Medical Education: Fellow
Category: Abstract Submission
Medical Education 8 - Medical Education: Fellow II
227 - Escalation of Care Outside the ICU: Opportunities for Interprofessional Education
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 227
Publication Number: 227.332
Publication Number: 227.332
Lauren E. Castaneda, Children's Hospital Colorado, Denver, CO, United States; Justin M. Lockwood, University of Colorado School of Medicine, Aurora, CO, United States; Beth Wathen, Children's Hospital Colorado, DENVER, CO, United States; Angela S. Czaja, University of Colorado School of Medicine, Aurora, CO, United States

Lauren E. Castaneda, MD
Critical Care Fellow
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
Background: Interprofessional (IP) education may improve timeliness and effectiveness of care escalation outside the ICU, reducing in-hospital cardiac arrests & deaths, but is inconsistent in our institution.
Objective: To assess the learning needs of team members to inform an effective IP pediatric escalation of care curriculum.
Design/Methods: As initial steps of Kern’s model for curriculum development, we performed a cross-sectional study at a quaternary care pediatric hospital in Dec-Jan 2020. Acute care floor (residents, advanced practice providers, nurses) and PICU rapid response team members (RRT) were sent an anonymous electronic survey. Survey items, developed and refined by clinical and educational experts for clarity and content, focused on domains of self-efficacy, communication and competence related to care escalation practices. Team member responses were compared using chi2 analysis, significance defined as p < 0.05.
Results: 152 team members responded: 45 floor providers, 81 nurses and 26 RRT (response rate of 24%). All respondents had prior escalation experience, but more nurses reported no dedicated teaching sessions. All floor team members expressed confidence in recognizing a patient in need of escalation, though more providers reported experiencing discomfort with escalating concerns when compared to nurses. Nurses were more likely to immediately escalate compared to providers. Both groups reported the decision to escalate is influenced by the person to whom they are escalating and often had discomfort in expressing disagreement with supervisors. All respondents reported effective team communication and early recognition by bedside team as always contributory to successful escalation. Floor team members less frequently identified trust between team members as contributory to effective care. All respondents were less likely to identify systems-based issues as positive contributors. Most respondents indicated some interest in IP escalation of care educational exercises, with on-shift timing preferred.Conclusion(s): Pediatric acute care team members often care for patients requiring escalation, however dedicated education varies based on clinical role. Survey respondents identified early recognition of patient deterioration, effective communication between team members and the potential hierarchical influence as important areas of educational focus. An IP approach to education is valuable and should be considered to improve clinical care and patient outcomes.
Figure 1.png) Figure 1: RN vs Provider Education and Comfort in Care Escalation
Figure 1: RN vs Provider Education and Comfort in Care Escalation
Figure 2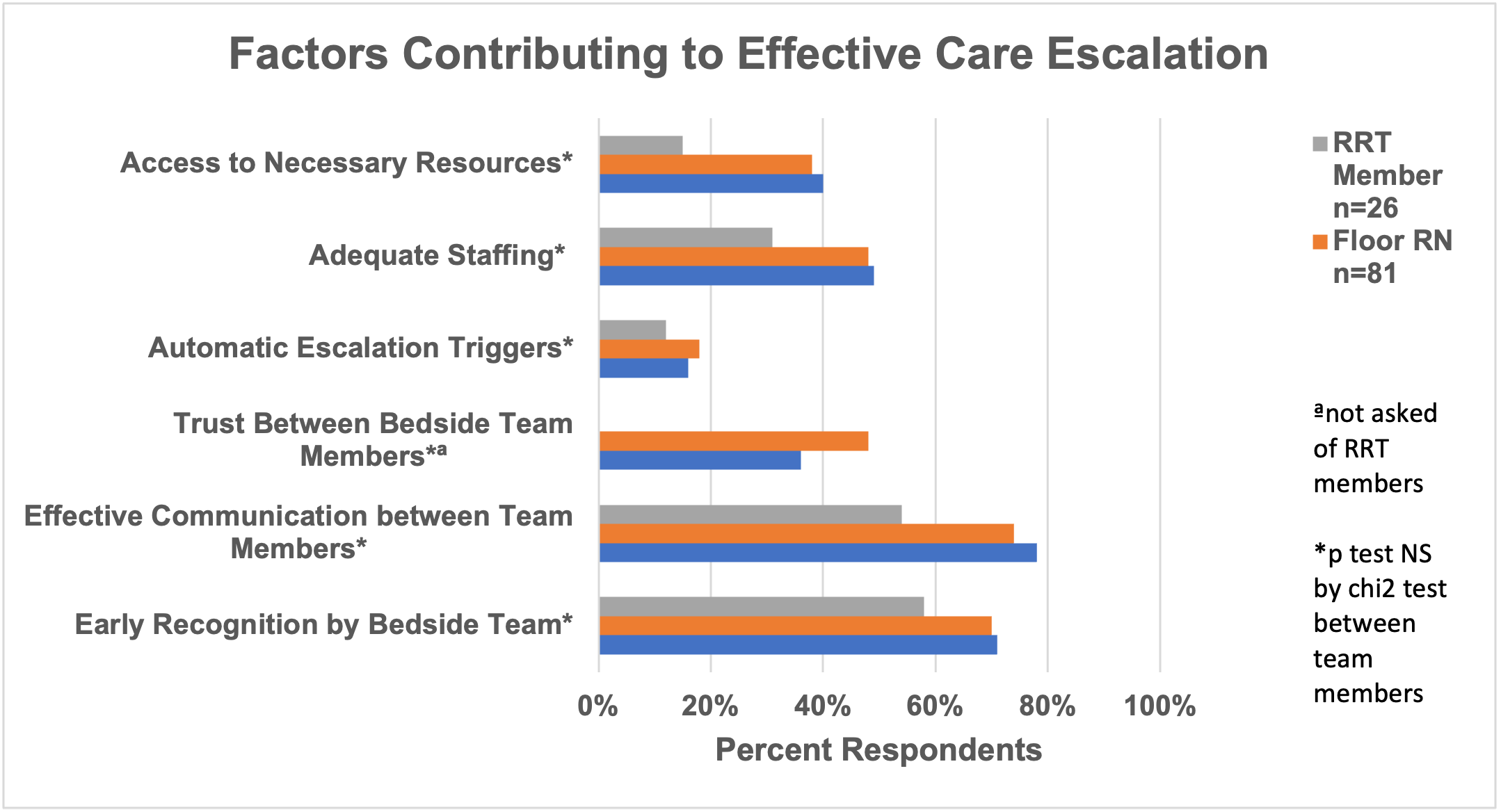 Figure 2: Perceived Factors Contributing to Effective Care Escalation
Figure 2: Perceived Factors Contributing to Effective Care Escalation
Objective: To assess the learning needs of team members to inform an effective IP pediatric escalation of care curriculum.
Design/Methods: As initial steps of Kern’s model for curriculum development, we performed a cross-sectional study at a quaternary care pediatric hospital in Dec-Jan 2020. Acute care floor (residents, advanced practice providers, nurses) and PICU rapid response team members (RRT) were sent an anonymous electronic survey. Survey items, developed and refined by clinical and educational experts for clarity and content, focused on domains of self-efficacy, communication and competence related to care escalation practices. Team member responses were compared using chi2 analysis, significance defined as p < 0.05.
Results: 152 team members responded: 45 floor providers, 81 nurses and 26 RRT (response rate of 24%). All respondents had prior escalation experience, but more nurses reported no dedicated teaching sessions. All floor team members expressed confidence in recognizing a patient in need of escalation, though more providers reported experiencing discomfort with escalating concerns when compared to nurses. Nurses were more likely to immediately escalate compared to providers. Both groups reported the decision to escalate is influenced by the person to whom they are escalating and often had discomfort in expressing disagreement with supervisors. All respondents reported effective team communication and early recognition by bedside team as always contributory to successful escalation. Floor team members less frequently identified trust between team members as contributory to effective care. All respondents were less likely to identify systems-based issues as positive contributors. Most respondents indicated some interest in IP escalation of care educational exercises, with on-shift timing preferred.Conclusion(s): Pediatric acute care team members often care for patients requiring escalation, however dedicated education varies based on clinical role. Survey respondents identified early recognition of patient deterioration, effective communication between team members and the potential hierarchical influence as important areas of educational focus. An IP approach to education is valuable and should be considered to improve clinical care and patient outcomes.
Figure 1
.png) Figure 1: RN vs Provider Education and Comfort in Care Escalation
Figure 1: RN vs Provider Education and Comfort in Care EscalationFigure 2
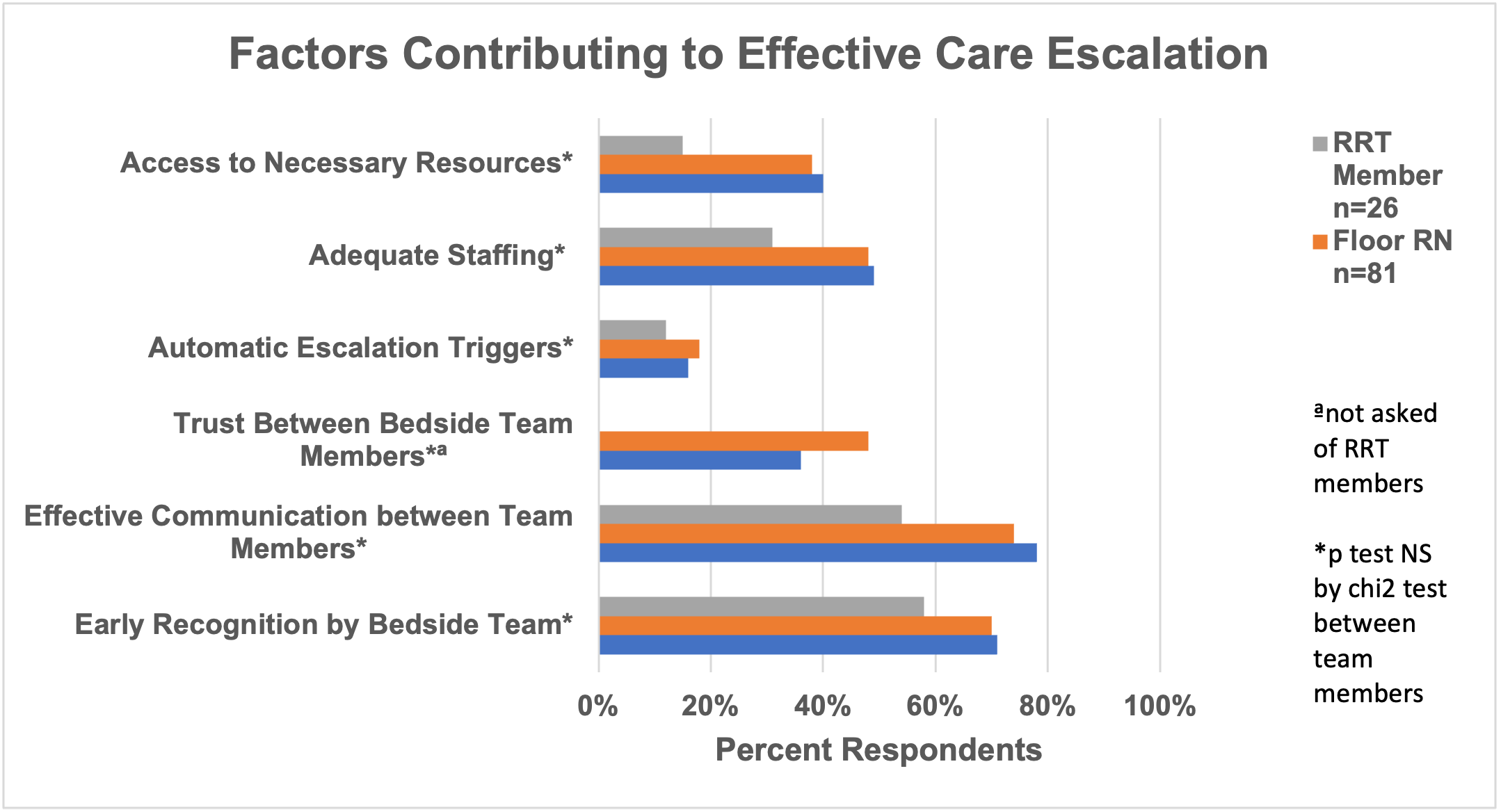 Figure 2: Perceived Factors Contributing to Effective Care Escalation
Figure 2: Perceived Factors Contributing to Effective Care Escalation