Back
Medical Education: Resident
Category: Abstract Submission
Medical Education 15 - Medical Education: Resident VI
295 - Resident Perceptions of Respiratory Therapy Directed Asthma Pathway Weaning and the Impact on Education: A Mixed-Methods Study
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 295
Publication Number: 295.421
Publication Number: 295.421
Nathaniel Goodrich, University of Nebraska Medical Center, Omaha, NE, United States; Simone Warrack, Bellin Health, Green Bay, WI, United States; Lauren Maskin, Children's Hospital & Medical Center, Omaha, NE, United States; Kristy J. Carlson, University of Nebraska College of Medicine, Omaha, NE, United States; Allison Ashford, University of Nebraska College of Medicine, Omaha, NE, United States

Nathaniel Goodrich, MD
Associate Professor
University of Nebraska College of Medicine
Omaha, Nebraska, United States
Presenting Author(s)
Background: Hospitals have commonly utilized asthma exacerbation pathways in the inpatient setting. At our hospital, such a pathway has been in place for several years. However, in October 2019, a protocol was implemented allowing respiratory therapists (RT) to wean albuterol dosing based on clinical respiratory scores (CRS). Though several studies have been published on RT-led weaning of albuterol treatments in cases of asthma exacerbations, none have focused on the impacts on education.
Objective: The purpose of our study was to examine the impact of an RT-led weaning protocol on resident education and perceptions.
Design/Methods: Residents in pediatrics and medicine-pediatrics were invited via email to respond to survey items using a 5-point Likert scale (1=strongly disagree, 5=strongly agree). Participants were asked about their comfort level in treating asthmatic patients and beliefs regarding the RT-led weaning protocol. The survey also included five objective clinical questions designed to assess resident knowledge of the pathway and care of asthmatics. Survey responses were anonymous. Two follow-up focus groups were conducted to allow for open dialogue and follow up questions on the RT led weaning protocol. Focus groups interviews were conducted via Zoom by a third party who provided a de-identified summary of the interviews. Informed consent was obtained for all participants.
Results: A total of 35 residents (57% response rate) completed the survey (Table 1). A majority (74%) of residents agreed that clinical pathways support resident education, and 63% felt they supported autonomy. Respectively, only 20% and 24% of residents agreed or strongly agreed that RT-led weaning positively affected their preparedness for managing asthma autonomously or their education on asthma management. Despite the potential impact of RT-led weaning, most (80%) residents felt comfortable assessing and weaning asthmatics. Furthermore, most residents could determine when to wean (96%) or escalate (75%) treatment on clinical scenario questions. Notably, 11% of residents (n=7) participated in the focus groups with five major themes emerging, including resident comfort managing asthmatics and help that RT’s can provide to residents (Table 2).Conclusion(s): Most residents felt comfortable caring for asthmatics and agreed that pathways support resident education. Residents indicated that hands-on learning was a large component of their education. Opinions on the effect of RT-led weaning on their education was mixed. Due to timeline constraints, residents were only assessed after the RT-led protocol had been introduced.
Resident Asthma Weaning Survey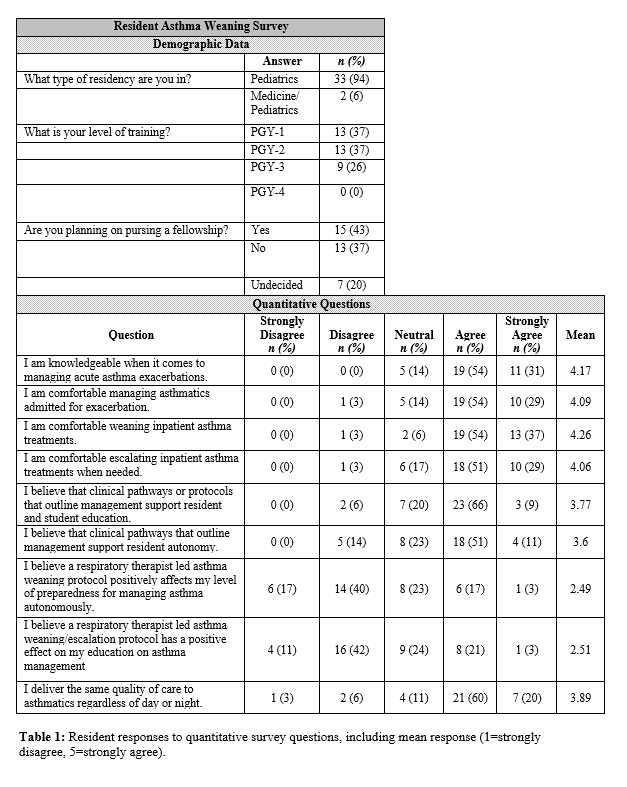 Table 1: Resident responses to quantitative survey questions, including mean response (1=strongly disagree, 5=strongly agree).
Table 1: Resident responses to quantitative survey questions, including mean response (1=strongly disagree, 5=strongly agree).
Representative Comments from Focus Group Participants.png) Table 2: Representative comments from residents participating in focus groups, including five major themes identified.
Table 2: Representative comments from residents participating in focus groups, including five major themes identified.
Objective: The purpose of our study was to examine the impact of an RT-led weaning protocol on resident education and perceptions.
Design/Methods: Residents in pediatrics and medicine-pediatrics were invited via email to respond to survey items using a 5-point Likert scale (1=strongly disagree, 5=strongly agree). Participants were asked about their comfort level in treating asthmatic patients and beliefs regarding the RT-led weaning protocol. The survey also included five objective clinical questions designed to assess resident knowledge of the pathway and care of asthmatics. Survey responses were anonymous. Two follow-up focus groups were conducted to allow for open dialogue and follow up questions on the RT led weaning protocol. Focus groups interviews were conducted via Zoom by a third party who provided a de-identified summary of the interviews. Informed consent was obtained for all participants.
Results: A total of 35 residents (57% response rate) completed the survey (Table 1). A majority (74%) of residents agreed that clinical pathways support resident education, and 63% felt they supported autonomy. Respectively, only 20% and 24% of residents agreed or strongly agreed that RT-led weaning positively affected their preparedness for managing asthma autonomously or their education on asthma management. Despite the potential impact of RT-led weaning, most (80%) residents felt comfortable assessing and weaning asthmatics. Furthermore, most residents could determine when to wean (96%) or escalate (75%) treatment on clinical scenario questions. Notably, 11% of residents (n=7) participated in the focus groups with five major themes emerging, including resident comfort managing asthmatics and help that RT’s can provide to residents (Table 2).Conclusion(s): Most residents felt comfortable caring for asthmatics and agreed that pathways support resident education. Residents indicated that hands-on learning was a large component of their education. Opinions on the effect of RT-led weaning on their education was mixed. Due to timeline constraints, residents were only assessed after the RT-led protocol had been introduced.
Resident Asthma Weaning Survey
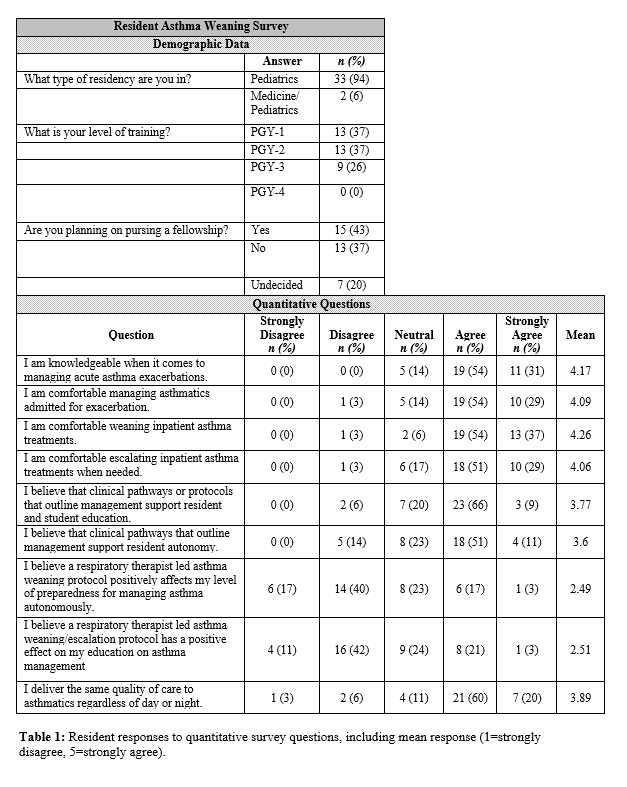 Table 1: Resident responses to quantitative survey questions, including mean response (1=strongly disagree, 5=strongly agree).
Table 1: Resident responses to quantitative survey questions, including mean response (1=strongly disagree, 5=strongly agree).Representative Comments from Focus Group Participants
.png) Table 2: Representative comments from residents participating in focus groups, including five major themes identified.
Table 2: Representative comments from residents participating in focus groups, including five major themes identified.