Neonatal General
Category: Abstract Submission
Neonatology General 11: Lung
368 - Survey of Nasal Continuous Positive Airway Pressure (nCPAP) Practices among Neonatal Providers in the United States
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 368
Publication Number: 368.440
Publication Number: 368.440
CIndy T. McEvoy, Oregon Health & Science University, Portland, OR, United States; Rachna Mamidi, Oregon Health & Science University School of Medicine, Portland, OR, United States; Mitzi Donabel A. Go, Oregon Health & Science University, Portland, OR, United States; Kelvin D. MacDonald, Oregon Health and Science University, Portland, OR, United States

Cindy T. McEvoy, MD, MCR (she/her/hers)
Professor of Pediatrics
Oregon Health & Science University
Portland, Oregon, United States
Presenting Author(s)
Background: Nasal continuous positive airway pressure (nCPAP) is the standard of care for the initial respiratory support of preterm infants.
Objective: To evaluate practice variation in the management of nCPAP among the Neonatal-Perinatal section of the AAP. We hypothesized large variations in clinical practice particularly with regards to CPAP discontinuation and chinstrap use.
Design/Methods: A web-based IRB approved survey was administered to the Neonatal-Perinatal section. It inquired about the NICU size, level, and location, approaches for CPAP initiation and management, and methods and post-menstrual ages (PMA) used to wean infants born at < 32 weeks gestation off CPAP. It assessed chinstrap use and rates of nipple feeding while on CPAP. Data were analyzed with descriptive statistics.
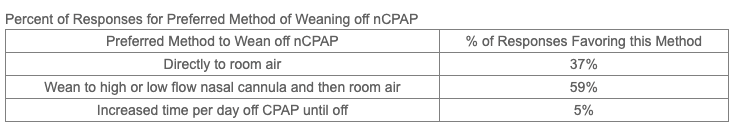
Results: Overall, 857/3700 (23%) of providers (718 neonatologists, 98 neonatal fellows) consented to the survey. 83% worked in a NICU with >20 beds and 94% in at least a level 3. 822/830 (99%) used CPAP with 300 (36%) primarily using bubble CPAP in infants < 32 weeks gestation; 229 (27%) using ventilator driven CPAP and 262 (31%) using a combination. For the primary interface used: 297/781 (38%) used short binasal prongs; 61 (8%) used long binasal prongs; 106 (14%) used a nasal mask; 295 (38%) used a combination. There was wide variation in: 1) the maximum CPAP used in the first 72 hours of life with 46/795 (6%) using 5 cmH2O; 258 (32%) using 6 cmH2O; 244 (31%) using 7 cm H2O; 216 (27%) using 8 cm H2O; 31 (4%) using ≥ 8 cm H2O; 2) the minimum CPAP usedprior to stopping or weaning CPAP were: 224/794 (28%) decreased to 4 cmH2O; 493 (62%) to 5 cmH2O and 44 (6%) to 6 cmH2O; 3) the methods to wean off CPAP (see Table). When asked when CPAP is discontinued or weaned, 69% responded when specific stability criteria were achieved; 22% at a specific PMA (5% at >30 weeks; 85% at >32 weeks; 11% at >34 weeks), and 8% answered other. While 65% endorsed that chinstraps improve CPAP efficacy; < 11% routinely used a chinstrap. When asked about barriers to chinstrap use, 27% said there were no barriers; 20% no sign of leak at the mouth; 15% reported adequate CPAP bubbling i; 10% did not have the equipment. 78% of responses never allowed infants to nipple on CPAP. 54% of providers worked in a NICU without CPAP initiation guidelines and 64% without CPAP discontinuation guidelines.Conclusion(s): There are significant practice variations across neonatology caregivers with regards to CPAP initiation, management, and discontinuation. Evidence-based research is needed in relation to respiratory outcomes to optimize CPAP strategies
Percent of Responses for Preferred Method of Weaning off Nasal CPAP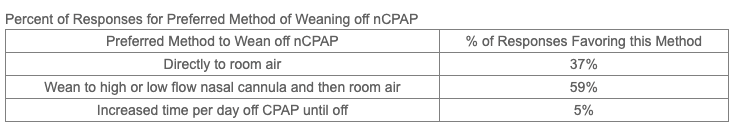
Objective: To evaluate practice variation in the management of nCPAP among the Neonatal-Perinatal section of the AAP. We hypothesized large variations in clinical practice particularly with regards to CPAP discontinuation and chinstrap use.
Design/Methods: A web-based IRB approved survey was administered to the Neonatal-Perinatal section. It inquired about the NICU size, level, and location, approaches for CPAP initiation and management, and methods and post-menstrual ages (PMA) used to wean infants born at < 32 weeks gestation off CPAP. It assessed chinstrap use and rates of nipple feeding while on CPAP. Data were analyzed with descriptive statistics.
Results: Overall, 857/3700 (23%) of providers (718 neonatologists, 98 neonatal fellows) consented to the survey. 83% worked in a NICU with >20 beds and 94% in at least a level 3. 822/830 (99%) used CPAP with 300 (36%) primarily using bubble CPAP in infants < 32 weeks gestation; 229 (27%) using ventilator driven CPAP and 262 (31%) using a combination. For the primary interface used: 297/781 (38%) used short binasal prongs; 61 (8%) used long binasal prongs; 106 (14%) used a nasal mask; 295 (38%) used a combination. There was wide variation in: 1) the maximum CPAP used in the first 72 hours of life with 46/795 (6%) using 5 cmH2O; 258 (32%) using 6 cmH2O; 244 (31%) using 7 cm H2O; 216 (27%) using 8 cm H2O; 31 (4%) using ≥ 8 cm H2O; 2) the minimum CPAP usedprior to stopping or weaning CPAP were: 224/794 (28%) decreased to 4 cmH2O; 493 (62%) to 5 cmH2O and 44 (6%) to 6 cmH2O; 3) the methods to wean off CPAP (see Table). When asked when CPAP is discontinued or weaned, 69% responded when specific stability criteria were achieved; 22% at a specific PMA (5% at >30 weeks; 85% at >32 weeks; 11% at >34 weeks), and 8% answered other. While 65% endorsed that chinstraps improve CPAP efficacy; < 11% routinely used a chinstrap. When asked about barriers to chinstrap use, 27% said there were no barriers; 20% no sign of leak at the mouth; 15% reported adequate CPAP bubbling i; 10% did not have the equipment. 78% of responses never allowed infants to nipple on CPAP. 54% of providers worked in a NICU without CPAP initiation guidelines and 64% without CPAP discontinuation guidelines.Conclusion(s): There are significant practice variations across neonatology caregivers with regards to CPAP initiation, management, and discontinuation. Evidence-based research is needed in relation to respiratory outcomes to optimize CPAP strategies
Percent of Responses for Preferred Method of Weaning off Nasal CPAP