Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement III: GI and Nutrition
243 - Reducing Spontaneous Intestinal Perforation Among Extremely Preterm Infants: A Quality Improvement Initiative
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 243
Publication Number: 243.128
Publication Number: 243.128
Mary Silverberg, University of Alabama at Birmingham, Birmingham, AL, United States; Samuel Gentle, UAB, Birmingham, AL, United States; Ariel Salas, UAB, Birmingham, AL, United States; Namasivayam Ambalavanan, University of Alabama School of Medicine, Birmingham, AL, United States; Waldemar A. Carlo, University of Alabama at Birmingham, Birmingham, AL, United States; Colm P. Travers, University of Alabama at Birmingham, Birmingham, AL, United States

Mary Silverberg, MD (she/her/hers)
Fellow
University of Alabama School of Medicine
Birmingham, Alabama, United States
Presenting Author(s)
Background: Postnatal indomethacin prophylaxis decreases severe IVH but increases the risk of spontaneous intestinal perforation (SIP) among extremely preterm infants. Our center utilized single dose indomethacin prophylaxis as part of a bundle of care for extremely preterm infants.
Objective: We undertook a quality improvement initiative due to concerns of SIP. Our SMART aim was to decrease the rate of SIP among extremely preterm infants by 50% within 12 months.
Design/Methods: We included infants from 22w 0d to 27w 6d inborn from July 2019 to September 2021. We excluded infants with a birth weight less than 400 grams and those with congenital anomalies. The primary outcome was the rate of SIP analyzed via statistical process control charts to detect special cause variation. Balancing measures included the rate of severe IVH in the first week after birth. Process measures included the use of indomethacin prophylaxis, standardized electronic medical record order-sets, and antenatal indomethacin use.
Results: We included 259 patients, 117 pre-intervention and 142 post-intervention, with a mean gestational age of 25w 4d ± 12d and birth weight of 759 ± 222 grams. The pre-intervention rate of SIP was 6.8% and post-intervention rate of SIP is 4.2%. There have been 52 consecutive infants since the last case of SIP with no special cause variation detected on P-chart analysis (Figure 1). T-chart analysis also did not indicate special cause variation in the number of days between cases of SIP. The use of postnatal indomethacin prophylaxis went from 82.1% to 4.3%, which was an absolute decrease of 77.8% (p < 0.001). The risk of severe IVH (pre-intervention = 16.1%, post intervention=8.8%, p=0.11) and severe IVH or death in the first week after birth (pre-intervention=20.5%, post-intervention= 12.9%, p=0.16) did not differ between epochs. Exposure to antenatal indomethacin occurred in 21.0% of the cohort.Conclusion(s): Despite successfully decreasing the use of postnatal indomethacin prophylaxis we did not identify a special cause variation in the incidence of SIP. Future interventions in this ongoing quality improvement initiative will include decreasing exposure to antenatal indomethacin.
Figure 1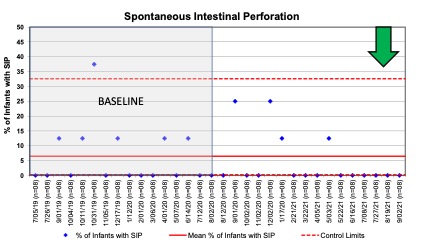 P-chart showing rate of spontaneous intestinal perforation (SIP) among extremely preterm infants. The baseline rate of SIP was 6.8% with no special cause variation detected. Routine postnatal indomethacin prophylaxis was discontinued in August 2020.
P-chart showing rate of spontaneous intestinal perforation (SIP) among extremely preterm infants. The baseline rate of SIP was 6.8% with no special cause variation detected. Routine postnatal indomethacin prophylaxis was discontinued in August 2020.
Objective: We undertook a quality improvement initiative due to concerns of SIP. Our SMART aim was to decrease the rate of SIP among extremely preterm infants by 50% within 12 months.
Design/Methods: We included infants from 22w 0d to 27w 6d inborn from July 2019 to September 2021. We excluded infants with a birth weight less than 400 grams and those with congenital anomalies. The primary outcome was the rate of SIP analyzed via statistical process control charts to detect special cause variation. Balancing measures included the rate of severe IVH in the first week after birth. Process measures included the use of indomethacin prophylaxis, standardized electronic medical record order-sets, and antenatal indomethacin use.
Results: We included 259 patients, 117 pre-intervention and 142 post-intervention, with a mean gestational age of 25w 4d ± 12d and birth weight of 759 ± 222 grams. The pre-intervention rate of SIP was 6.8% and post-intervention rate of SIP is 4.2%. There have been 52 consecutive infants since the last case of SIP with no special cause variation detected on P-chart analysis (Figure 1). T-chart analysis also did not indicate special cause variation in the number of days between cases of SIP. The use of postnatal indomethacin prophylaxis went from 82.1% to 4.3%, which was an absolute decrease of 77.8% (p < 0.001). The risk of severe IVH (pre-intervention = 16.1%, post intervention=8.8%, p=0.11) and severe IVH or death in the first week after birth (pre-intervention=20.5%, post-intervention= 12.9%, p=0.16) did not differ between epochs. Exposure to antenatal indomethacin occurred in 21.0% of the cohort.Conclusion(s): Despite successfully decreasing the use of postnatal indomethacin prophylaxis we did not identify a special cause variation in the incidence of SIP. Future interventions in this ongoing quality improvement initiative will include decreasing exposure to antenatal indomethacin.
Figure 1
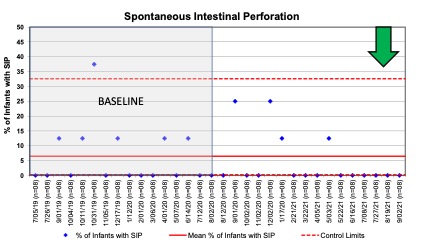 P-chart showing rate of spontaneous intestinal perforation (SIP) among extremely preterm infants. The baseline rate of SIP was 6.8% with no special cause variation detected. Routine postnatal indomethacin prophylaxis was discontinued in August 2020.
P-chart showing rate of spontaneous intestinal perforation (SIP) among extremely preterm infants. The baseline rate of SIP was 6.8% with no special cause variation detected. Routine postnatal indomethacin prophylaxis was discontinued in August 2020.