General Pediatrics: All Areas
Category: Abstract Submission
General Pediatrics V
100 - Atopic Dermatitis: Building a System of Care. An Ohio AAP Learning Collaborative
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 100
Publication Number: 100.409
Publication Number: 100.409
Chris Peltier, Cincinnati Children's Hospital Medical Center, South Lebanon, OH, United States; Kara Shah, Optima Dermatology, Cincinnati, OH, United States; Emily Harris, University of Cincinnati College of Medicine, Cincinnati, OH, United States; Alexandra Miller, Ohio Chapter, American Academy of Pediatrics, Columbus, OH, United States; Hayley Southworth, Ohio Chapter American Academy of Pediatrics, Columbus, OH, United States

Chris Peltier, MD, FAAP (he/him/his)
Associate Professor of Pediatrics
Cincinnati Children's Hospital Medical Center
South Lebanon, Ohio, United States
Presenting Author(s)
Background: Atopic dermatitis (AD) is a common, chronic inflammatory skin disease that affects 10-15% of children in the U.S. Approximately 1:3 children with AD experience moderate to severe disease, which can negatively impact quality of life. Under-treated AD is associated with sleep disturbances and anxiety disorders (for the child and caregiver). Empowering families to manage this chronic skin condition is a primary function of the Primary Care Provider (PCP)
Objective: Global
Aim: To increase capacity of PCPs to improve family adherence to evidence-based treatments for AD by addressing identified social-emotional factors, and creating family-centered educational resources.,
Specific
Aims: In visits with patients with a chief complaint or previous diagnosis of AD: 85% of providers will report an increase in confidence in discussing AD; implement screening for patients in 80% of visits; utilize educational materials with 90% of patients; utilize AD plan of care in 90% of patients; decrease referrals of AD patients with mild to moderate disease to dermatologist by 75%
Design/Methods: Thirty four providers randomly reviewed pediatric patient charts for patients with chief complaint of or prior diagnosis of AD at well and ill visits for baseline and action period data. Resources were created to educate families. An AD action plan was created and implemented into practice. An AD Chart Review Tool was created to capture de-identified process metrics on AD symptom assessment, counseling, goal setting and provision of patient resources. Data was collected, analyzed, and reported to participants monthly to assist in monitoring progress. Project participants had access to performance data for quality improvement purposes. Providers completed four PDSA cycles for tests of changes as they incorporated project elements into daily practices
Results: All project leaders reported that they were “very confident” discussing AD and resources with families at project end (85% increase). Use of AD resources for families increased 10% to 63%. Use of an AD Action Plan increased 3% to 62%. While referrals to a specialist did increase from 2% to 6%, they remained under 10%Conclusion(s): The program launched a quality improvement QI project recruiting 11 pediatric primary care practices across two states. Nearly all the objective measures increased significantly over baseline. We demonstrated that a low number of specialist referrals can be maintained, aligning with a focus on ensuring proper management of mild AD in the primary care setting. Future steps include creating new resources to focus on health equity as it relates to AD
AD Resources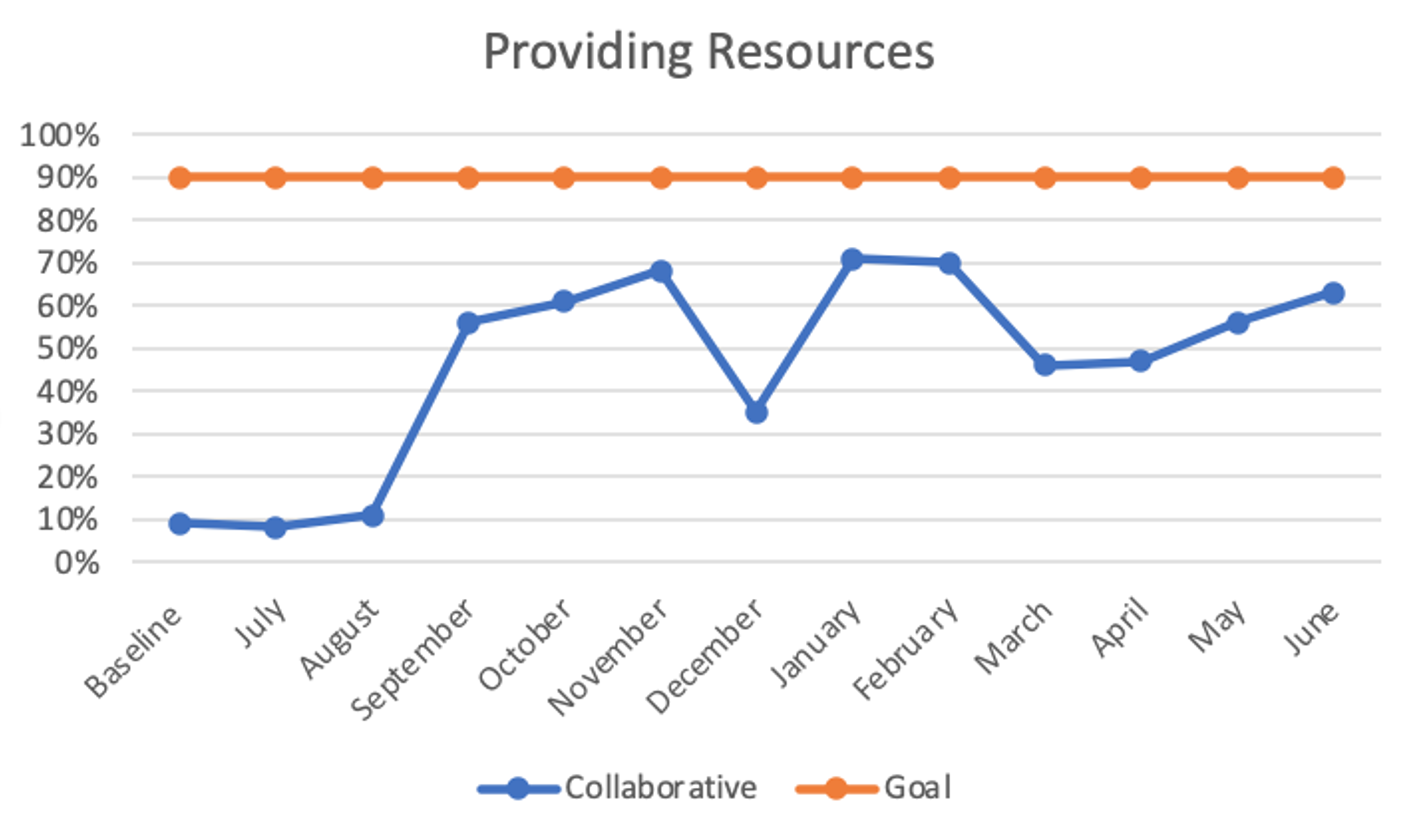 Use of AD resources for families increased 10% to 63%.
Use of AD resources for families increased 10% to 63%.
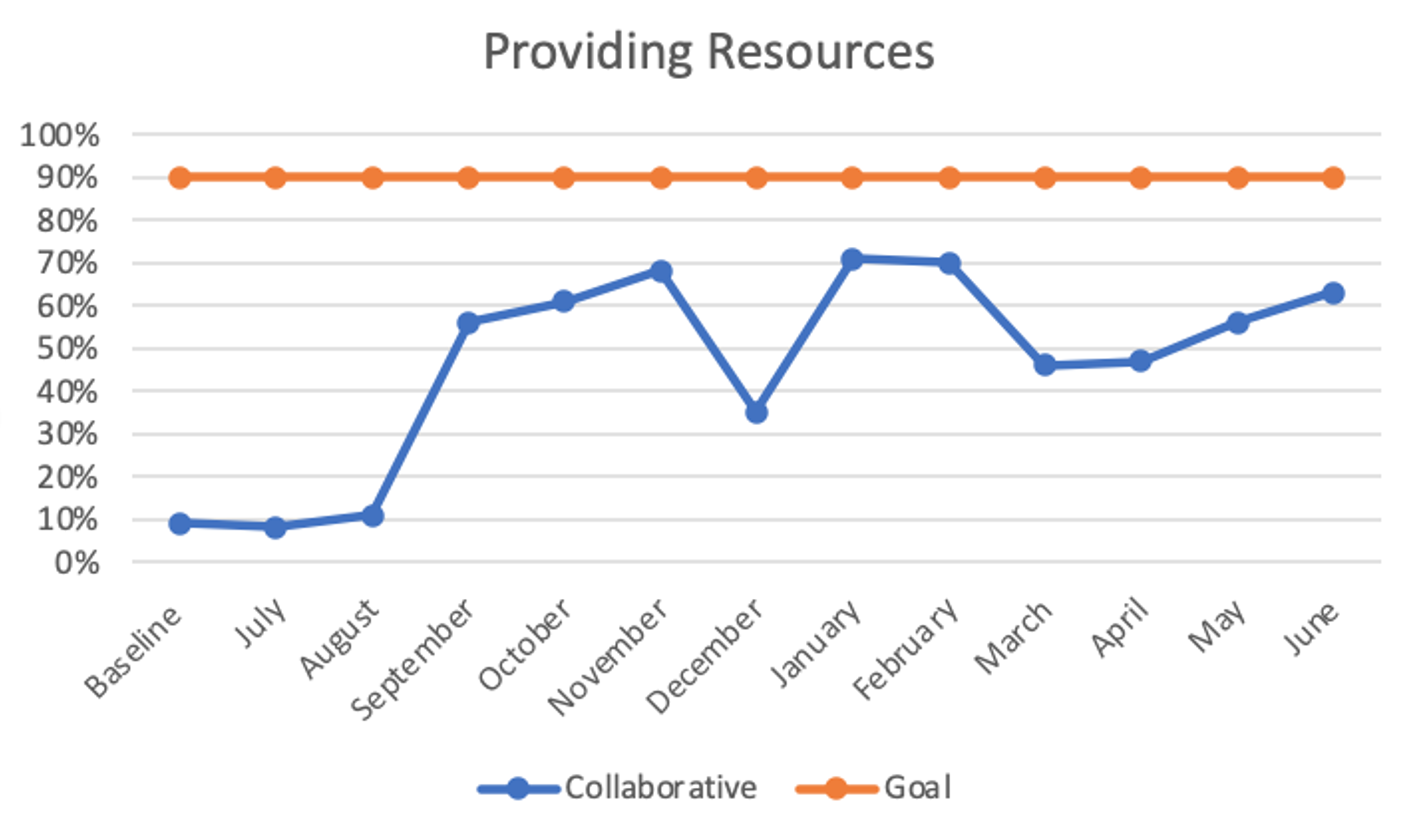
Use of an AD Action Plan.png) Use of an AD Action Plan increased 3% to 62%
Use of an AD Action Plan increased 3% to 62%
Objective: Global
Aim: To increase capacity of PCPs to improve family adherence to evidence-based treatments for AD by addressing identified social-emotional factors, and creating family-centered educational resources.,
Specific
Aims: In visits with patients with a chief complaint or previous diagnosis of AD: 85% of providers will report an increase in confidence in discussing AD; implement screening for patients in 80% of visits; utilize educational materials with 90% of patients; utilize AD plan of care in 90% of patients; decrease referrals of AD patients with mild to moderate disease to dermatologist by 75%
Design/Methods: Thirty four providers randomly reviewed pediatric patient charts for patients with chief complaint of or prior diagnosis of AD at well and ill visits for baseline and action period data. Resources were created to educate families. An AD action plan was created and implemented into practice. An AD Chart Review Tool was created to capture de-identified process metrics on AD symptom assessment, counseling, goal setting and provision of patient resources. Data was collected, analyzed, and reported to participants monthly to assist in monitoring progress. Project participants had access to performance data for quality improvement purposes. Providers completed four PDSA cycles for tests of changes as they incorporated project elements into daily practices
Results: All project leaders reported that they were “very confident” discussing AD and resources with families at project end (85% increase). Use of AD resources for families increased 10% to 63%. Use of an AD Action Plan increased 3% to 62%. While referrals to a specialist did increase from 2% to 6%, they remained under 10%Conclusion(s): The program launched a quality improvement QI project recruiting 11 pediatric primary care practices across two states. Nearly all the objective measures increased significantly over baseline. We demonstrated that a low number of specialist referrals can be maintained, aligning with a focus on ensuring proper management of mild AD in the primary care setting. Future steps include creating new resources to focus on health equity as it relates to AD
AD Resources
 Use of AD resources for families increased 10% to 63%.
Use of AD resources for families increased 10% to 63%.Use of an AD Action Plan
.png) Use of an AD Action Plan increased 3% to 62%
Use of an AD Action Plan increased 3% to 62%