Emergency Medicine: Quality Improvement
Category: Abstract Submission
Emergency Medicine XV
65 - Fill don’t spill: reduction in time to pelvic ultrasound for adolescent females with lower abdominal pain in the emergency department
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 65
Publication Number: 65.408
Publication Number: 65.408
Rebecca S. Green, Boston Children's Hospital, Boston, MA, United States; Rachelle El Helou, Boston Children's Hospital, Bostonq, MA, United States; Jheanelle McKay, Boston Children's Hospital, Boston, MA, United States; Megan Gerling, Boston Children's Hospital, Boston, MA, United States; Matthew A. Eisenberg, Boston Children's Hospital, Boston, MA, United States; joel Hudgins, Boston Children's Hospital, Boston, MA, United States

Rebecca S. Green, MD
Clinical fellow
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Transabdominal pelvic ultrasound (US) is the preferred imaging modality for female patients with lower abdominal pain presenting to the pediatric emergency department (ED) with suspected ovarian pathology. This resource-intensive approach requires a full bladder for optimal sonographic windows, which may prolong length of stay (LOS) and delay time-sensitive diagnoses.
Objective: To reduce ED roomed time to US completion by 25% over a 9-month period for female patients ≥ 11 years undergoing pelvic US in the ED.
Design/Methods:
We conducted a quality improvement initiative beginning in July 2021 to standardize bladder filling for patients undergoing pelvic US as part of a diagnostic workup for lower abdominal pain in a quaternary care pediatric ED. Our multidisciplinary group created a driver diagram to identify improvement opportunities (Figure 1). Interventions included optimizing and increasing use of an ED abdominal pain and bladder filling order set within the electronic medical record. The order set contained two pre-checked 20 mL/kg normal saline (NS) boluses in an effort to standardize the initial IV fluid orders. Educational interventions included information sessions during shifts, e-mail campaigns and ED posters. Data were collected for outcome measures (ED roomed time to US completion and ED LOS), process measures (% use of both abdominal pain and bladder filling order sets) and a balancing measure (cancelled NS bolus orders not required for bladder filling). Statistical process control methodology was used to assess differences between baseline data and post-intervention periods.
Results:
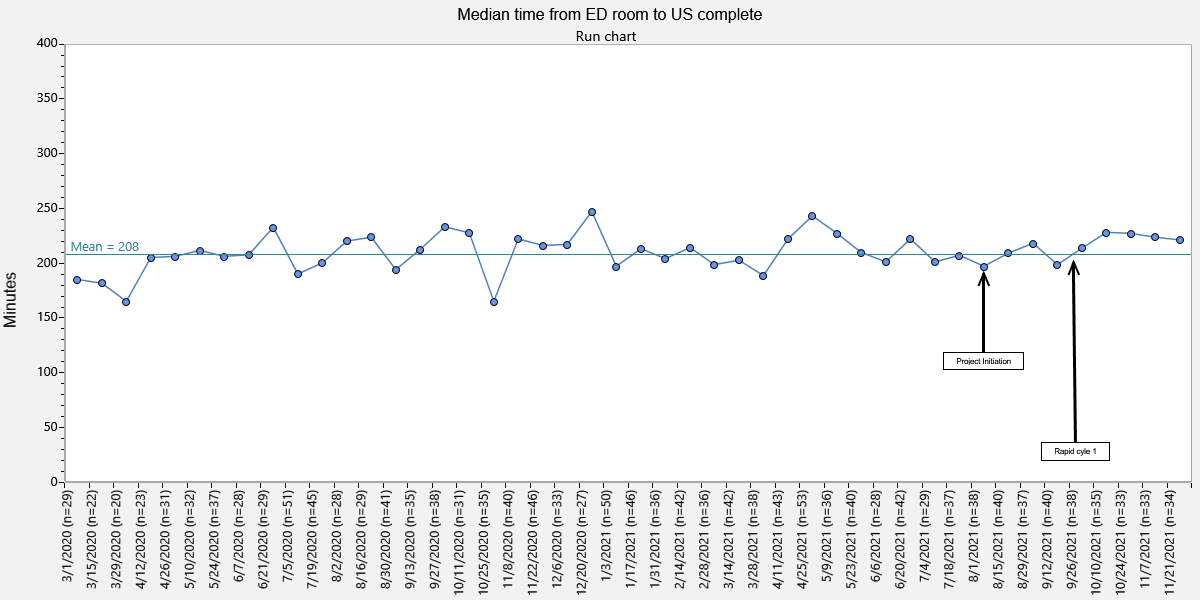
During a five-month period (July – November 2021), we identified 394 patients who underwent pelvic US with a median of 208 minutes for ED roomed time to US completion (Figure 2). After plan-do-study-act (PDSA) cycle #1, improvement was seen in the use of the bladder filling order set indicated by the shift in the centerline (Figure 3). No change was observed in ED roomed time to US completion, ED LOS or use of abdominal pain order set nor any increase in cancelled NS boluses.
Conclusion(s):
This ongoing study showed an increase in usage of a bladder filling order set which may be a promising intervention to reduce ED roomed time to US completion. The lack of improvement in time to US and LOS after only 3 months from the first intervention may be attributable to current ED volume and staffing challenges. Future PDSA cycles in this project will target optimizing bladder filling by reducing IV fluid delivery time and increasing furosemide usage.
Figure 1. Key driver diagram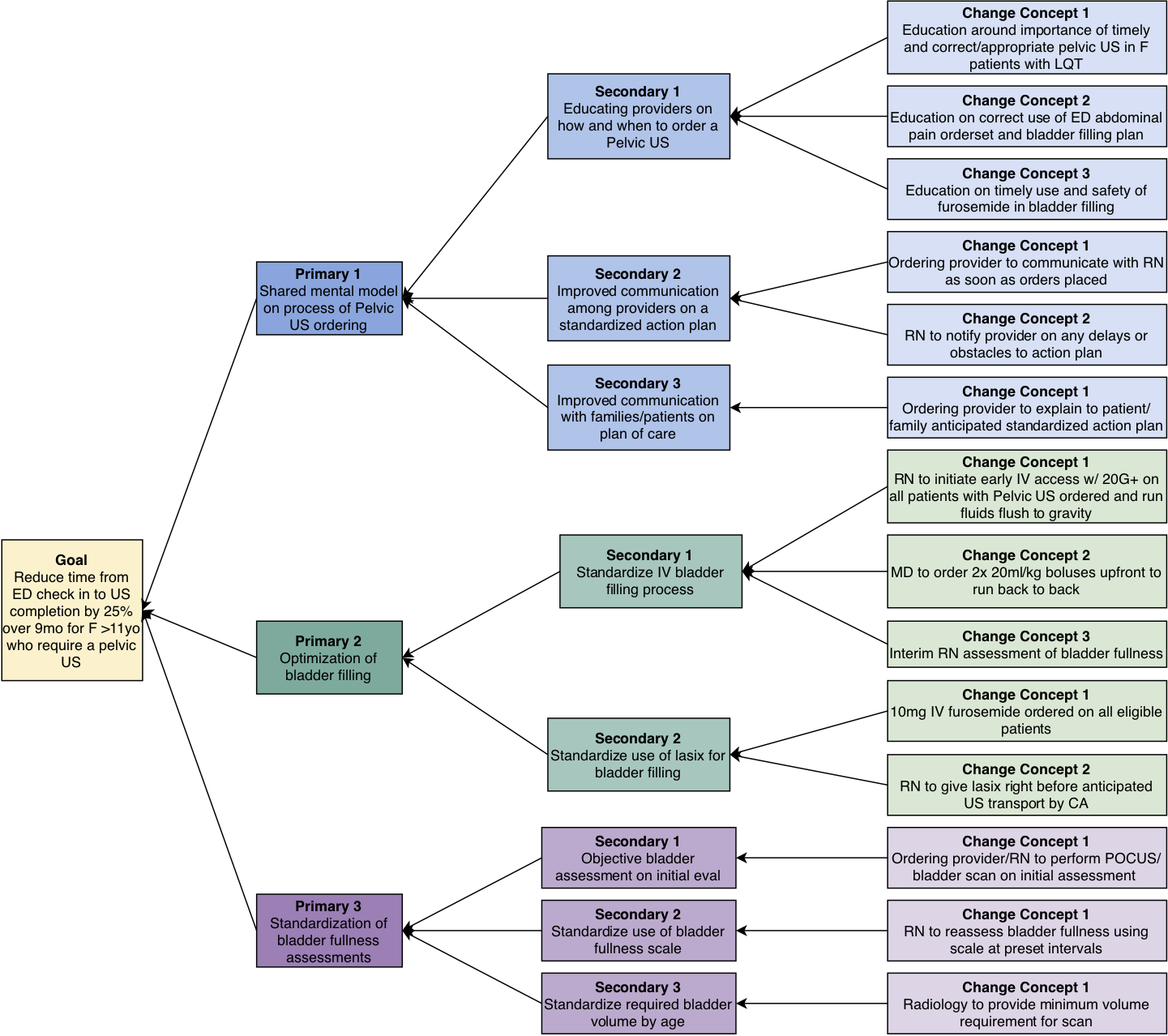
Figure 2: Median ED roomed time to US completion (minutes)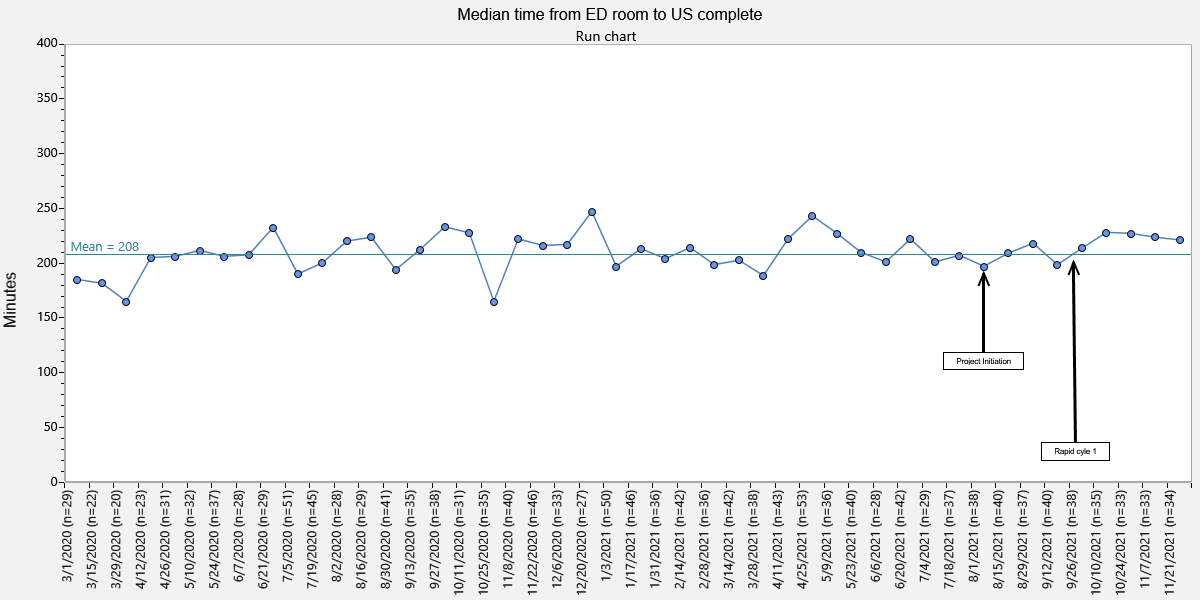
Objective: To reduce ED roomed time to US completion by 25% over a 9-month period for female patients ≥ 11 years undergoing pelvic US in the ED.
Design/Methods:
We conducted a quality improvement initiative beginning in July 2021 to standardize bladder filling for patients undergoing pelvic US as part of a diagnostic workup for lower abdominal pain in a quaternary care pediatric ED. Our multidisciplinary group created a driver diagram to identify improvement opportunities (Figure 1). Interventions included optimizing and increasing use of an ED abdominal pain and bladder filling order set within the electronic medical record. The order set contained two pre-checked 20 mL/kg normal saline (NS) boluses in an effort to standardize the initial IV fluid orders. Educational interventions included information sessions during shifts, e-mail campaigns and ED posters. Data were collected for outcome measures (ED roomed time to US completion and ED LOS), process measures (% use of both abdominal pain and bladder filling order sets) and a balancing measure (cancelled NS bolus orders not required for bladder filling). Statistical process control methodology was used to assess differences between baseline data and post-intervention periods.
Results:
During a five-month period (July – November 2021), we identified 394 patients who underwent pelvic US with a median of 208 minutes for ED roomed time to US completion (Figure 2). After plan-do-study-act (PDSA) cycle #1, improvement was seen in the use of the bladder filling order set indicated by the shift in the centerline (Figure 3). No change was observed in ED roomed time to US completion, ED LOS or use of abdominal pain order set nor any increase in cancelled NS boluses.
Conclusion(s):
This ongoing study showed an increase in usage of a bladder filling order set which may be a promising intervention to reduce ED roomed time to US completion. The lack of improvement in time to US and LOS after only 3 months from the first intervention may be attributable to current ED volume and staffing challenges. Future PDSA cycles in this project will target optimizing bladder filling by reducing IV fluid delivery time and increasing furosemide usage.
Figure 1. Key driver diagram
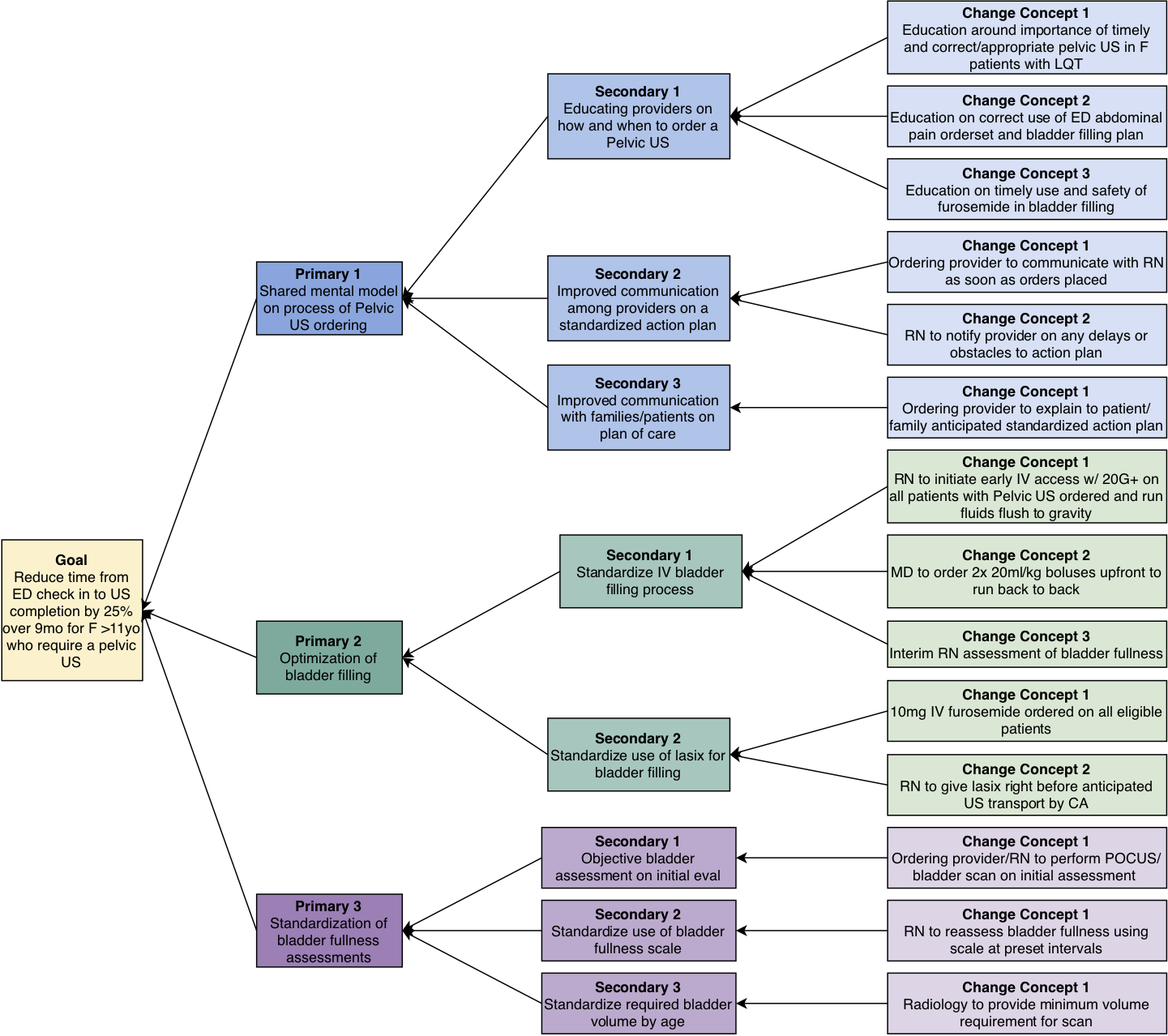
Figure 2: Median ED roomed time to US completion (minutes)