Back
Neonatal Neurology: Clinical
Category: Abstract Submission
Neurology 7: Neonatal Neurology Term Imaging
354 - Routine Implementation of Magnetic Resonance Venography in Neonates with Encephalopathy Receiving Therapeutic Hypothermia and Its Value in the Diagnosis of Cerebral Venous Sinus Thrombosis
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 354
Publication Number: 354.443
Publication Number: 354.443
Chelsea Munster, Brigham and Women's Hospital, Boston, MA, United States; Hoda Elshibiny, Birgham and Women's Hospital, Boston, MA, United States; Eniko Szakmar, Harvard Medical School, Brigham and Women's Hospital, Budapest, Budapest, Hungary; Edward Yang, Boston Children's Hospital, Jamaica Plain, MA, United States; Terrie E. Inder, Harvard Medical School, Boston, MA, United States; Mohamed El-Dib, Harvard Medical School, Boston, MA, United States

Chelsea Munster, BA (she/her/hers)
Clinical Research Assistant
Brigham and Women's Hospital
731 South Eureka St, California, United States
Presenting Author(s)
Background: Neonatal encephalopathy (NE) may be associated with increased incidence of cerebral venous sinus thrombosis (CVST), a diagnosis with significant therapeutic implications. A recent study by Radicioni et al. demonstrated that 10 out of 37 asphyxiated neonates (27%) undergoing therapeutic hypothermia (TH) were diagnosed with CVST using magnetic resonance venography (MRV) [1]. For this reason, MRV was routinely added to the imaging protocol for NE infants in a tertiary care center providing TH for infants with mild, moderate and severe encephalopathy.
Objective: To investigate the frequency and incidence of CVST diagnoses before and after implementation of routine MRV into the post-rewarming magnetic resonance imaging (MRI) protocol.
Design/Methods: We performed a retrospective chart review for all neonates who received TH from January 2014-March 2020 at Brigham and Women’s Hospital. MRV was routinely performed for cooled neonates with NE between April 2018 and March 2020. Demographic and clinical data of the study cohort were compared between those who were born before the implementation of routine MRV (January 2014-March 2018) and those born after the implementation of routine MRV (April 2018-March 2020). Incidence of CSVT detection was compared between these two groups.
Results: There were 291 babies cooled during the study period. Demographic and clinical data of the study cohort are provided in Table 1. Before the routine use of MRV, 209 babies were cooled, and 25 (12%) of them had MRV. Only one baby was diagnosed with CVST in this period, and it was initially detected with MRI and then confirmed with MRV. Following the routine inclusion of MRV in the imaging protocol in April 2018, 82 neonates were cooled. Of these 82, 74 (90%) had MRV performed. None of these neonates were diagnosed with CVST. Out of the 99 neonates with MRV, 15 showed severe cerebral veins asymmetry. Representative MRI and MRV scans of the infant with CVST and another infant with asymmetry but no CVST are shown in Figure 1.Conclusion(s): Incidence of CVST in neonates receiving TH for NE may not be as common as previously reported. Routine MRV has not been associated with increased detection of CVST. 1. Radicioni, M., et al., Cerebral Sinovenous Thrombosis in the Asphyxiated Cooled Infants: A Prospective Observational Study. Pediatr Neurol, 2017.
Table 1: Demographic and Clinical Data of the Cohort.png) Abbreviations: NE, neonatal encephalopathy; UA, umbilical artery; UV, umbilical venous; BD, base deficit
Abbreviations: NE, neonatal encephalopathy; UA, umbilical artery; UV, umbilical venous; BD, base deficit
Note: Data are presented as n (%) except
a Mean +/- SD and
b Median (Interquartile Range)
Figure 1: MRI and MRV images of the Case 1 (the baby diagnosed with CVST, panels A-D) and Case 2 (a baby with asymmetry on MRV but no CVST, panels E-H)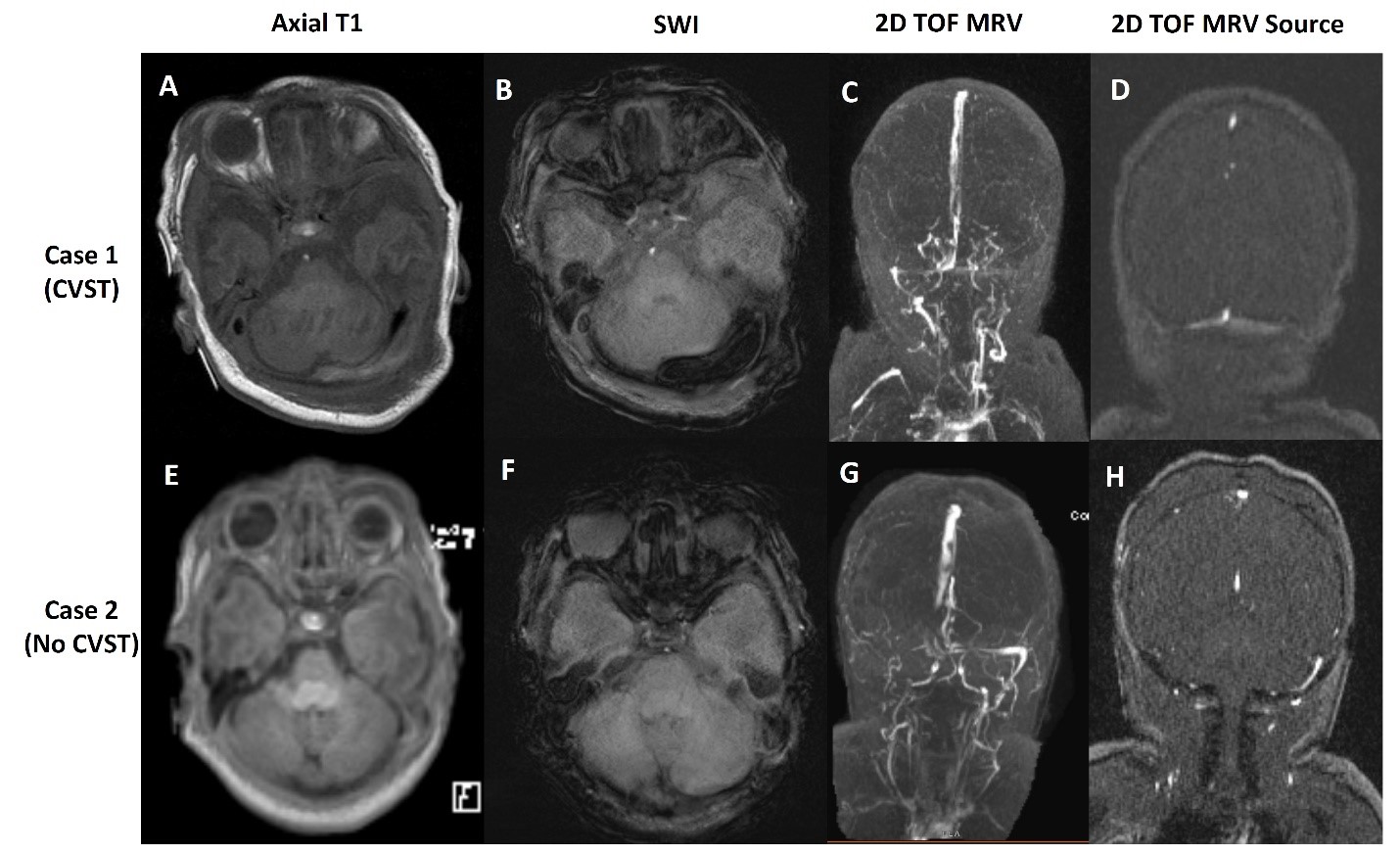 Case 1: Demonstration of linear hyperintensity on Axial T1(A) and susceptibility on SWI (B) in the region of the left transverse sinus not associated with significant asymmetry on MRV (C and D)
Case 1: Demonstration of linear hyperintensity on Axial T1(A) and susceptibility on SWI (B) in the region of the left transverse sinus not associated with significant asymmetry on MRV (C and D)
Case 2: Demonstration of absence of flow in the right transverses and sigmoid sinuses on MRV (G and H) in absence of clear corresponding thrombosis in T1 and SWI sequences (E and F)
Abbreviations: SWI, Susceptibility weighted imaging; TOF, Time of flight
Objective: To investigate the frequency and incidence of CVST diagnoses before and after implementation of routine MRV into the post-rewarming magnetic resonance imaging (MRI) protocol.
Design/Methods: We performed a retrospective chart review for all neonates who received TH from January 2014-March 2020 at Brigham and Women’s Hospital. MRV was routinely performed for cooled neonates with NE between April 2018 and March 2020. Demographic and clinical data of the study cohort were compared between those who were born before the implementation of routine MRV (January 2014-March 2018) and those born after the implementation of routine MRV (April 2018-March 2020). Incidence of CSVT detection was compared between these two groups.
Results: There were 291 babies cooled during the study period. Demographic and clinical data of the study cohort are provided in Table 1. Before the routine use of MRV, 209 babies were cooled, and 25 (12%) of them had MRV. Only one baby was diagnosed with CVST in this period, and it was initially detected with MRI and then confirmed with MRV. Following the routine inclusion of MRV in the imaging protocol in April 2018, 82 neonates were cooled. Of these 82, 74 (90%) had MRV performed. None of these neonates were diagnosed with CVST. Out of the 99 neonates with MRV, 15 showed severe cerebral veins asymmetry. Representative MRI and MRV scans of the infant with CVST and another infant with asymmetry but no CVST are shown in Figure 1.Conclusion(s): Incidence of CVST in neonates receiving TH for NE may not be as common as previously reported. Routine MRV has not been associated with increased detection of CVST. 1. Radicioni, M., et al., Cerebral Sinovenous Thrombosis in the Asphyxiated Cooled Infants: A Prospective Observational Study. Pediatr Neurol, 2017.
Table 1: Demographic and Clinical Data of the Cohort
.png) Abbreviations: NE, neonatal encephalopathy; UA, umbilical artery; UV, umbilical venous; BD, base deficit
Abbreviations: NE, neonatal encephalopathy; UA, umbilical artery; UV, umbilical venous; BD, base deficitNote: Data are presented as n (%) except
a Mean +/- SD and
b Median (Interquartile Range)
Figure 1: MRI and MRV images of the Case 1 (the baby diagnosed with CVST, panels A-D) and Case 2 (a baby with asymmetry on MRV but no CVST, panels E-H)
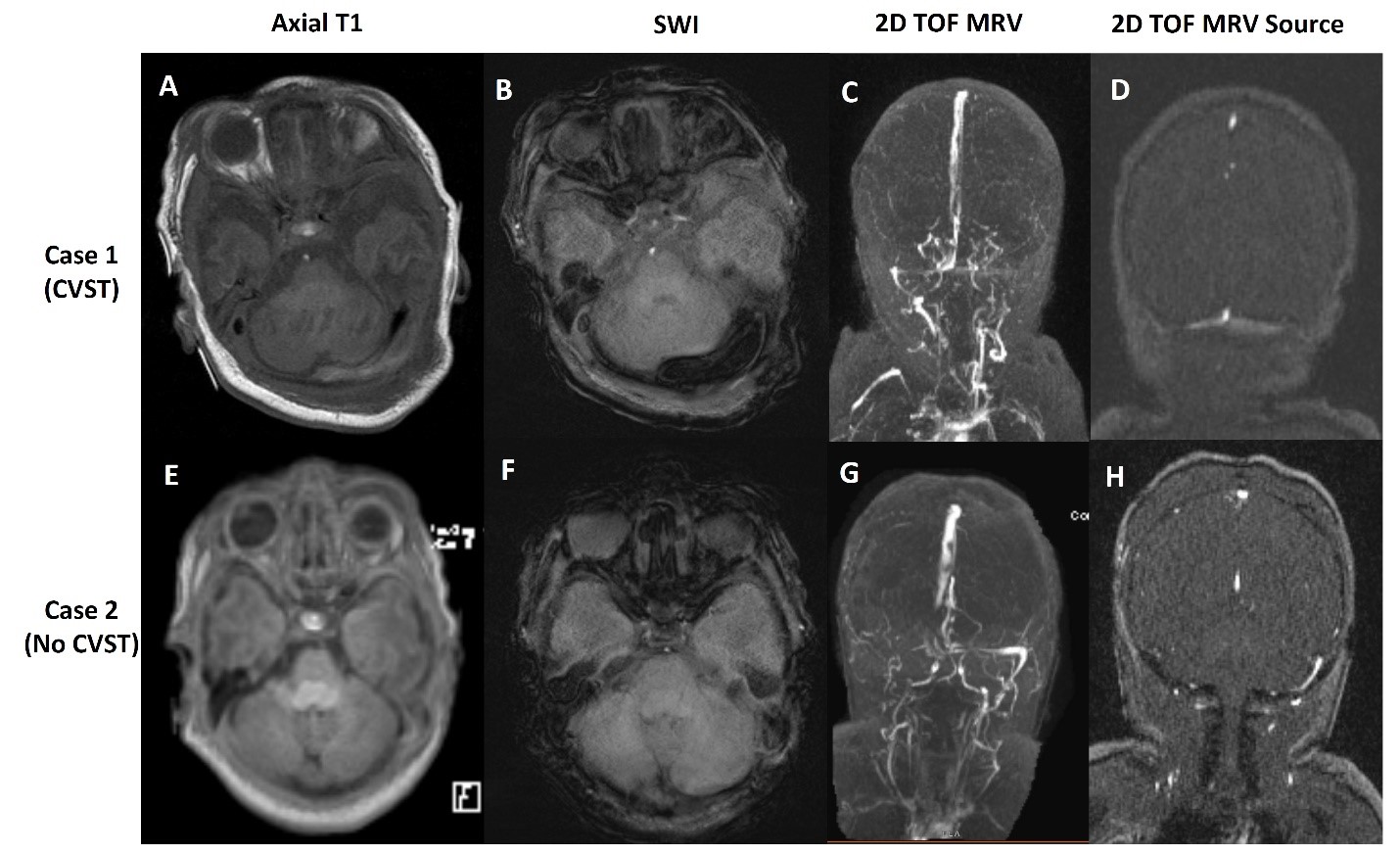 Case 1: Demonstration of linear hyperintensity on Axial T1(A) and susceptibility on SWI (B) in the region of the left transverse sinus not associated with significant asymmetry on MRV (C and D)
Case 1: Demonstration of linear hyperintensity on Axial T1(A) and susceptibility on SWI (B) in the region of the left transverse sinus not associated with significant asymmetry on MRV (C and D)Case 2: Demonstration of absence of flow in the right transverses and sigmoid sinuses on MRV (G and H) in absence of clear corresponding thrombosis in T1 and SWI sequences (E and F)
Abbreviations: SWI, Susceptibility weighted imaging; TOF, Time of flight
