Critical Care
Category: Abstract Submission
3: Critical Care I
24 - Impact of Maternal Oxygenation On Fetal Hypoxia: Lessons For COVID in Pregnancy
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 24
Publication Number: 24.102
Publication Number: 24.102
Nithi Fernandes, Children's Hospital of Michigan, Northville, MI, United States; Praveen Chandrasekharan, Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, Buffalo, NY, United States; Munmun Rawat, University at Buffalo, Buffalo, NY, United States; Sylvia Gugino, SUNY at Buffalo, Buffalo, NY, United States; Satyan Lakshminrusimha, University of California Davis Children's Hospital, Sacramento, CA, United States
- NF
Nithi Fernandes, MD (she/her/hers)
Neonatologist
Children's Hospital of Michigan
Detroit, Michigan, United States
Presenting Author(s)
Background: COVID-19 during pregnancy increases the risk of hypoxemia from severe acute respiratory distress syndrome as coronavirus ARDSnet practice guidelines recommend PaO2 55-80mmHg during management of non-pregnant adults. However, there are still limited data available on optimal maternal oxygenation parameters to avoid fetal hypoxia. The Society for Maternal Fetal Medicine (SNFM) recommends higher oxygen targets in pregnant mothers with COVID compared to non-pregnant adults.
Objective: Our objective was to compare the effects of decreasing maternal oxygen tension on fetal hemodynamics, oxygenation and brain oxygen delivery in lambs.
Design/Methods: Partially exteriorized 37 near-term fetal lambs were instrumented with catheters in the right carotid artery, and jugular vein, and flow probes around left carotid and pulmonary arteries. Gases were obtained from fetal vessels simultaneously with maternal carotid artery while periodically increasing maternal inspired oxygen from FiO2 of 0.1 in steps to 1.0. Hemoglobin was monitored from the fetal blood gases to calculate oxygen delivery to the brain, inferred from fetal carotid flow data. Maternal and fetal pulse oximetry were also monitored. Using non-parametric statistics, comparisons of the data were made between maternal PaO2 levels of < 55mmHg, 55-80mmHg and >80mmHg. Ewes were ventilated with different FiO2 values for 15-20 minutes each to achieve these PaO2 levels (Table 1).
Results: Historical data from spontaneously breathing ewes shows fetal umbilical arterial PaO2 values to be 22.8±1.2 mmHg (shaded area in Figure 1C). The median PaO2 and FiO2 levels in the three levels of maternal PaO2 are shown in table 1. There were significant decreases in fetal PaO2 and SpO2 when maternal PaO2 was reduced from >80mmHg to 55-80 mmHg (Figure 1). Decreasing maternal PaO2 < 55 mmHg resulted in a further drop in fetal PaO2. Fetal brain oxygen delivery did not significantly decrease when maternal PaO2 decreased from >80mmHg to 55-80 but dropped when maternal PaO2 was < 55 mmHg.Conclusion(s): Fetal PaO2 and oxygen delivery to the brain improves when maternal PaO2 increases from < 55 to >80mmHg. In the setting of lung disease of pregnancy such as COVID-19, it may be advisable to administer supplemental oxygen to the mother to maintain PaO2 slightly higher than that recommended by ARDSnet for non-pregnant adults to optimize fetal oxygen delivery and supports the current recommendations of Society for Maternal Fetal Medicine.
Figure 1..jpg) Maternal oxygen tension with A. Fetal oxygen delivery, B. Fetal pulse oximetry and C. Fetal oxygen tension.
Maternal oxygen tension with A. Fetal oxygen delivery, B. Fetal pulse oximetry and C. Fetal oxygen tension.
Table 1.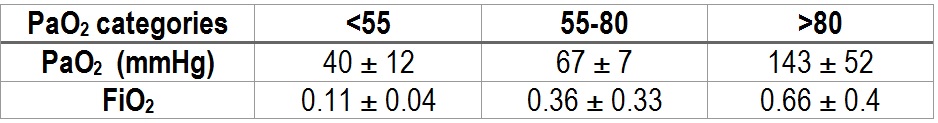 Mean and standard deviation for ranges in maternal PaO2 for FiO2
Mean and standard deviation for ranges in maternal PaO2 for FiO2
Objective: Our objective was to compare the effects of decreasing maternal oxygen tension on fetal hemodynamics, oxygenation and brain oxygen delivery in lambs.
Design/Methods: Partially exteriorized 37 near-term fetal lambs were instrumented with catheters in the right carotid artery, and jugular vein, and flow probes around left carotid and pulmonary arteries. Gases were obtained from fetal vessels simultaneously with maternal carotid artery while periodically increasing maternal inspired oxygen from FiO2 of 0.1 in steps to 1.0. Hemoglobin was monitored from the fetal blood gases to calculate oxygen delivery to the brain, inferred from fetal carotid flow data. Maternal and fetal pulse oximetry were also monitored. Using non-parametric statistics, comparisons of the data were made between maternal PaO2 levels of < 55mmHg, 55-80mmHg and >80mmHg. Ewes were ventilated with different FiO2 values for 15-20 minutes each to achieve these PaO2 levels (Table 1).
Results: Historical data from spontaneously breathing ewes shows fetal umbilical arterial PaO2 values to be 22.8±1.2 mmHg (shaded area in Figure 1C). The median PaO2 and FiO2 levels in the three levels of maternal PaO2 are shown in table 1. There were significant decreases in fetal PaO2 and SpO2 when maternal PaO2 was reduced from >80mmHg to 55-80 mmHg (Figure 1). Decreasing maternal PaO2 < 55 mmHg resulted in a further drop in fetal PaO2. Fetal brain oxygen delivery did not significantly decrease when maternal PaO2 decreased from >80mmHg to 55-80 but dropped when maternal PaO2 was < 55 mmHg.Conclusion(s): Fetal PaO2 and oxygen delivery to the brain improves when maternal PaO2 increases from < 55 to >80mmHg. In the setting of lung disease of pregnancy such as COVID-19, it may be advisable to administer supplemental oxygen to the mother to maintain PaO2 slightly higher than that recommended by ARDSnet for non-pregnant adults to optimize fetal oxygen delivery and supports the current recommendations of Society for Maternal Fetal Medicine.
Figure 1.
.jpg) Maternal oxygen tension with A. Fetal oxygen delivery, B. Fetal pulse oximetry and C. Fetal oxygen tension.
Maternal oxygen tension with A. Fetal oxygen delivery, B. Fetal pulse oximetry and C. Fetal oxygen tension.Table 1.
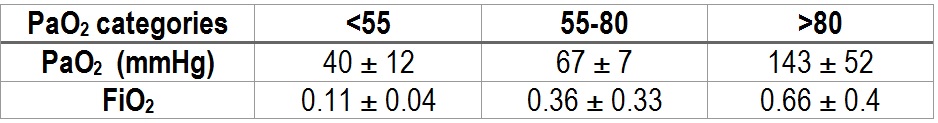 Mean and standard deviation for ranges in maternal PaO2 for FiO2
Mean and standard deviation for ranges in maternal PaO2 for FiO2