Palliative Care
Category: Abstract Submission
Palliative Care I
512 - Characteristics of Critically Ill Infants at the End of Life in the Neonatal Intensive Care Unit: A 10-year Chart Review
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 512
Publication Number: 512.140
Publication Number: 512.140
Christine A. Fortney, Ohio State University College of Nursing, Columbus, OH, United States; Amy E. Baughcum, Nationwide Children's Hospital, Columbus, OH, United States; Adrien M. Winning, Loyola University Chicago, Chicago, IL, United States; Dana Garcia, Nationwide Children's Hospital, Columbus, OH, United States; Lisa H. Humphrey, Nationwide Children's Hospital, Columbus, OH, United States; Nicole Cistone, ohio state universitsy, MECHANICSBURG, OH, United States; Emily L. Moscato, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Madelaine C. Keim, University of Washington, Seattle, WA, United States; Cynthia Gerhardt, Nationwide Children's Hospital, Columbus, OH, United States

Christine A. Fortney, PhD, RN
Assistant Professor
Ohio State University College of Nursing
Columbus, Ohio, United States
Presenting Author(s)
Background: Each year in the U.S., about 16,000 infants die in the neonatal intensive care unit (NICU). These infants often experience invasive medical treatments and high symptom burden throughout hospitalization as curative treatments continue until it is clear that the infant will not survive. Thus, it is crucial to identify and better understand the characteristics of critically ill infants (e.g., diagnoses, treatments, symptoms) so that symptom assessment and management may be optimized.
Objective: To characterize the demographic, clinical, and symptom characteristics of infants who died in the NICU.
Design/Methods: Retrospective electronic medical record (EMR) review of 476 infants who died in a large, Midwestern level IV NICU during admission to a NICU between July 1, 2009 and June 30, 2019. Demographic information, diagnosis, treatment, and EOL characteristics were extracted from each infant’s EMR by trained research assistants using a standardized form developed for the study.
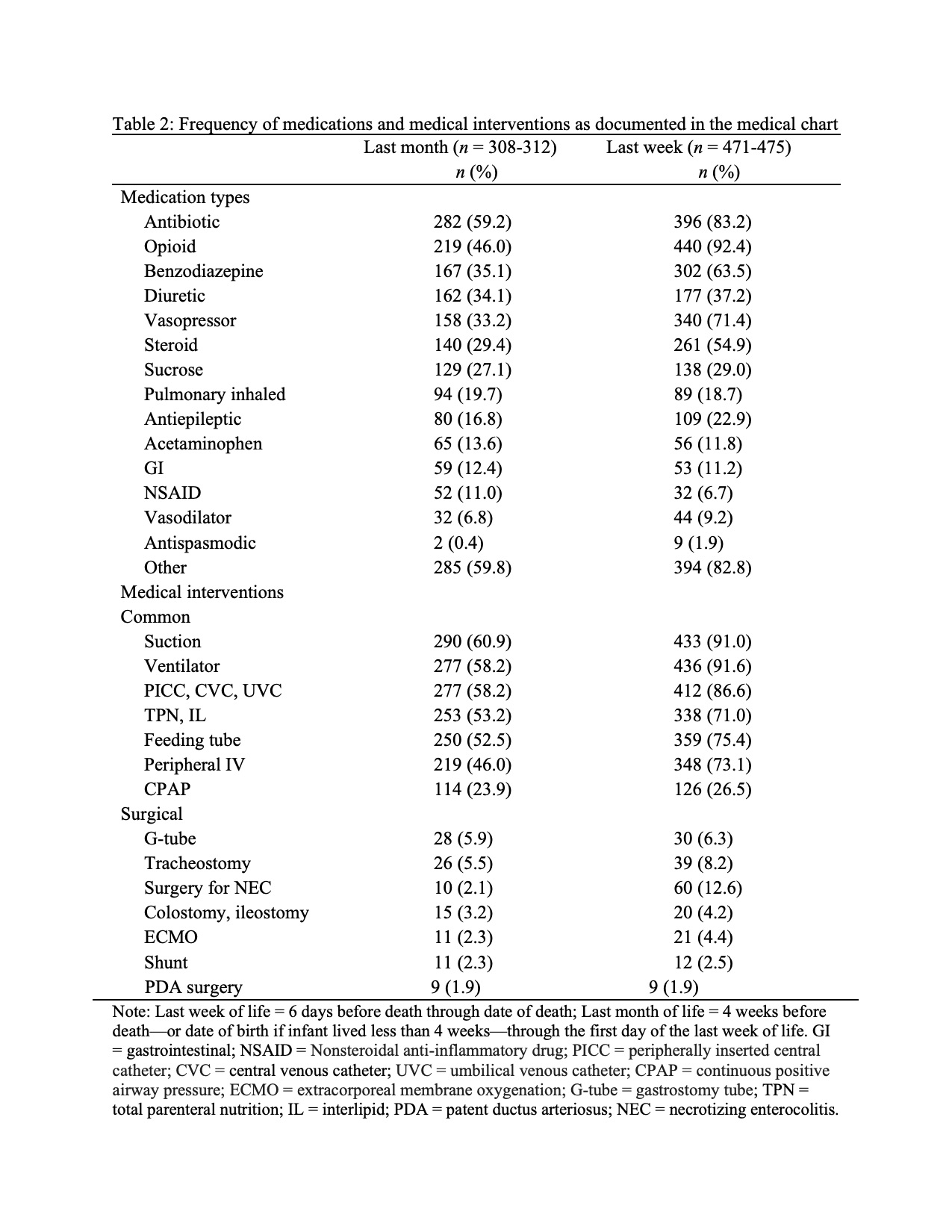
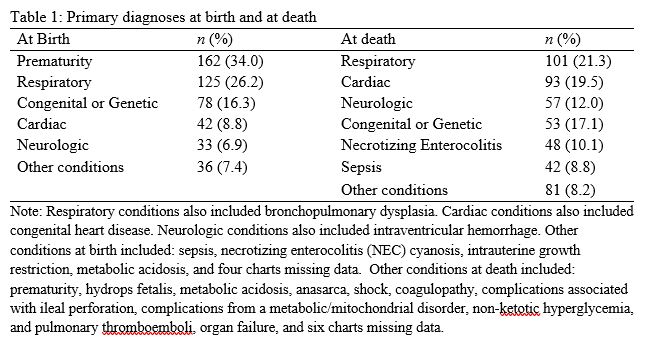
Results: Of the 476 infants who died in the NICU, about half (55.9%, n = 266) were male. The average gestational age at birth was 31.28 weeks (SD = 6.47), and most (68.5%, n = 326) survived for one week or more. Only 29% (n = 138) received a prenatal diagnosis, and the most common diagnosis at birth was prematurity. At death, infants were an average of 40.08 days old (SD = 84.46), and the most common cause was respiratory (Table 1). Paired samples t-tests indicated that infants received more medical interventions (t = -1.99, p = .048) and had more symptoms (t = -3.76, p < .001) documented during the last week of life compared to the last month. Antibiotics were the most common medication in the last month, while opioids were most common in the last week (Table 2). Suctioning was the most common medical intervention in both the last month and last week (Table 2). The most common symptom in the last month was respiratory difficulty, while unstable vital signs were most common in the last week (Table 3). Most infants (77.7%, n = 370) had life sustaining treatment discontinued, while 18.1% (n = 86) died following a code event. Only 34.9% of infants (n = 166) received palliative care consultation, placed 26.87 days before death (SD = 58.65) before death.Conclusion(s): Although the circumstances of infants who die in the NICU are complex, these findings are an important first step in understanding patterns of care and symptom trajectories of critically ill infants who die in the NICU. This information may help to reduce symptom burden and suffering and aid in supporting decision-making at EOL for critically-ill infants and their families.
Primary diagnoses at birth and at death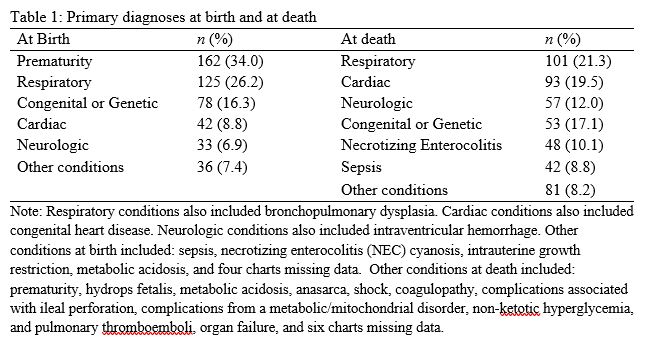
Frequency of medications and medical interventions as documented in the medical chart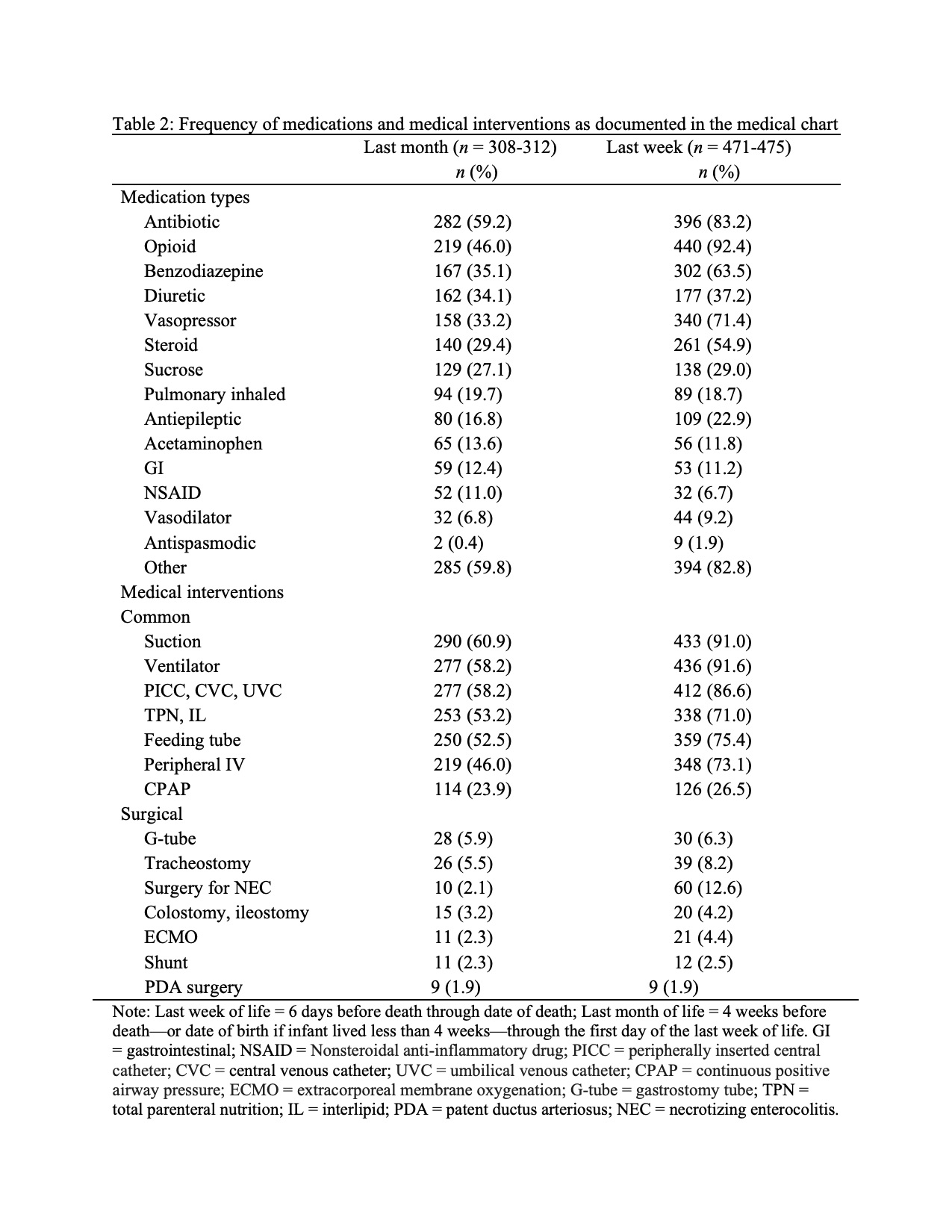
Objective: To characterize the demographic, clinical, and symptom characteristics of infants who died in the NICU.
Design/Methods: Retrospective electronic medical record (EMR) review of 476 infants who died in a large, Midwestern level IV NICU during admission to a NICU between July 1, 2009 and June 30, 2019. Demographic information, diagnosis, treatment, and EOL characteristics were extracted from each infant’s EMR by trained research assistants using a standardized form developed for the study.
Results: Of the 476 infants who died in the NICU, about half (55.9%, n = 266) were male. The average gestational age at birth was 31.28 weeks (SD = 6.47), and most (68.5%, n = 326) survived for one week or more. Only 29% (n = 138) received a prenatal diagnosis, and the most common diagnosis at birth was prematurity. At death, infants were an average of 40.08 days old (SD = 84.46), and the most common cause was respiratory (Table 1). Paired samples t-tests indicated that infants received more medical interventions (t = -1.99, p = .048) and had more symptoms (t = -3.76, p < .001) documented during the last week of life compared to the last month. Antibiotics were the most common medication in the last month, while opioids were most common in the last week (Table 2). Suctioning was the most common medical intervention in both the last month and last week (Table 2). The most common symptom in the last month was respiratory difficulty, while unstable vital signs were most common in the last week (Table 3). Most infants (77.7%, n = 370) had life sustaining treatment discontinued, while 18.1% (n = 86) died following a code event. Only 34.9% of infants (n = 166) received palliative care consultation, placed 26.87 days before death (SD = 58.65) before death.Conclusion(s): Although the circumstances of infants who die in the NICU are complex, these findings are an important first step in understanding patterns of care and symptom trajectories of critically ill infants who die in the NICU. This information may help to reduce symptom burden and suffering and aid in supporting decision-making at EOL for critically-ill infants and their families.
Primary diagnoses at birth and at death
Frequency of medications and medical interventions as documented in the medical chart