Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine VI
360 - Point-of-Care Ultrasound Interpretation of Cardiac Standstill in Children
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 360
Publication Number: 360.205
Publication Number: 360.205
Evan Yanni, Hassenfeld Children's Hospital at NYU Langone, Brooklyn, NY, United States; James W. Tsung, Icahn School of Medicine at Mount Sinai, New York, NY, United States; Kevin Hu, Icahn School of Medicine at Mount Sinai, New York, NY, United States; Ee Tay, NYU Langone Health, New York, NY, United States

Evan Yanni, MD
Pediatric Emergency Medicine Fellow
Hassenfeld Children's Hospital at NYU Langone
Brooklyn, New York, United States
Presenting Author(s)
Background:
Use of point-of-care ultrasound (POCUS) to diagnose cardiac standstill and guide continuation of cardiac resuscitation has gained widespread use in adult patients and is becoming more prevalent in pediatric patients. Previous studies have demonstrated moderate inter-observer agreement among physicians using POCUS to diagnose cardiac standstill during cardiac arrests in adult patients. There is limited data regarding POCUS interpretation of cardiac standstill among pediatric patients during cardiac resuscitations.
Objective:
This study seeks to determine the level of inter-observer agreement among Pediatric Emergency Medicine (PEM) physicians when interpreting POCUS for cardiac standstill in pediatric patients during cardiac arrest as well as highlight factors that may contribute to lack of agreement.
Design/Methods:
A single, nation-wide, cross-sectional, convenience sample survey was administered to PEM attendings and fellows between Feb - Jun of 2021. PEM attendings with ≥ 25 cardiac ultrasound scans were considered “proficient” based on POCUS competency set by the American College of Emergency Physicians. The survey contained 11 unique 6-second video clips of cardiac POCUS performed during pulseless arrests in pediatric patients and asked the respondents to determine which clips represented cardiac standstill. A description of each clip is found in Table 1. The level of inter-observer agreement was determined using Krippendorff’s alpha (K alpha) coefficient for PEM attendings with ≥ 25 scans, PEM attendings with 1-24 scans, PEM attendings with 0 scans, PEM fellows with ≥ 25 scans, and PEM fellows with 1-24 scans. K alpha ≥ 0.800 is determined as good agreement and a K alpha ≤ 0.667 is considered an unacceptable level of agreement.
Results:
263 PEM physicians completed the survey. Respondent demographics are found in Table 2. Agreement among subgroups is found in Table 3. PEM attendings with ≥ 25 scans had moderate agreement (K alpha = 0.740). PEM fellows with ≥ 25 scans had good agreement (K alpha = 0.811). PEM attendings with no prior ultrasound experience had lack of acceptable agreement (K alpha = 0.630). Highest divergence in responses included clips displaying minimal wall or valve motion as well as swirling blood in an otherwise static heart.
Conclusion(s):
There is moderate inter-observer agreement interpreting pediatric cardiac standstill on POCUS during cardiac resuscitations among PEM attendings who are considered proficient. Minimal cardiac structural movements during POCUS may influence interpretation. Cardiac POCUS may be a useful tool to guide resuscitation efforts in pediatric patients.
Table 1. Interpretation of each clip by study authors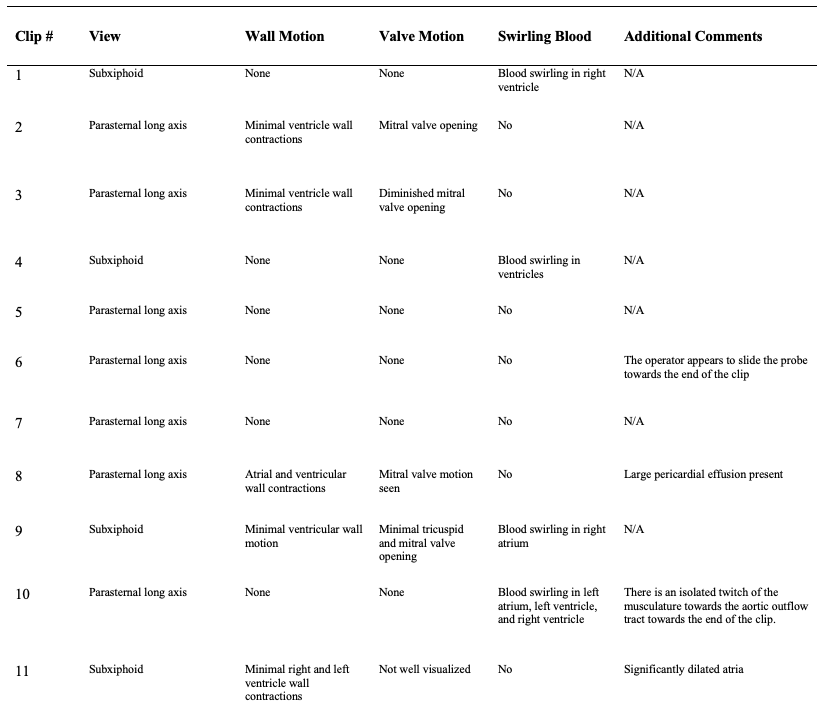
Table 2. Respondent Demographics.jpg)
Use of point-of-care ultrasound (POCUS) to diagnose cardiac standstill and guide continuation of cardiac resuscitation has gained widespread use in adult patients and is becoming more prevalent in pediatric patients. Previous studies have demonstrated moderate inter-observer agreement among physicians using POCUS to diagnose cardiac standstill during cardiac arrests in adult patients. There is limited data regarding POCUS interpretation of cardiac standstill among pediatric patients during cardiac resuscitations.
Objective:
This study seeks to determine the level of inter-observer agreement among Pediatric Emergency Medicine (PEM) physicians when interpreting POCUS for cardiac standstill in pediatric patients during cardiac arrest as well as highlight factors that may contribute to lack of agreement.
Design/Methods:
A single, nation-wide, cross-sectional, convenience sample survey was administered to PEM attendings and fellows between Feb - Jun of 2021. PEM attendings with ≥ 25 cardiac ultrasound scans were considered “proficient” based on POCUS competency set by the American College of Emergency Physicians. The survey contained 11 unique 6-second video clips of cardiac POCUS performed during pulseless arrests in pediatric patients and asked the respondents to determine which clips represented cardiac standstill. A description of each clip is found in Table 1. The level of inter-observer agreement was determined using Krippendorff’s alpha (K alpha) coefficient for PEM attendings with ≥ 25 scans, PEM attendings with 1-24 scans, PEM attendings with 0 scans, PEM fellows with ≥ 25 scans, and PEM fellows with 1-24 scans. K alpha ≥ 0.800 is determined as good agreement and a K alpha ≤ 0.667 is considered an unacceptable level of agreement.
Results:
263 PEM physicians completed the survey. Respondent demographics are found in Table 2. Agreement among subgroups is found in Table 3. PEM attendings with ≥ 25 scans had moderate agreement (K alpha = 0.740). PEM fellows with ≥ 25 scans had good agreement (K alpha = 0.811). PEM attendings with no prior ultrasound experience had lack of acceptable agreement (K alpha = 0.630). Highest divergence in responses included clips displaying minimal wall or valve motion as well as swirling blood in an otherwise static heart.
Conclusion(s):
There is moderate inter-observer agreement interpreting pediatric cardiac standstill on POCUS during cardiac resuscitations among PEM attendings who are considered proficient. Minimal cardiac structural movements during POCUS may influence interpretation. Cardiac POCUS may be a useful tool to guide resuscitation efforts in pediatric patients.
Table 1. Interpretation of each clip by study authors
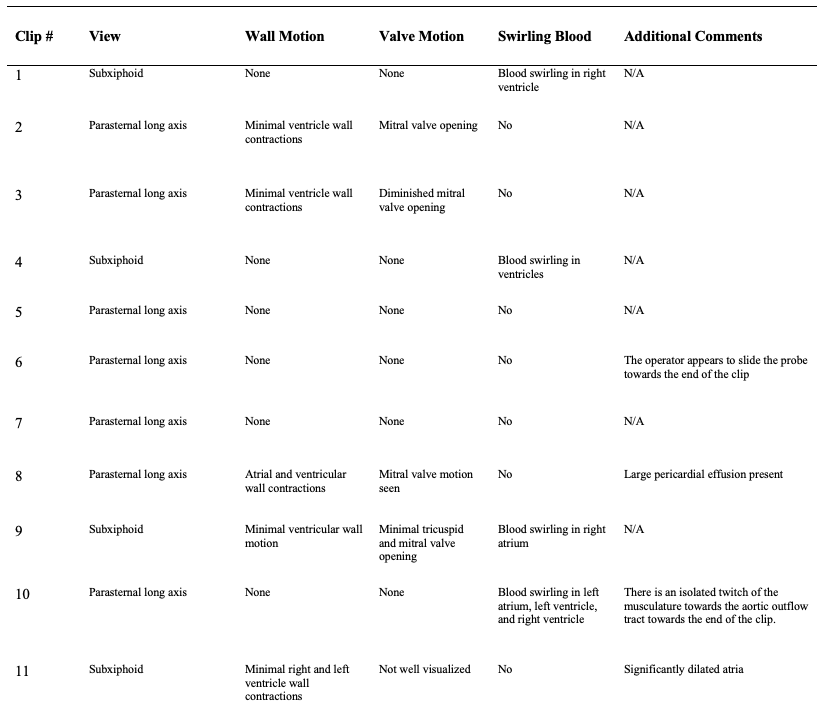
Table 2. Respondent Demographics
.jpg)
