Hospital Medicine: Hospital Medicine Quality Improvement
Category: Abstract Submission
Hospital Medicine: Clinical - Bronchiolitis/HFNC and Newborn Care
134 - Understanding High Flow Nasal Cannula Deimplementation in Pediatric Bronchiolitis
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 134
Publication Number: 134.415
Publication Number: 134.415
Diana Jo, Inova Children's Hospital, Falls Church, VA, United States; Courtney Port, Inova Children's Hospital, Falls Church, VA, United States; Anna Newcomb, Inova Fairfax Medical Campus, Falls Church, VA, United States; Amy Weis, Inova Children's Hospital, Chevy Chase, MD, United States; David Bastawrous, Inova Children's Hospital, Falls Church, VA, United States; Hayley R. Busch, Inova Children's Hospital, Falls Church, VA, United States; Nisha Gupta, Inova Children's Hospital, Falls Church, VA, United States
Diana Jo, MD
Resident
Inova Children's Hospital
Arlington, Virginia, United States
Presenting Author(s)
Background: High flow nasal cannula (HFNC) use in children with bronchiolitis does not significantly improve clinical outcomes, but can increase costs and intensive care unit utilization. Despite this, HFNC continues to be widely used. Therefore it is imperative to reduce HFNC use in children with bronchiolitis. Limited information is available on key factors that may support HFNC deimplementation.
Objective: Explore provider perceptions of the benefits of HFNC and acceptability of HFNC deimplementation and identify barriers and facilitators to HFNC deimplementation in children hospitalized with bronchiolitis.
Design/Methods: This was a mixed-methods study of providers at a large academic children’s hospital. Data were collected via electronic survey and semi-structured interviews of nurses (RNs), respiratory therapists (RTs), and physicians (MDs) from various hospital settings. Quantitative data were analyzed using Chi-square and exact testing where appropriate. Qualitative data were analyzed using thematic content analysis.
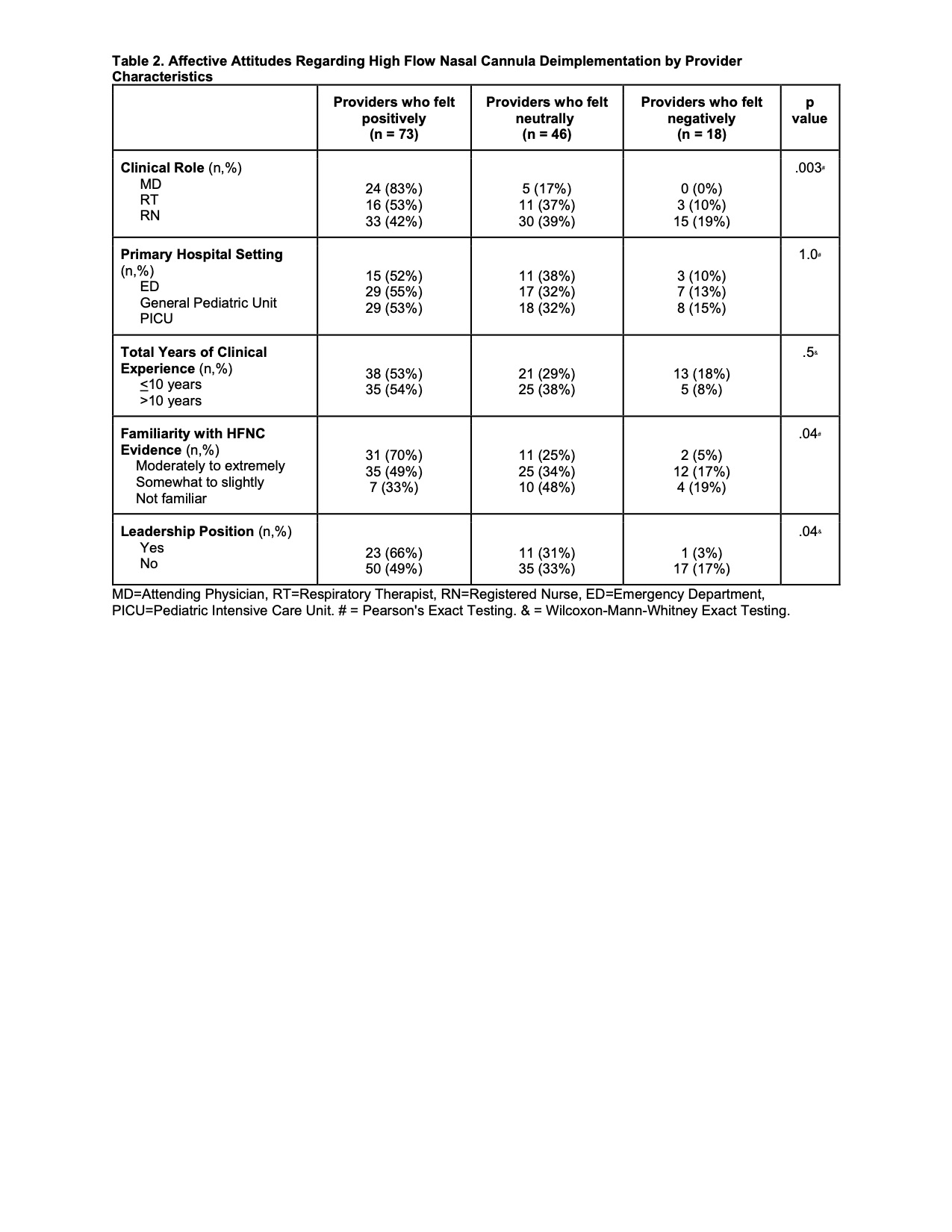
Results: 137 (41%) providers completed the survey; 9 participated in interviews. HFNC-related benefits to clinical outcomes (length of stay, length of oxygen supplementation, and ICU transfer) were identified by 94 (69%) providers, despite current evidence not supporting these outcomes (Table 1). Overall, 73 (53%) providers reported positive affective attitudes in regards to HFNC deimplementation, 46 (34%) responded neutrally, and 18 (13%) reported negative affective attitudes. Positive affective attitudes increased as perceived familiarity with HFNC evidence increased (p=.01). Primary hospital setting and years of clinical experience were not associated with affective attitudes (p=1 and 0.5, respectively). MDs were more likely than RNs and RTs to report positive affective attitudes (Table 2). Barriers to deimplementation identified during interviews included provider discomfort with not intervening, provider perception that HFNC helps, and a lack of inter-rater reliability with patient assessments. Facilitators to deimplementation included adopting a culture of safely doing less, accessible education for staff, and enhanced interdisciplinary communication (Table 3).Conclusion(s): Deimplementation of HFNC in children with bronchiolitis is acceptable amongst healthcare providers. Future HFNC deimplementation efforts should focus on adopting a culture of safely doing less, providing staff education, and enhancing interdisciplinary communication.
CVEdit12.14.2021.pdf
Table 2. Affective Attitudes Regarding High Flow Nasal Cannula Deimplementation by Provider Characteristics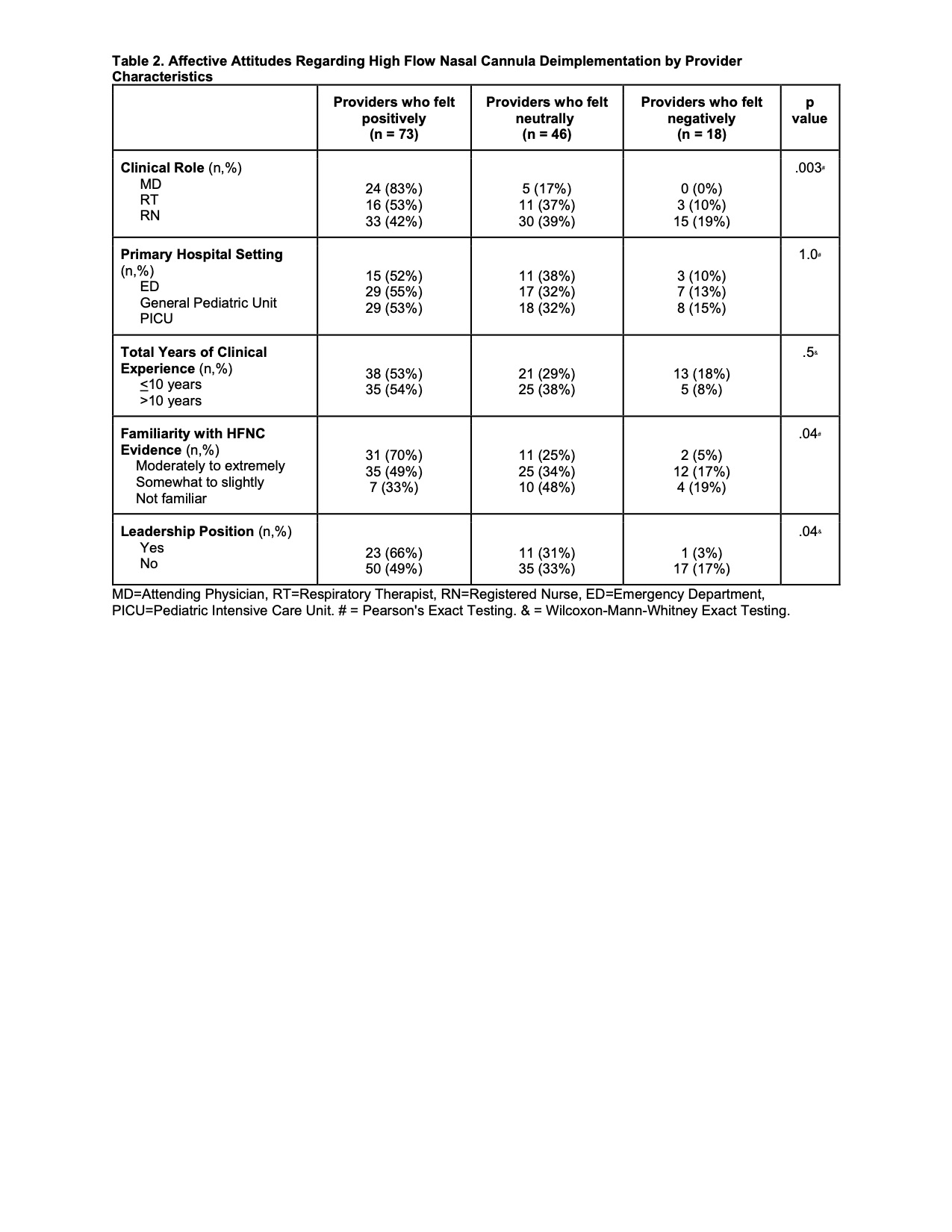
Objective: Explore provider perceptions of the benefits of HFNC and acceptability of HFNC deimplementation and identify barriers and facilitators to HFNC deimplementation in children hospitalized with bronchiolitis.
Design/Methods: This was a mixed-methods study of providers at a large academic children’s hospital. Data were collected via electronic survey and semi-structured interviews of nurses (RNs), respiratory therapists (RTs), and physicians (MDs) from various hospital settings. Quantitative data were analyzed using Chi-square and exact testing where appropriate. Qualitative data were analyzed using thematic content analysis.
Results: 137 (41%) providers completed the survey; 9 participated in interviews. HFNC-related benefits to clinical outcomes (length of stay, length of oxygen supplementation, and ICU transfer) were identified by 94 (69%) providers, despite current evidence not supporting these outcomes (Table 1). Overall, 73 (53%) providers reported positive affective attitudes in regards to HFNC deimplementation, 46 (34%) responded neutrally, and 18 (13%) reported negative affective attitudes. Positive affective attitudes increased as perceived familiarity with HFNC evidence increased (p=.01). Primary hospital setting and years of clinical experience were not associated with affective attitudes (p=1 and 0.5, respectively). MDs were more likely than RNs and RTs to report positive affective attitudes (Table 2). Barriers to deimplementation identified during interviews included provider discomfort with not intervening, provider perception that HFNC helps, and a lack of inter-rater reliability with patient assessments. Facilitators to deimplementation included adopting a culture of safely doing less, accessible education for staff, and enhanced interdisciplinary communication (Table 3).Conclusion(s): Deimplementation of HFNC in children with bronchiolitis is acceptable amongst healthcare providers. Future HFNC deimplementation efforts should focus on adopting a culture of safely doing less, providing staff education, and enhancing interdisciplinary communication.
CVEdit12.14.2021.pdf
Table 2. Affective Attitudes Regarding High Flow Nasal Cannula Deimplementation by Provider Characteristics