Emergency Medicine: Quality Improvement
Category: Abstract Submission
Emergency Medicine XIV
59 - Standardized medication reconciliation in a pediatric emergency department
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 59
Publication Number: 59.407
Publication Number: 59.407
Sarika K. Sheth, Rady Children's Hospital San Diego, San Diego, CA, United States; Mario Bialostozky, University of California, San Diego, San Diego, CA, United States; Kathryn Hollenbach, UCSD/Rady Children's Hospital, San Diego, CA, United States; Lindsay Heitzman, Rady Children's Hospital San Diego, San Diego, CA, United States; Deven O'Crump, Rady Children's Hospital San Diego, San Diego, CA, United States; Seema S. Mishra-Occhino, Rady Children's Hospital San Diego, San Diego, CA, United States; Gregory H. Langley, Rady Children's Hospital San Diego, San Diego, CA, United States; Kristen M. Santiago, Rady Children's Hospital San Diego, Poway, CA, United States; Fareed Saleh, UCSD/Rady Children's Hospital, SAN DIEGO, CA, United States; Glenn F. Billman, Rady Children's Hospital - San Diego, San Diego, CA, United States; Amy Bryl, Rady Children's Hospital San Diego, San Diego, CA, United States
- SS
Sarika K. Sheth, MD
Fellow Physician
Rady Children's Hospital San Diego
San Diego, California, United States
Presenting Author(s)
Background: Medication errors are common during transitions of care, such as discharge from the emergency department (ED) or urgent care (UC). The Joint Commission has identified medication reconciliation as a key safety practice.
Objective: Our aim was to increase the percentage of patients with completed medication reconciliation at discharge from our pediatric ED and four UCs from 25 to 75% in 12 months.
Design/Methods: A quality improvement (QI) task force including ED and UC physicians and nurses, informatics, and quality management was created. The baseline process for medication reconciliation was mapped and modified to create a streamlined process that enabled communication between existing nursing and physician workflows (Figure 1). An Ishikawa diagram was created to assess potential failures. Electronic health record (EHR) interventions included adapting the EHR workflow from an inpatient model and a best practice advisory alert. Educational interventions included on-shift nursing education, physician education through division meeting presentations, video tutorials, and just-in-time training, and periodic physician-specific and group feedback using funnel plots. Secondary process measures were the proportion of patients discharged from the ED and UCs with completed nurse home medication review. We used statistical process control to analyze changes in measures over time.
Results: In the UCs, nurse home medication review increased from 91% (UCL 96, LCL 86) to 98% (UCL 100, LCL 95) within 4 months of intervention and discharge medication reconciliation increased from 35% to 87% (Figure 2). In the ED, nurse home medication review increased from 2% to 84% (Figure 3) and discharge medication reconciliation increased from 25% (UCL 31, LCL 20) to 52% (UCL 57, LCL 47) within 5 months.Conclusion(s): Using QI methodology, we successfully increased the proportion of UC and ED discharged patients with completed medication reconciliation. This initiative is ongoing with the aim to reach goal in the ED and sustain improvement in the UCs.
Sarika Sheth CVJan 2022 Sarika Sheth CV.pdf
Figure 2.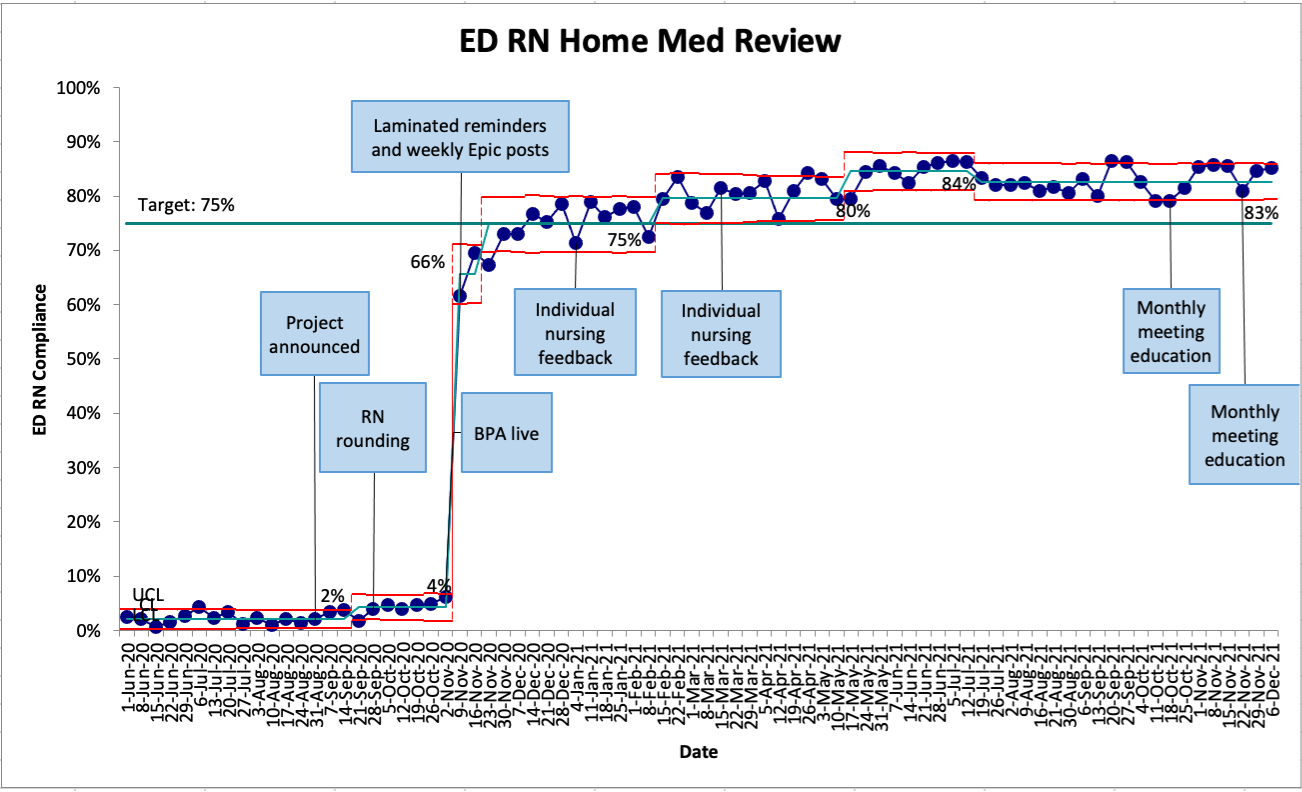 ED nursing home medication review
ED nursing home medication review
Objective: Our aim was to increase the percentage of patients with completed medication reconciliation at discharge from our pediatric ED and four UCs from 25 to 75% in 12 months.
Design/Methods: A quality improvement (QI) task force including ED and UC physicians and nurses, informatics, and quality management was created. The baseline process for medication reconciliation was mapped and modified to create a streamlined process that enabled communication between existing nursing and physician workflows (Figure 1). An Ishikawa diagram was created to assess potential failures. Electronic health record (EHR) interventions included adapting the EHR workflow from an inpatient model and a best practice advisory alert. Educational interventions included on-shift nursing education, physician education through division meeting presentations, video tutorials, and just-in-time training, and periodic physician-specific and group feedback using funnel plots. Secondary process measures were the proportion of patients discharged from the ED and UCs with completed nurse home medication review. We used statistical process control to analyze changes in measures over time.
Results: In the UCs, nurse home medication review increased from 91% (UCL 96, LCL 86) to 98% (UCL 100, LCL 95) within 4 months of intervention and discharge medication reconciliation increased from 35% to 87% (Figure 2). In the ED, nurse home medication review increased from 2% to 84% (Figure 3) and discharge medication reconciliation increased from 25% (UCL 31, LCL 20) to 52% (UCL 57, LCL 47) within 5 months.Conclusion(s): Using QI methodology, we successfully increased the proportion of UC and ED discharged patients with completed medication reconciliation. This initiative is ongoing with the aim to reach goal in the ED and sustain improvement in the UCs.
Sarika Sheth CVJan 2022 Sarika Sheth CV.pdf
Figure 2.
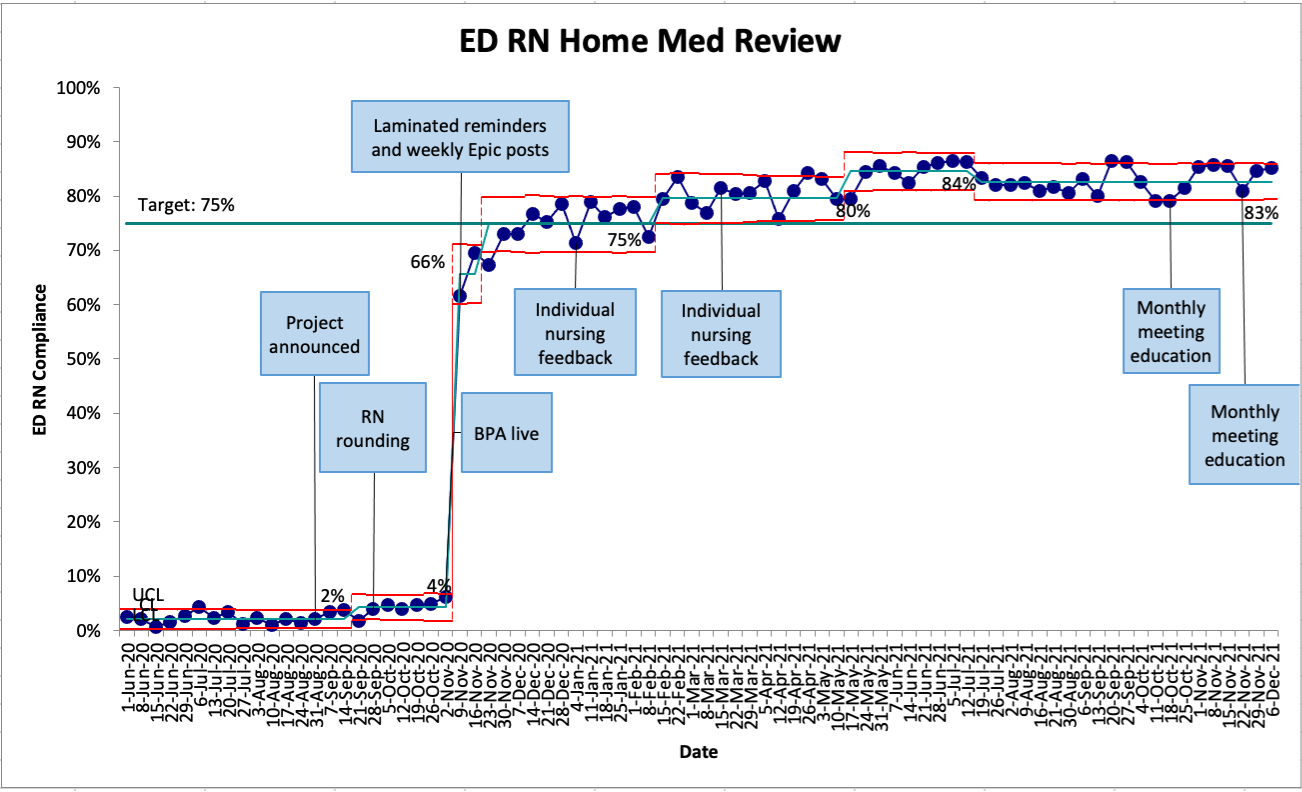 ED nursing home medication review
ED nursing home medication review