 2007-2012, with a total of 3,138 shunt surgeries through 2015. Differences were noted between hospitals in gestational age, etiology of hydrocephalus, and race and ethnicity, but not gender, weight at surgery and previous surgeries (Table 1). Utilization of infection prevention techniques varied across participating hospitals (Figure 2). HCRN hospitals used more IT antibiotics in 2007-2011, and most hospitals saw increasing adoption of AIC after 2012. A total of 129 shunt infections occurred within 6 months of placement. No significant differences were observed in infection rates between the hospitals (p =0.059) and between infection prevention techniques (p =0.5), but a significant difference was observed across years (p =0.004)(Table 2). Conclusion(s): Differences in use of shunt infection prevention techniques vary across children’s hospitals, with recent increases seen in the use of AICs. No difference in infection rates was observed, but additional adjustment for difference over time and between hospitals is warranted.
Table 1: Demographic characteristics of entire cohort of children (n=1752), overall and by hospital
.png)
Figure 1: Trends over time in the utilization of infection prevention techniques (standard care, IT antibiotics, AIC, and both), overall and by hospital