Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine IV
81 - Impact of the COVID-19 Pandemic on Emergency Department Visits for High-risk Conditions and Associated Complications in a Statewide Pediatric Emergency Network
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 81
Publication Number: 81.106
Publication Number: 81.106
Courtney W. Mangus, University of Michigan Medical School, Ann Arbor, MI, United States; Sarah J. Parker, University of Michigan Medical School, Ann Arbor, MI, United States; Amy DeLaroche, Children's Hospital of Michigan, Detroit, MI, United States; Julia Hays, Henry Ford Health System, Detroit, MI, United States; Stephen Gunnink, Spectrum Health Helen DeVos Children's Hospital, Grand Rapids, MI, United States; Erica A. Michiels, Helen DeVos Children's Hospital, Ada, MI, United States; Prashant Mahajan, University of Michigan Medical School, Ann Arbor, MI, United States; Michigan Pediatric Emergency Research Network, University of Michigan Medical School, Ann Arbor, MI, United States
Courtney W. Mangus, MD (she/her/hers)
Assistant Professor
University of Michigan Medical School
Ann arbor, Michigan, United States
Presenting Author(s)
Background: The COVID-19 pandemic has affected emergency department (ED) patient volumes and the epidemiology of ED visits. The impact of the pandemic on the frequency and complications of certain high-risk conditions is unknown.
Objective: To determine the frequency of 16 high-risk conditions and associated complications in a Michigan state-wide network of academic and community EDs (MiPEM) during the COVID-19 pandemic.
Design/Methods: We conducted a cross-sectional study of pediatric (age 0-21 years) ED visits among a network of 5 Michigan health systems comprising 10 EDs during pre-pandemic (3/1/19-3/10/20) and pandemic (3/11/20-3/31/21) periods. Data from all pediatric visits were collected from the electronic medical record and included patient demographics, ED visit characteristics (chief complaint, emergency severity index [ESI] triage level, mode of arrival, disposition), procedure codes, and encounter final International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) diagnosis codes. Selection of ICD-10-CM codes for high-risk conditions and associated diagnostic complications were identified using previously described methods. Statistical hypothesis tests were assessed for significance using chi-squared and Fisher’s exact tests at a two-tailed alpha of 0.05.
Results: 522,998 visits were analyzed (71% pre pandemic, 29% pandemic). ED volumes decreased overall during the pandemic, but visits during this period had a higher proportion of high-acuity visits (ESI Triage Level 1-3 vs. Level 4-5, p < 0.001), deaths in the ED (p < 0.001) and ED arrivals by ambulance, medical flight, or police (p < 0.001) when compared to pre-pandemic visits. The proportion of patients presenting with select high-risk conditions (appendicitis, bacterial meningitis, diabetic ketoacidosis, intussusception, myocarditis, ovarian & testicular torsion, sepsis, septic arthritis, stroke, and others) was higher in the pandemic period compared to pre-pandemic (p < 0.01). No statistically significant increases in the frequency of complications during the pandemic period compared to pre-pandemic period were identified.Conclusion(s): Pandemic ED visits were lower in volume but higher in acuity compared to pre-pandemic visits. Despite a higher proportion of ED visits due to high-risk conditions, there was no increase in complications, suggesting minimal impact of the pandemic in outcomes of pediatric ED visits.
Table. 1 Patient and Visit Demographics for Michigan Pediatric Emergency Department Encounters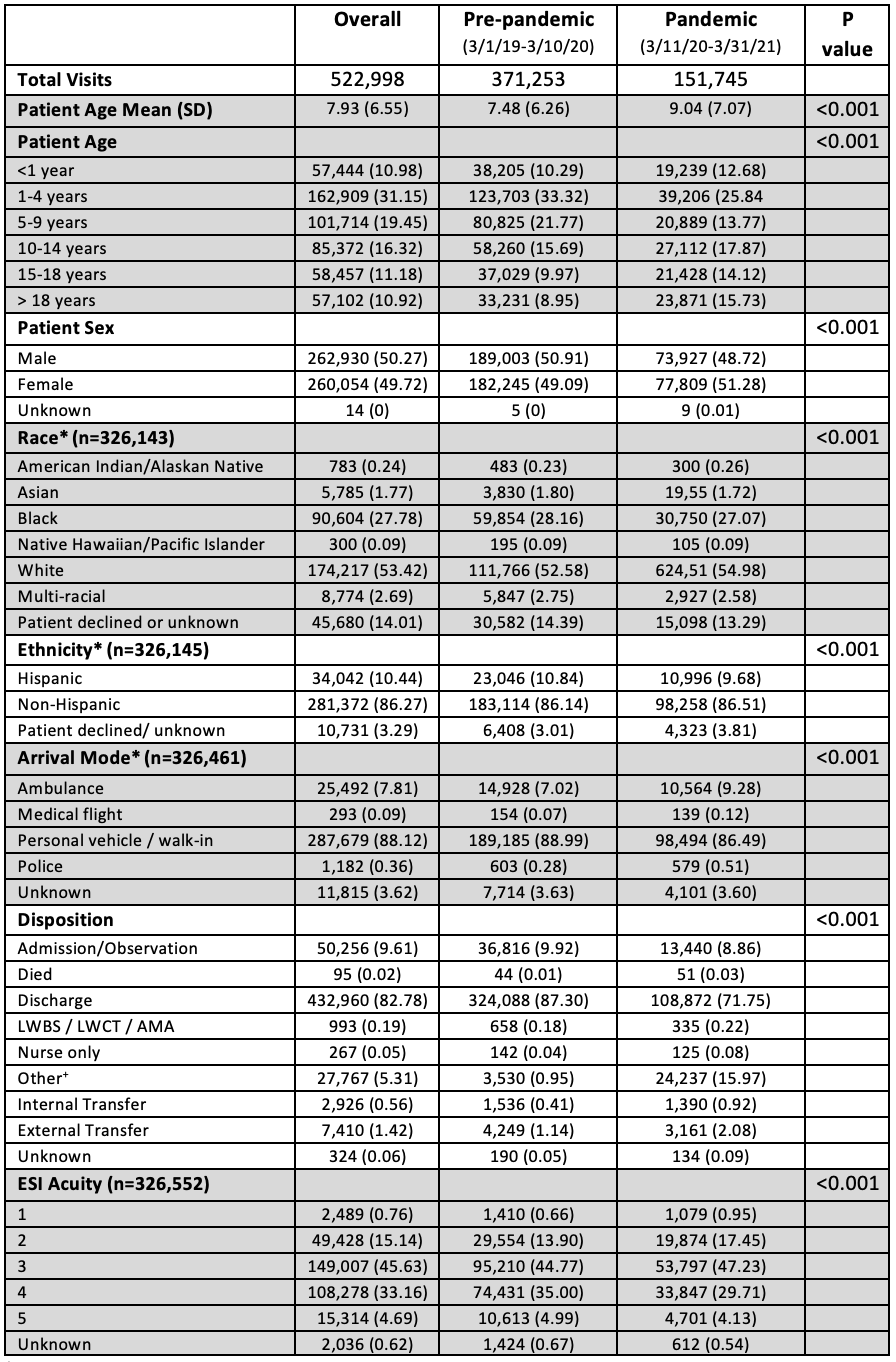 * Incomplete data, 4/5 participating sites reporting.
* Incomplete data, 4/5 participating sites reporting.
LWBS: Left without being seen; LWCT: Left without completion of treatment; AMA: Against Medical Advice
ESI: Emergency Severity Index.
+Other: Elected to go to urgent care, unknown other, send to safe center
Table 2. Frequency of High-Risk Conditions Diagnosed in the Pre-Pandemic and Pandemic Periods.png)
Objective: To determine the frequency of 16 high-risk conditions and associated complications in a Michigan state-wide network of academic and community EDs (MiPEM) during the COVID-19 pandemic.
Design/Methods: We conducted a cross-sectional study of pediatric (age 0-21 years) ED visits among a network of 5 Michigan health systems comprising 10 EDs during pre-pandemic (3/1/19-3/10/20) and pandemic (3/11/20-3/31/21) periods. Data from all pediatric visits were collected from the electronic medical record and included patient demographics, ED visit characteristics (chief complaint, emergency severity index [ESI] triage level, mode of arrival, disposition), procedure codes, and encounter final International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) diagnosis codes. Selection of ICD-10-CM codes for high-risk conditions and associated diagnostic complications were identified using previously described methods. Statistical hypothesis tests were assessed for significance using chi-squared and Fisher’s exact tests at a two-tailed alpha of 0.05.
Results: 522,998 visits were analyzed (71% pre pandemic, 29% pandemic). ED volumes decreased overall during the pandemic, but visits during this period had a higher proportion of high-acuity visits (ESI Triage Level 1-3 vs. Level 4-5, p < 0.001), deaths in the ED (p < 0.001) and ED arrivals by ambulance, medical flight, or police (p < 0.001) when compared to pre-pandemic visits. The proportion of patients presenting with select high-risk conditions (appendicitis, bacterial meningitis, diabetic ketoacidosis, intussusception, myocarditis, ovarian & testicular torsion, sepsis, septic arthritis, stroke, and others) was higher in the pandemic period compared to pre-pandemic (p < 0.01). No statistically significant increases in the frequency of complications during the pandemic period compared to pre-pandemic period were identified.Conclusion(s): Pandemic ED visits were lower in volume but higher in acuity compared to pre-pandemic visits. Despite a higher proportion of ED visits due to high-risk conditions, there was no increase in complications, suggesting minimal impact of the pandemic in outcomes of pediatric ED visits.
Table. 1 Patient and Visit Demographics for Michigan Pediatric Emergency Department Encounters
 * Incomplete data, 4/5 participating sites reporting.
* Incomplete data, 4/5 participating sites reporting.LWBS: Left without being seen; LWCT: Left without completion of treatment; AMA: Against Medical Advice
ESI: Emergency Severity Index.
+Other: Elected to go to urgent care, unknown other, send to safe center
Table 2. Frequency of High-Risk Conditions Diagnosed in the Pre-Pandemic and Pandemic Periods
.png)
