Health Services Research
Category: Abstract Submission
Health Services Research III
11 - Predictive Modeling of Prospective High Healthcare Use: Comparison of Models Using Social Risk Factors vs. Prior Utilization and Co-morbidities
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 11
Publication Number: 11.414
Publication Number: 11.414
Megan T. Sandel, Boston University School of Medicine, Boston, MA, United States; Ana Poblacion, Boston Medical Center, Boston, MA, United States; Stephanie Ettinger de Cuba, Boston University School of Medicine, Boston, MA, United States; Richard Sheward, Children's HealthWatch at Boston Medical Center, Boston, MA, United States; Lindsey Rateau, Boston University School of Public Health, BOSTON, MA, United States; Margaret G. Shea, Boston University School of Public Health, Cambridge, MA, United States; Timothy Heeren, Boston University School of Public Health, Boston, MA, United States; Amresh Hanchate, Wake Forest School of Medicine, Winston-Salem, NC, United States

Megan Sandel, MD MPH (she/her/hers)
Associate Professor
Boston University School of Medicine
Boston Medical Center
Boston, Massachusetts, United States
Presenting Author(s)
Background: Value-based models in healthcare heavily focus on identifying & treating high need, high cost adults to drive down high utilization & healthcare costs. Children can be forgotten unless they are high utilizers (i.e., medically complex). Prior utilization & co-morbidities can predict future utilization for children, but whether social risk factor data may be used to predict future high utilization among young children is less known.
Objective: Develop predictive models for High Utilization (HU), defined as Acute Utilization (AU) & Low Acuity Emergency Department (LAED) use in children, by comparing modifiable hardships (Social Risk Factors-SRFs) & non-modifiable (prior utilization & co-morbidities) risks.
Design/Methods: Longitudinal data (2007-2019) from families with children < 4 years interviewed in emergency departments (EDs) or clinics in 3 US cities included sociodemographic characteristics and material hardships (food, housing or energy insecurity or healthcare cost trade-offs). Survey data linked to electronic health records were used to obtain prior (year 1 post survey) & prospective (year 2 post survey) ED, outpatient & inpatient visits, & baseline co-morbidities by ICD-10 codes. Outcome variable AU was defined as 3+ ED visits &/or 1+ inpatient stay, & LAED was defined using a Medicaid Accountable Care Organization diagnoses list and 2+ LAED visits in year 2. Two models were conceptualized: “Conventional Model” using prior utilization & co-morbidities & “Survey Model” using SRFs only. C-statistic was used to measure predictive accuracy (discrimination) of each model.
Results: Of 11,871 children, 34% identified as Hispanic (H), 43% Black-non H, 18% White-non H, 4% other. In the sample, 84 % were publicly insured, 9% privately insured, and 6% uninsured, and 16 % of children had AU while 14% of children had LAED use. Children in households experiencing 1+ material hardship accounted for 64% with AU & 65% with LAED use. Both models were able to predict future HU, however C-statistic was higher for the Conventional Model.Conclusion(s): Despite lower C-statistic, Survey Models performed well compared with Conventional Models in a predominantly publicly insured, diverse sample. Since prior utilization & co-morbidities are unmodifiable risks, health systems could consider using modifiable social risks to predict & lower AU & LAED use among children. Future research should examine if other social risks, such as parental Experiences of Discrimination or Adverse Childhood Experiences or Health Outcomes from Positive Experiences strengthen predictive accuracy.
C Statistics for Conventional vs Survey only models for Acute Utilization (AU) and Low Acuity ED visits (LAED)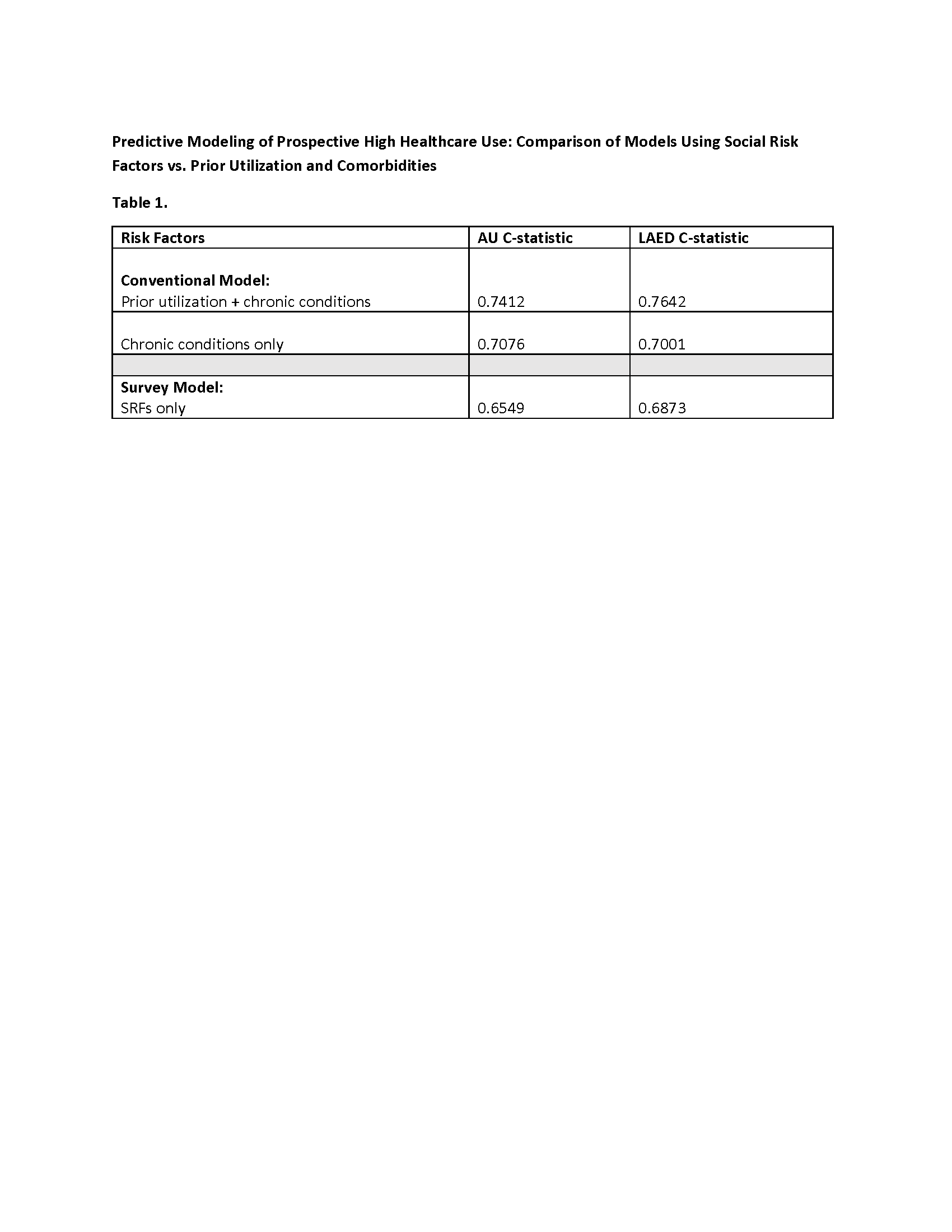 AU- Acute Utilization (as defined by 3+ ED visits and/or 1+ inpatient stays per year)
AU- Acute Utilization (as defined by 3+ ED visits and/or 1+ inpatient stays per year)
LAED- Low Acuity ED visits (as defined by 2+ ED visits/year meeting a Medicaid Accountable Care Definition of diagnoses of low acuity)
Objective: Develop predictive models for High Utilization (HU), defined as Acute Utilization (AU) & Low Acuity Emergency Department (LAED) use in children, by comparing modifiable hardships (Social Risk Factors-SRFs) & non-modifiable (prior utilization & co-morbidities) risks.
Design/Methods: Longitudinal data (2007-2019) from families with children < 4 years interviewed in emergency departments (EDs) or clinics in 3 US cities included sociodemographic characteristics and material hardships (food, housing or energy insecurity or healthcare cost trade-offs). Survey data linked to electronic health records were used to obtain prior (year 1 post survey) & prospective (year 2 post survey) ED, outpatient & inpatient visits, & baseline co-morbidities by ICD-10 codes. Outcome variable AU was defined as 3+ ED visits &/or 1+ inpatient stay, & LAED was defined using a Medicaid Accountable Care Organization diagnoses list and 2+ LAED visits in year 2. Two models were conceptualized: “Conventional Model” using prior utilization & co-morbidities & “Survey Model” using SRFs only. C-statistic was used to measure predictive accuracy (discrimination) of each model.
Results: Of 11,871 children, 34% identified as Hispanic (H), 43% Black-non H, 18% White-non H, 4% other. In the sample, 84 % were publicly insured, 9% privately insured, and 6% uninsured, and 16 % of children had AU while 14% of children had LAED use. Children in households experiencing 1+ material hardship accounted for 64% with AU & 65% with LAED use. Both models were able to predict future HU, however C-statistic was higher for the Conventional Model.Conclusion(s): Despite lower C-statistic, Survey Models performed well compared with Conventional Models in a predominantly publicly insured, diverse sample. Since prior utilization & co-morbidities are unmodifiable risks, health systems could consider using modifiable social risks to predict & lower AU & LAED use among children. Future research should examine if other social risks, such as parental Experiences of Discrimination or Adverse Childhood Experiences or Health Outcomes from Positive Experiences strengthen predictive accuracy.
C Statistics for Conventional vs Survey only models for Acute Utilization (AU) and Low Acuity ED visits (LAED)
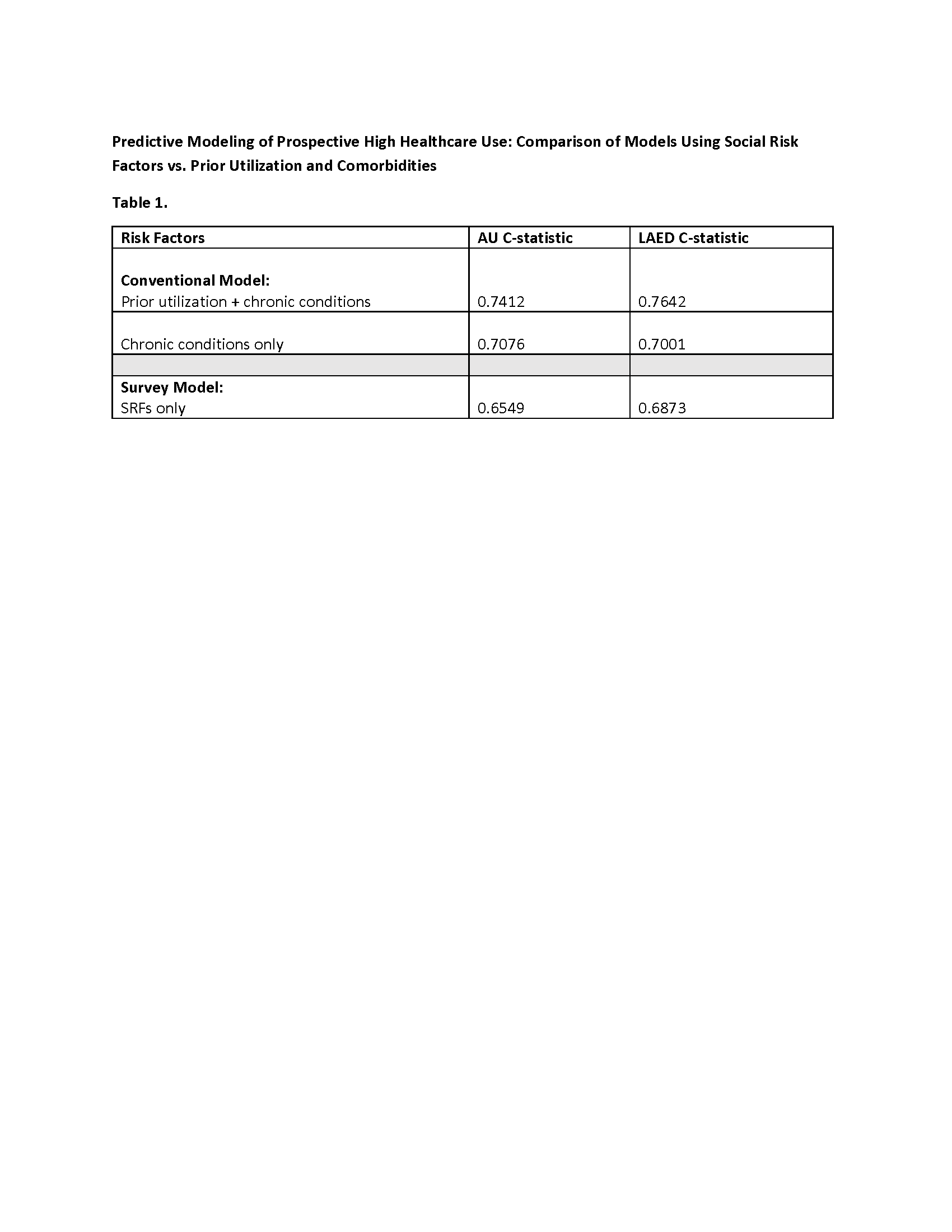 AU- Acute Utilization (as defined by 3+ ED visits and/or 1+ inpatient stays per year)
AU- Acute Utilization (as defined by 3+ ED visits and/or 1+ inpatient stays per year)LAED- Low Acuity ED visits (as defined by 2+ ED visits/year meeting a Medicaid Accountable Care Definition of diagnoses of low acuity)
