Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine XI
400 - Emergency Medical Services Treatment of Refugee Children
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 400
Publication Number: 400.315
Publication Number: 400.315
Anna Abrams, University of Colorado School of Medicine, Denver, CO, United States; Shivani Kapur, Children's Hospital Los Angeles, Los Angeles, CA, United States; Margaret Tashjian, University of Colorado School of Medicine, Aurora, CO, United States; Jan Leonard, University of Colorado Anschutz Medical Campus, Aurora, CO, United States; Janine Young, Denver Health and Hospitals, Denver, CO, United States; Sarah E. Brewer, University of Colorado School of Medicine, Aurora, CO, United States; Kathleen Adelgais, University of Colorado School of Medicine, Aurora, CO, United States
Anna Abrams, MD (she/her/hers)
Pediatric Emergency medicine Fellow
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: Refugee children face difficulties accessing quality healthcare due to a lack of adequate interpretation services, transportation, and health insurance. These barriers potentially result in misdiagnoses or delays in care. In the out-of-hospital setting, delays in transport can result in increased morbidity and mortality. The impact of barriers faced by refugee children on outcomes of care by Emergency Medical Services (EMS) is unknown.
Objective: To compare prehospital scene time, clinical interventions, and ED and EMS diagnosis concordance during EMS encounters for refugee and non-refugee children.
Design/Methods: This is a matched case-control study of refugee children with a domestic medical examination from a refugee services clinic between 2014-2019 transported by ground from the scene via EMS to a single center ED. We performed 1:2 matching for age (within 1 year), date of service (within 1 year), insurance (public vs private), and EMS transport agency. The primary outcome was a difference in scene time (minutes) with a negative binomial analysis adjusting for primary language. Secondary outcomes included EMS and ED interventions, and EMS and ED diagnosis concordance. Diagnosis concordance and agreement was assessed by 2 independent reviewers.
Results: We included 20 refugee and 40 matched non-refugee EMS encounters. Top documented primary languages among refugees were Nepali (25%), English (20%), and Arabic (10%); 35% of non-refugees were Spanish speaking (table 1). There was no difference in median or adjusted scene time (11 minutes, rate ratio 1.18, 95% CI 0.93-1.50). Intravenous (IV) access was attempted in 20% of refugees and 31% of non-refugees yet IV access was utilized in 75% of refugees and only 20% of non-refugees. There were no differences between groups receiving other prehospital interventions (table 2) or ED interventions (Table 3). EMS and ED diagnoses were concordant in 90% of encounters independent of refugee status with 85% agreement. The top EMS Primary Impression for refugees was General Illness (29%), compared to Behavioral for non-refugees (28%). EMS reported barriers to care more often for refugees (60% vs 15%).Conclusion(s): Despite higher reports of barriers to care, there was no difference in prehospital scene time or frequency of EMS and ED diagnosis concordance. When obtained, IV access was more likely to be utilized in refugee children suggesting a higher threshold for placement. Further investigation is needed to understand EMS/ED provider perceptions of barriers to care of refugees in the prehospital setting.
Anna Abrams CVAnna_Abrams_PEM_CV.pdf
Emergency Medical Services (EMS) Encounter Characteristics and Interventions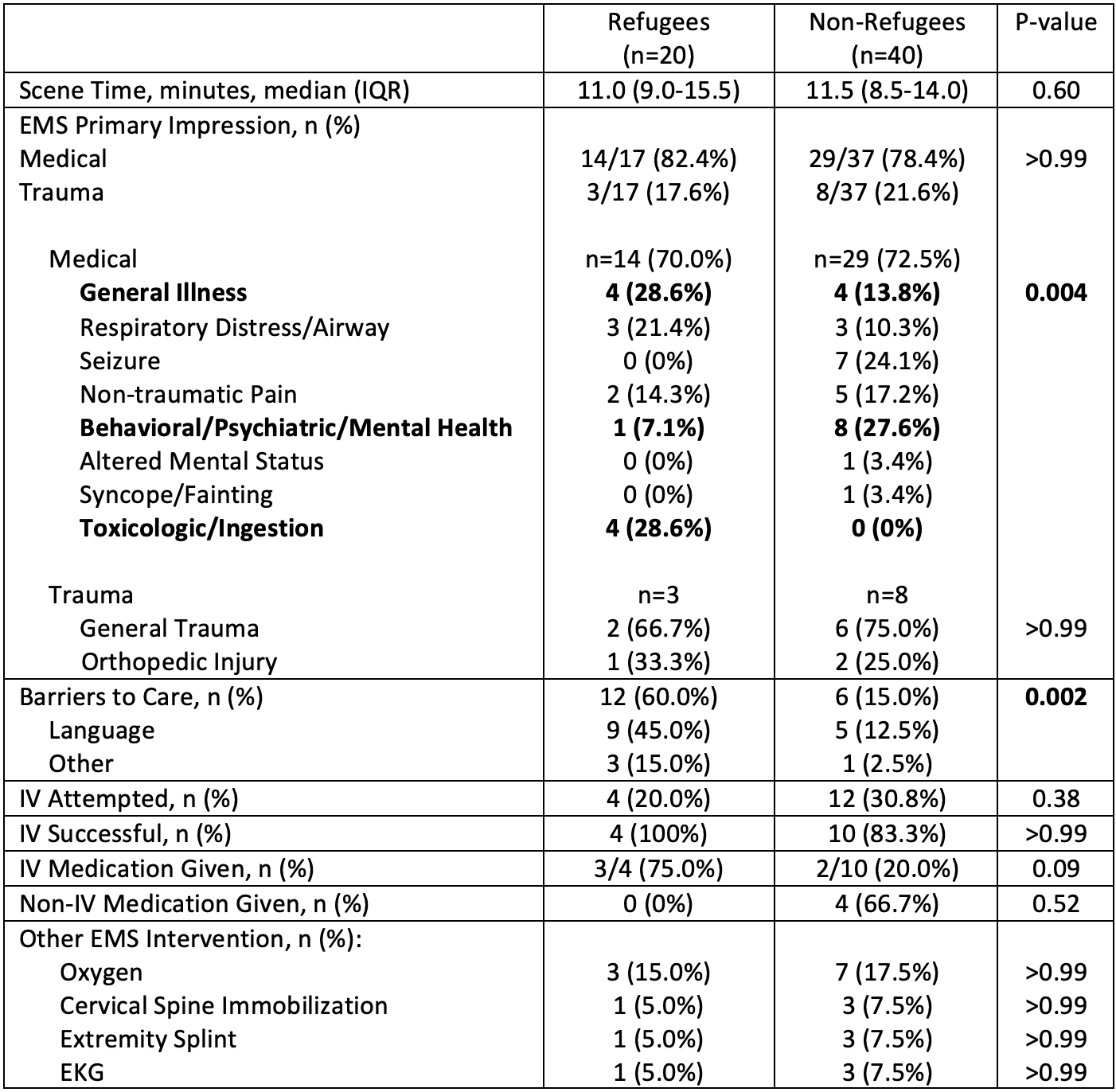 Number of missing data points for: Scene time (n=4, all in the non-refugee group); Distance to hospital (n=1, in refugee group)
Number of missing data points for: Scene time (n=4, all in the non-refugee group); Distance to hospital (n=1, in refugee group)
Objective: To compare prehospital scene time, clinical interventions, and ED and EMS diagnosis concordance during EMS encounters for refugee and non-refugee children.
Design/Methods: This is a matched case-control study of refugee children with a domestic medical examination from a refugee services clinic between 2014-2019 transported by ground from the scene via EMS to a single center ED. We performed 1:2 matching for age (within 1 year), date of service (within 1 year), insurance (public vs private), and EMS transport agency. The primary outcome was a difference in scene time (minutes) with a negative binomial analysis adjusting for primary language. Secondary outcomes included EMS and ED interventions, and EMS and ED diagnosis concordance. Diagnosis concordance and agreement was assessed by 2 independent reviewers.
Results: We included 20 refugee and 40 matched non-refugee EMS encounters. Top documented primary languages among refugees were Nepali (25%), English (20%), and Arabic (10%); 35% of non-refugees were Spanish speaking (table 1). There was no difference in median or adjusted scene time (11 minutes, rate ratio 1.18, 95% CI 0.93-1.50). Intravenous (IV) access was attempted in 20% of refugees and 31% of non-refugees yet IV access was utilized in 75% of refugees and only 20% of non-refugees. There were no differences between groups receiving other prehospital interventions (table 2) or ED interventions (Table 3). EMS and ED diagnoses were concordant in 90% of encounters independent of refugee status with 85% agreement. The top EMS Primary Impression for refugees was General Illness (29%), compared to Behavioral for non-refugees (28%). EMS reported barriers to care more often for refugees (60% vs 15%).Conclusion(s): Despite higher reports of barriers to care, there was no difference in prehospital scene time or frequency of EMS and ED diagnosis concordance. When obtained, IV access was more likely to be utilized in refugee children suggesting a higher threshold for placement. Further investigation is needed to understand EMS/ED provider perceptions of barriers to care of refugees in the prehospital setting.
Anna Abrams CVAnna_Abrams_PEM_CV.pdf
Emergency Medical Services (EMS) Encounter Characteristics and Interventions
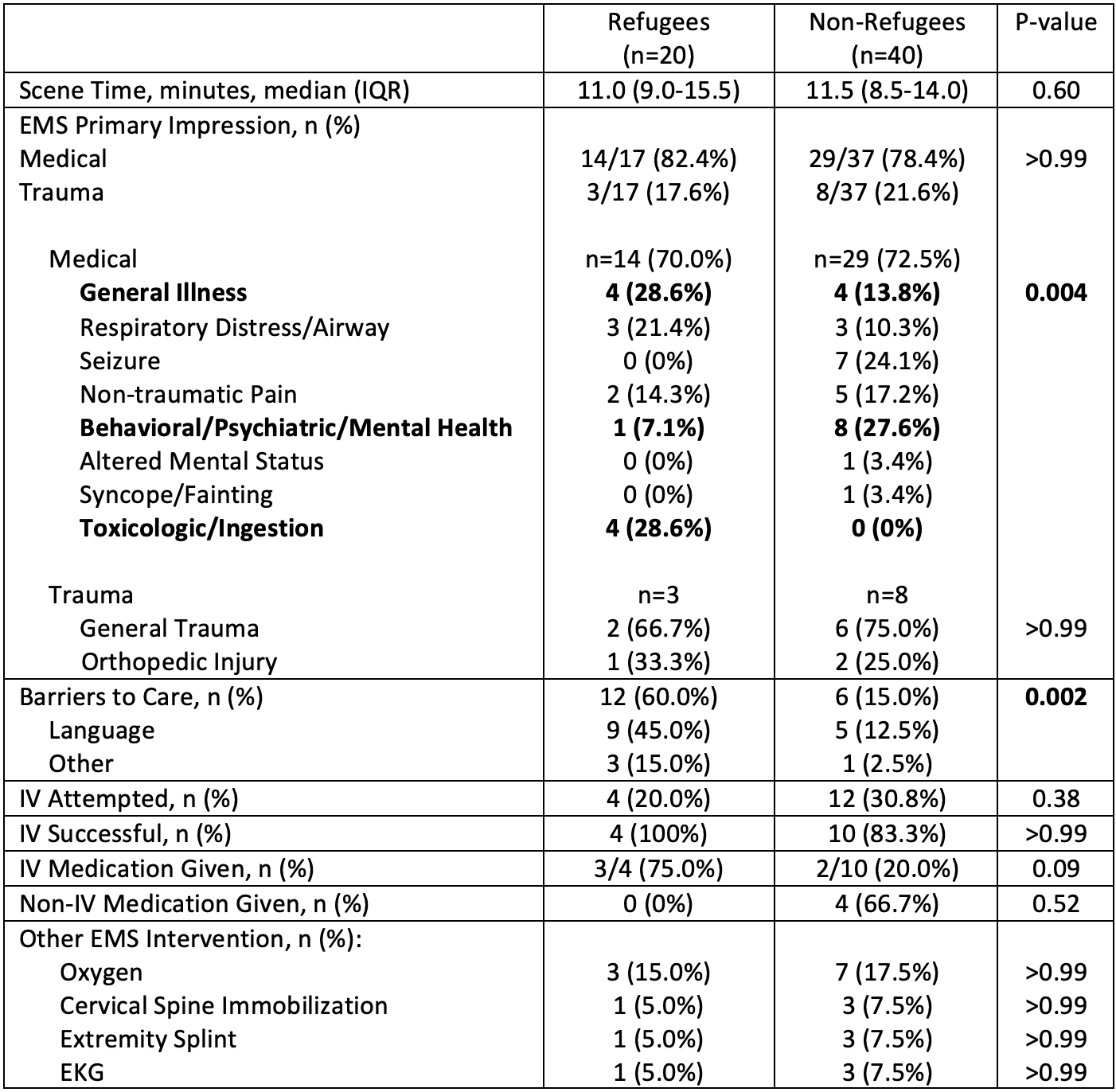 Number of missing data points for: Scene time (n=4, all in the non-refugee group); Distance to hospital (n=1, in refugee group)
Number of missing data points for: Scene time (n=4, all in the non-refugee group); Distance to hospital (n=1, in refugee group)