Neonatal Pulmonology
Category: Abstract Submission
Neonatal Pulmonology V: Preclinical studies and Clinical Care Issues
478 - Prone positioning of neonates with different types of lung injury: effect on respiratory function and hemodynamics
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 478
Publication Number: 478.433
Publication Number: 478.433
Barbara Loi, APHP, Paris, Ile-de-France, France; Giulia regiroli, Assistance publique hôpitaux de paris, Clamart, Ile-de-France, France; Roberta Centorrino, APHP, Paris, Ile-de-France, France; Daniele M. De Luca, Paris Saclay University - "A.Beclere" Hospital, Clamart (Paris), Ile-de-France, France

Barbara Loi, MD (she/her/hers)
Fellow
Paris Saclay University
Paris, Ile-de-France, France
Presenting Author(s)
Background: Prone positioning is known to improve oxygenation in adults with respiratory failure due to restrictive pattern (i.e.: severe ARDS).
Objective: We aim to investigate the physiological respiratory and hemodynamic effects of prone positioning in neonates with different types of lung injury. We hypothesize that prone positioning may improve respiratory function.
Design/Methods: This is a prospective, quasi-randomized, observational, crossover, physiologic cohort study. Over a 12h-period, infants were allocated to switch between two different body positions (supine and prone) every 6 h. We analyzed data of two timepoints (T0 and T6h for every position) from patients who switched to prone position when initially supine (SP period) and from patients who switched to supine position when initially prone (PS period). We enrolled cases of respiratory failure due to: 1) severe restrictive pattern (neonates fulfilling Montreux definition of neonatal ARDS (NARDS), n=55)1, 2) mild restrictive pattern (preterm neonates recovering from RDS after surfactant replacement, n=56), 3) mixed pattern (neonates with evolving BPD, that is chronic pulmonary insufficiency of prematurity (CPIP), n=50).2 The following were measured for each timepoint: lung aeration (by semiquantitative lung ultrasound score (LUS)3), pre-ductal SpO2, transcutaneous PtcO2/PtcCO2 (also used to calculate derived oxygenation indexes), cardiac output (by electrical cardiometry4), mean arterial pressure (MAP), heart rate and perfusion index. Data were analyzed with multivariate RM-ANOVA considering as covariates the type of lung injury and the initial patients’ position.
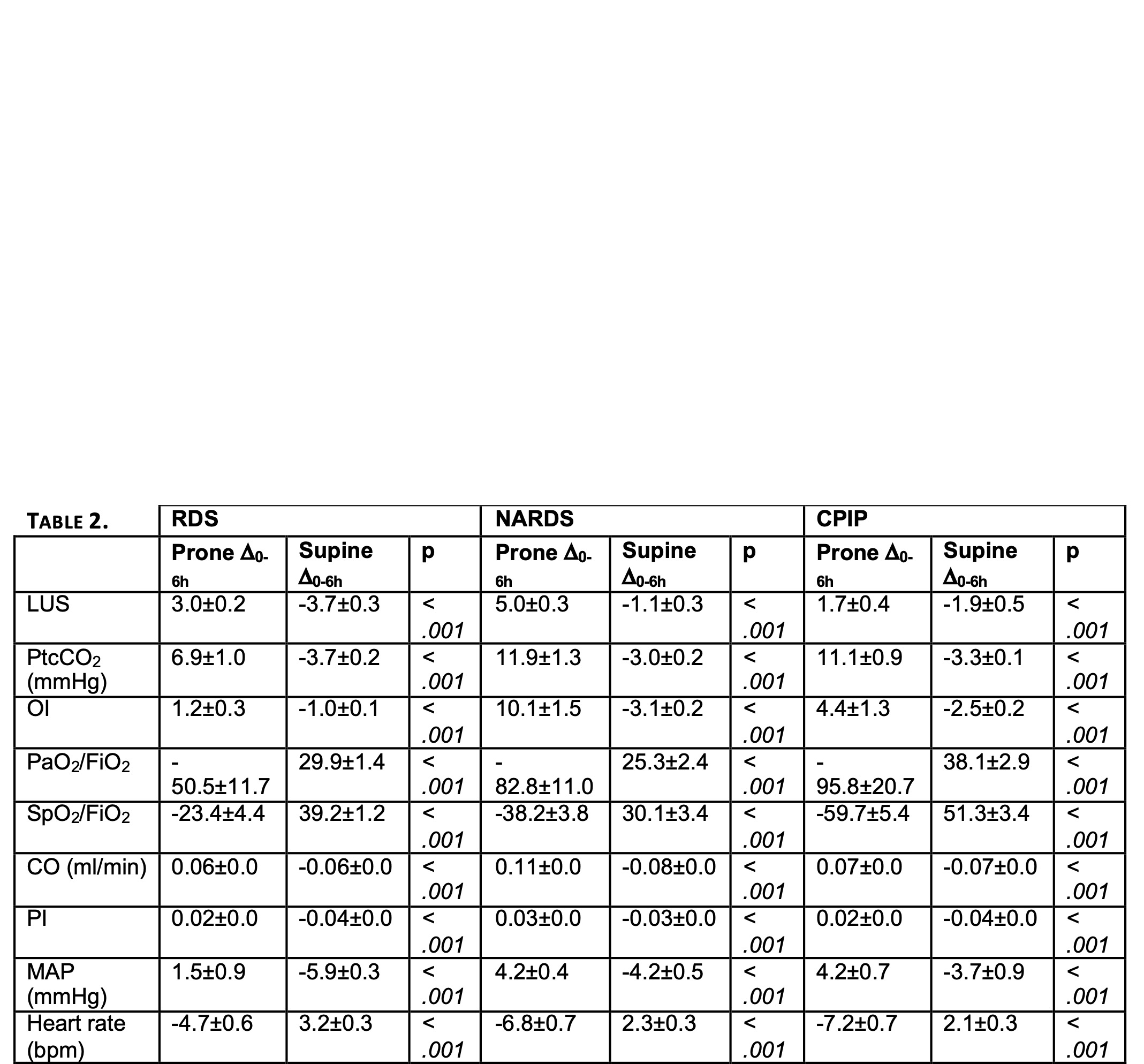
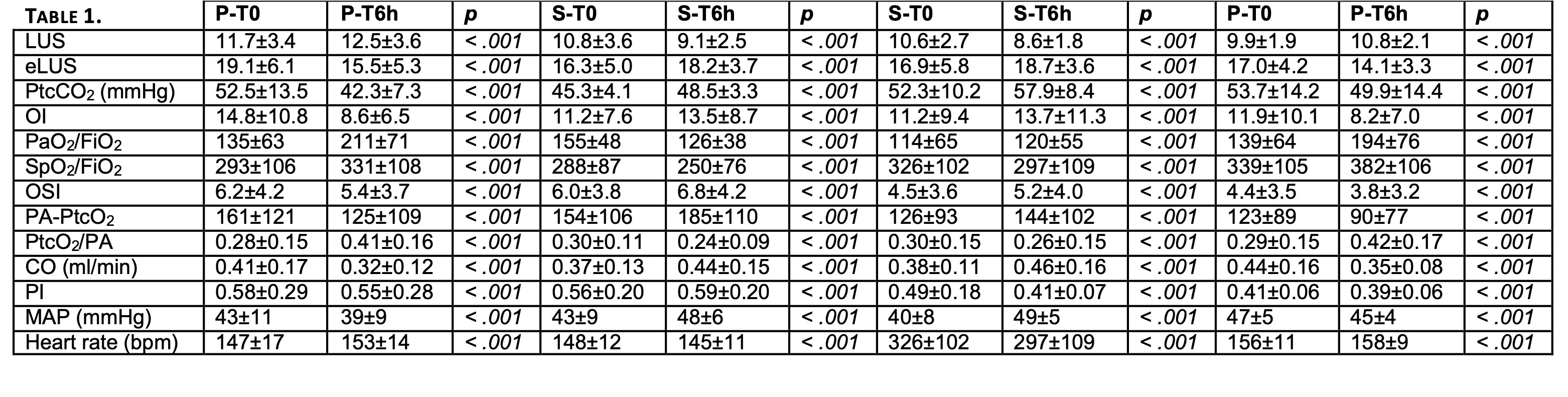
Results: In the whole population, lung aeration and gas exchange measurements significantly improved with pronation (Tab.1). Cardiac output, perfusion index, MAP and HR changes with pronation although remaining within physiological values (Tab.1). Changes () in lung aeration (p < 0.001), OI (p < 0.001), PtcO2/FiO2 (p < 0.001) SpO2/FiO2 (p < 0.001) as well as PI (p < 0.001), HR (p < 0.001) and MAP (p < 0.001) are more pronounced in NARDS neonates (Tab.2).Conclusion(s): Prone positioning significantly improves lung aeration and gas exchange. These effects are more evident in neonates with severe restrictive pattern (NARDS) but are also occurring in neonates with RDS or CPIP. Prone positioning alters hemodynamic parameters which however remain within normal values.
References
1. De Luca D. Lancet Respir Med 2017
2. Steinhorn R. J Pediatr 2018
3. Brat R. JAMA Pediatr 2015
4. Boet A. J Perinatol 2016
Respiratory and hemodynamic effects of prone positioning in the whole population (irrespective of the underlying lung disorder).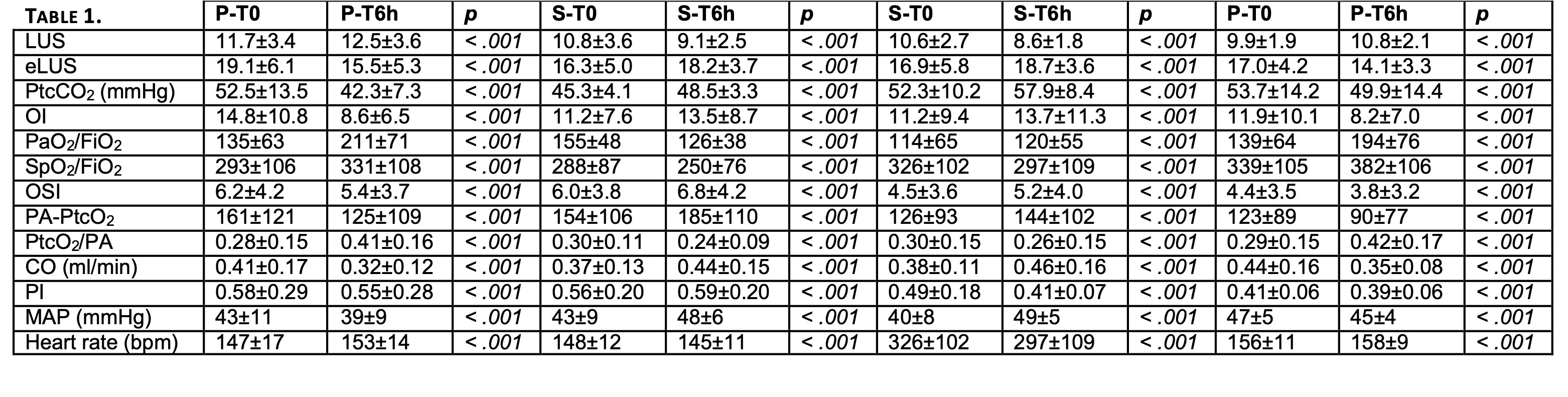
Respiratory and hemodynamic effects of prone positioning in neonates with different type of lung disorder.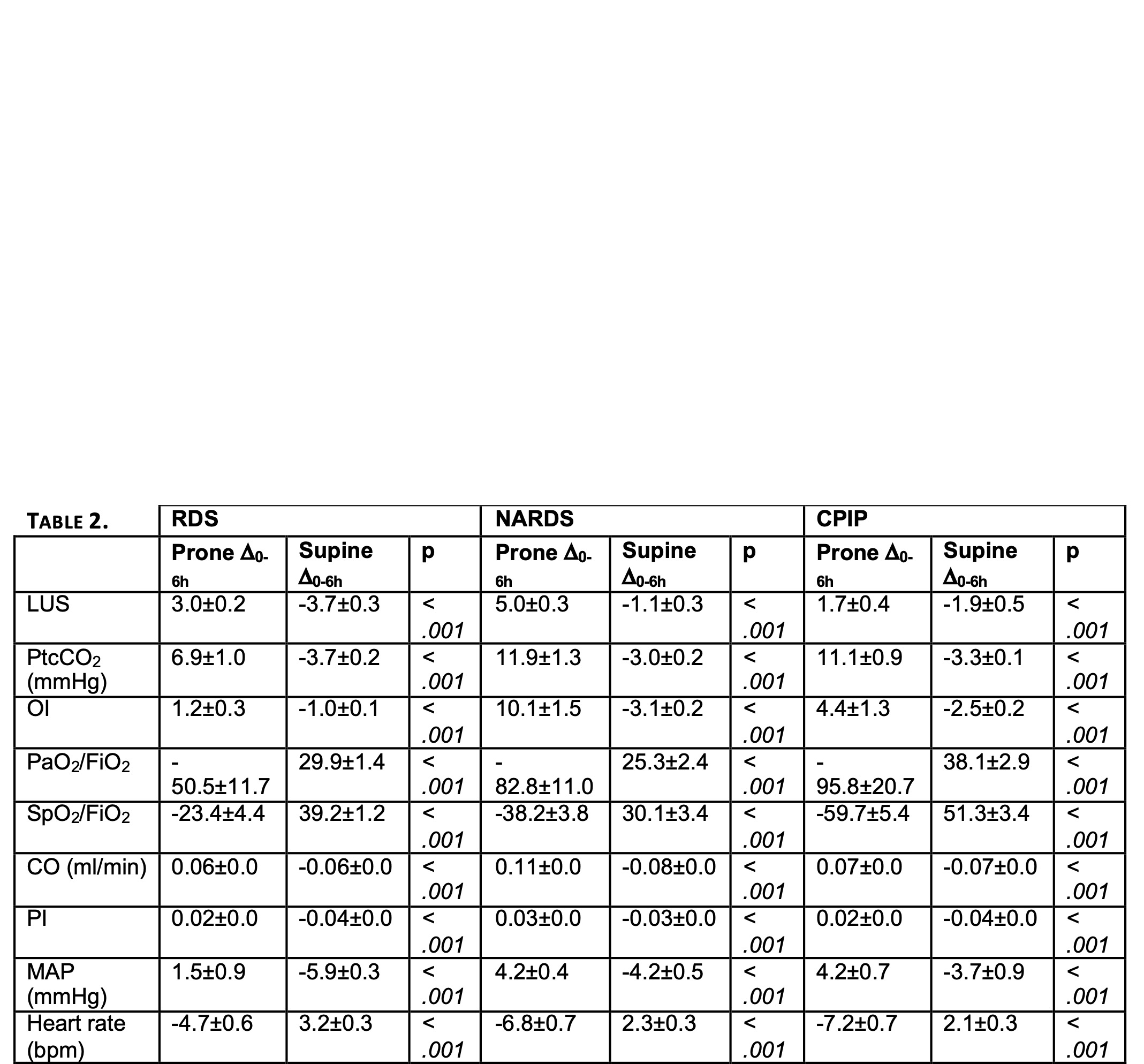
Objective: We aim to investigate the physiological respiratory and hemodynamic effects of prone positioning in neonates with different types of lung injury. We hypothesize that prone positioning may improve respiratory function.
Design/Methods: This is a prospective, quasi-randomized, observational, crossover, physiologic cohort study. Over a 12h-period, infants were allocated to switch between two different body positions (supine and prone) every 6 h. We analyzed data of two timepoints (T0 and T6h for every position) from patients who switched to prone position when initially supine (SP period) and from patients who switched to supine position when initially prone (PS period). We enrolled cases of respiratory failure due to: 1) severe restrictive pattern (neonates fulfilling Montreux definition of neonatal ARDS (NARDS), n=55)1, 2) mild restrictive pattern (preterm neonates recovering from RDS after surfactant replacement, n=56), 3) mixed pattern (neonates with evolving BPD, that is chronic pulmonary insufficiency of prematurity (CPIP), n=50).2 The following were measured for each timepoint: lung aeration (by semiquantitative lung ultrasound score (LUS)3), pre-ductal SpO2, transcutaneous PtcO2/PtcCO2 (also used to calculate derived oxygenation indexes), cardiac output (by electrical cardiometry4), mean arterial pressure (MAP), heart rate and perfusion index. Data were analyzed with multivariate RM-ANOVA considering as covariates the type of lung injury and the initial patients’ position.
Results: In the whole population, lung aeration and gas exchange measurements significantly improved with pronation (Tab.1). Cardiac output, perfusion index, MAP and HR changes with pronation although remaining within physiological values (Tab.1). Changes () in lung aeration (p < 0.001), OI (p < 0.001), PtcO2/FiO2 (p < 0.001) SpO2/FiO2 (p < 0.001) as well as PI (p < 0.001), HR (p < 0.001) and MAP (p < 0.001) are more pronounced in NARDS neonates (Tab.2).Conclusion(s): Prone positioning significantly improves lung aeration and gas exchange. These effects are more evident in neonates with severe restrictive pattern (NARDS) but are also occurring in neonates with RDS or CPIP. Prone positioning alters hemodynamic parameters which however remain within normal values.
References
1. De Luca D. Lancet Respir Med 2017
2. Steinhorn R. J Pediatr 2018
3. Brat R. JAMA Pediatr 2015
4. Boet A. J Perinatol 2016
Respiratory and hemodynamic effects of prone positioning in the whole population (irrespective of the underlying lung disorder).
Respiratory and hemodynamic effects of prone positioning in neonates with different type of lung disorder.