Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up I
447 - Impact of Social Determinants of Health on Follow Up for Neonates Requiring Neurocritical Care
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 447
Publication Number: 447.121
Publication Number: 447.121
Beatrice Stefanescu, Riley Hospital for Children at Indiana University Health, Indianapolis,, IN, United States; Andrei Stefanescu, Independent Investigator, River Ridge, LA, United States; Isabella T. Eiler, Riley Hospital for Children at Indiana University Health, Indianapolis, IN, United States
- SH
Susan Henderson, MA, CPXP (she/her/hers)
Director of NICU Parent Support
Indiana University School of Medicine
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Long-term neurodevelopmental outcomes of infants requiring neurocritical care depend on the effectiveness of follow up clinic visits scheduled after discharge from the hospital.
Objective: The study objective was to evaluate the impact of social determinants of health (SDH) on attrition rates for 1st clinic follow-up visit of infants who required neonatal neurocritical care.
Design/Methods: Our retrospective cohort study was conducted in a level IV neonatal intenstive care unit from November 2013 to December 2019. Infants with at least one diagnosis in the ICD-10 diagnostic group associated with a neurologic condition requiring neurocritical care were eligible. Patients were divided into “Show” and “No Show” groups based on 1st neurodevelopmental follow up visit.
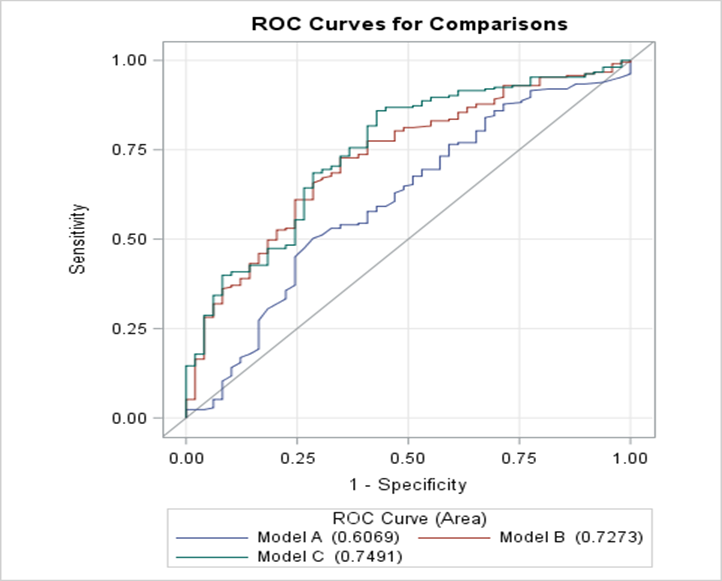
Results: Of 565 infants who has a follow-up visit scheduled, 111 (19.6%) were “no show” (Figure 1). Most common reason for no show was infant rehospitalization (40%), followed by rescheduling with other appointments (25%). Baseline infant characteristics and demographics in the two study groups are shown in Table 1. Three SDH predictive models of attrition to 1st follow-up visit were developed: Model A predictors included gestational age, respiratory and feeding type at discharge, Model B includes Model A predictors plus maternal education and health insurance, and Model C includes Model B indicators plus marital status, driving distance, driving time, employment status, and median household income in zip code of residence (Figure 2). Of the three models, Model B significantly improves predictive power over Model A (p=0.007). Model C does not significantly improve predictive power over Model B (p=0.34).Conclusion(s): This is the first study to explore the impact of SDH factors on attrition to 1st follow-up visit of infants who needed neurocritical care. It showed that greater driving distance and time were associated with increased attrition risk. Our findings suggest socio-economic disparity impacted the ability to follow-up. Our model analysis demonstrated that SDH inclusive of maternal education and type of health insurance can be used to predict attrition at follow-up. We plan to further explore how knowledge gained from this study can fuel future interventions to improve outpatient clinic operations and strategies to expand access to care. Further research on SDH factors that influence attrition to follow-up need to be further characterized to argue for improved resource allocation.
Figure 1. Study flowchart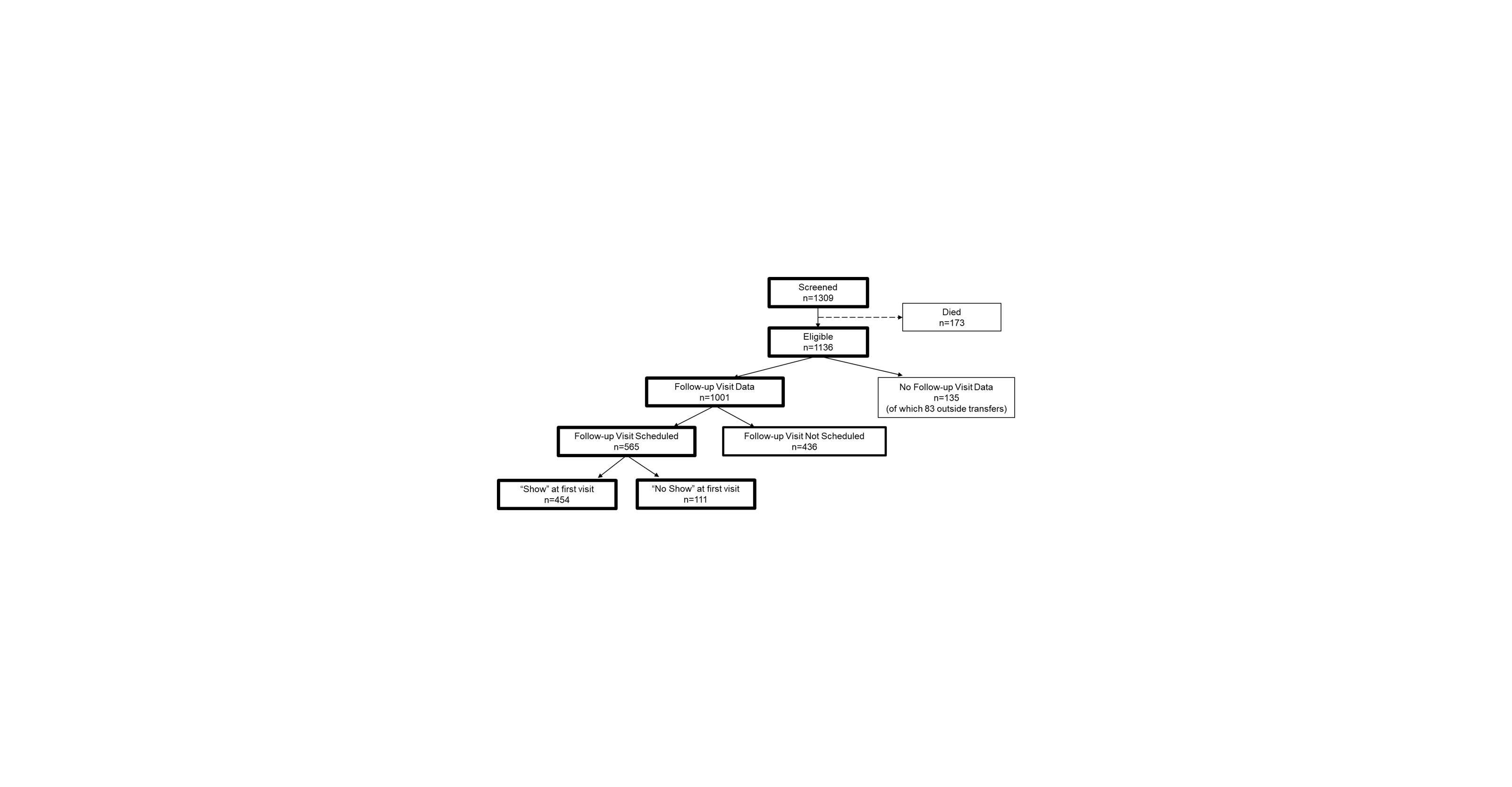
Figure 2. Receiver Operating Characteristics (ROC) curves and Area Under the Curve (AUC) values for three predictive models. Model A predictors include gestational age, not on room air at discharge, and feeding at discharge other than PO or PONG. Model B includes Model A predictors plus maternal education and health insurance. Model C includes Model B indicators plus marital status, driving distance, driving time, employment status, and median household income in zip code of residence.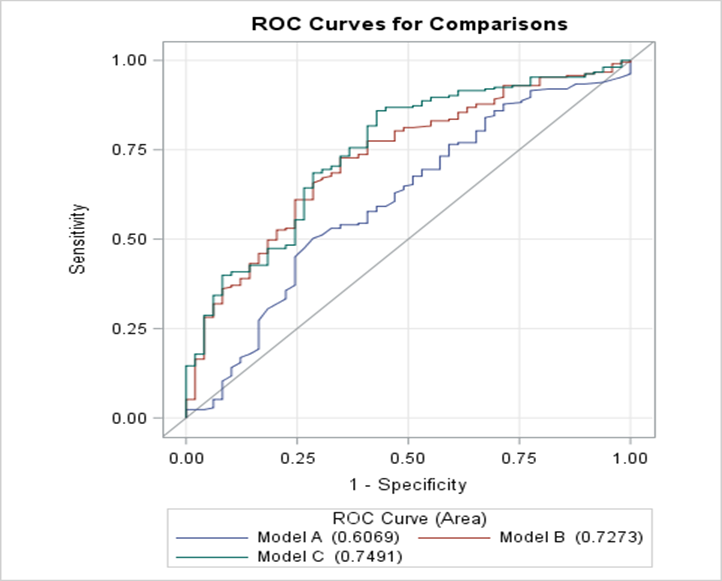
Objective: The study objective was to evaluate the impact of social determinants of health (SDH) on attrition rates for 1st clinic follow-up visit of infants who required neonatal neurocritical care.
Design/Methods: Our retrospective cohort study was conducted in a level IV neonatal intenstive care unit from November 2013 to December 2019. Infants with at least one diagnosis in the ICD-10 diagnostic group associated with a neurologic condition requiring neurocritical care were eligible. Patients were divided into “Show” and “No Show” groups based on 1st neurodevelopmental follow up visit.
Results: Of 565 infants who has a follow-up visit scheduled, 111 (19.6%) were “no show” (Figure 1). Most common reason for no show was infant rehospitalization (40%), followed by rescheduling with other appointments (25%). Baseline infant characteristics and demographics in the two study groups are shown in Table 1. Three SDH predictive models of attrition to 1st follow-up visit were developed: Model A predictors included gestational age, respiratory and feeding type at discharge, Model B includes Model A predictors plus maternal education and health insurance, and Model C includes Model B indicators plus marital status, driving distance, driving time, employment status, and median household income in zip code of residence (Figure 2). Of the three models, Model B significantly improves predictive power over Model A (p=0.007). Model C does not significantly improve predictive power over Model B (p=0.34).Conclusion(s): This is the first study to explore the impact of SDH factors on attrition to 1st follow-up visit of infants who needed neurocritical care. It showed that greater driving distance and time were associated with increased attrition risk. Our findings suggest socio-economic disparity impacted the ability to follow-up. Our model analysis demonstrated that SDH inclusive of maternal education and type of health insurance can be used to predict attrition at follow-up. We plan to further explore how knowledge gained from this study can fuel future interventions to improve outpatient clinic operations and strategies to expand access to care. Further research on SDH factors that influence attrition to follow-up need to be further characterized to argue for improved resource allocation.
Figure 1. Study flowchart
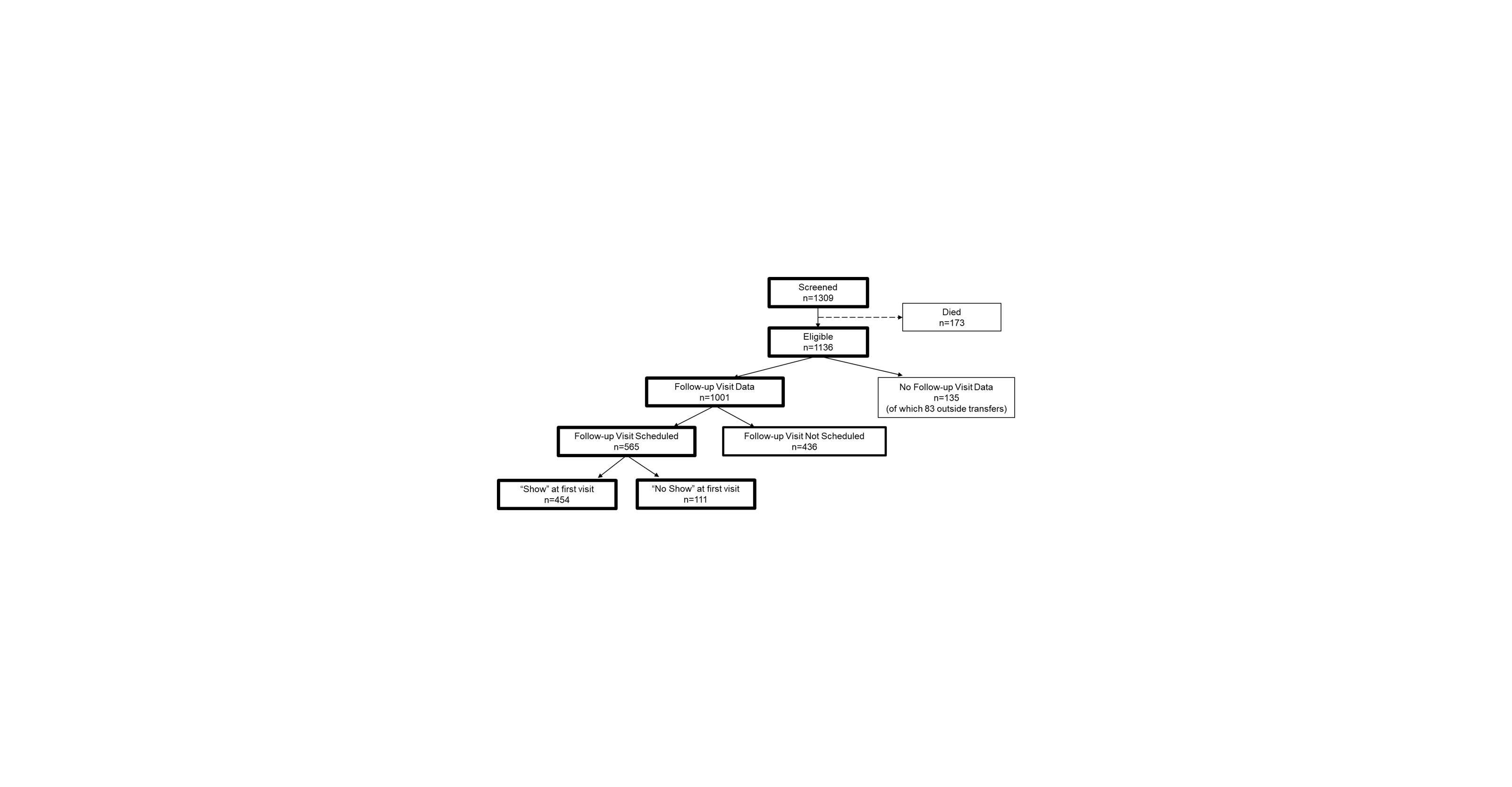
Figure 2. Receiver Operating Characteristics (ROC) curves and Area Under the Curve (AUC) values for three predictive models. Model A predictors include gestational age, not on room air at discharge, and feeding at discharge other than PO or PONG. Model B includes Model A predictors plus maternal education and health insurance. Model C includes Model B indicators plus marital status, driving distance, driving time, employment status, and median household income in zip code of residence.