Back
Obesity
Category: Abstract Submission
Obesity I
514 - Risk for Potential Adverse Events among Hospitalized Children with Obesity
Saturday, April 23, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 514
Publication Number: 514.238
Publication Number: 514.238
Kathryn Kyler, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Matthew Hall, Children's Hospital Association, Lenexa, Kansas, KS, United States; Ann M. Davis, Center for Children's Healthy Lifestyles & Nutrition/ KU Medical Center, Kansas City, MO, United States; Elizabeth E. Halvorson, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston-Salem, NC, United States

Kathryn E. Kyler, MD, MS
Assistant Professor of Pediatrics
Children's Mercy Hospitals and Clinics
Kansas City, Missouri, United States
Presenting Author(s)
Background: Obesity may increase the risk of experiencing adverse events (AEs) during hospitalization, but studies examining specific AEs among children with obesity have mixed results. Global Assessment of Pediatric Patient Safety (GAPPS) is a validated tool identifying triggers (i.e., events indicating increased risk of AE) and actual AEs during hospitalization. An examination of GAPPS triggers indicating potential AEs in hospitalized children with obesity may provide targets for future research and quality improvement work.
Objective: To compare rates of AE triggers between hospitalized children with and without obesity.
Design/Methods: This was a retrospective study of children aged 2-17 years hospitalized for any reason at a single free-standing children’s hospital during 2017-2019. Children were categorized as having or not having obesity based on measured height/weight using Centers for Disease Control and Prevention definitions. The occurrence of 23 validated GAPPS triggers within the electronic health record were recorded for each encounter using an automated process. Proportions of encounters experiencing triggers were compared between weight categories using Chi square tests. Logistic regression was used to determine the odds of experiencing any AE trigger by weight category, adjusted for demographic and clinical characteristics.
Results: A total of 33,261 encounters were included, 15.5% of which were patients with obesity (Table 1). Occurrence of AE triggers ranged from very rare events (e.g., flumazenil administration, 4 occurrences during study period) to common events (e.g., 30-day readmission rates, 4,513 occurrences). Trigger rates varied by weight category for only 2 triggers examined, both occurring less frequently in children with obesity: oral vancomycin ordered (p=0.006), and inpatient death (p=0.010) (Table 2). Children with obesity had no increased odds of experiencing any category of AE trigger compared to children without obesity (Table 3).Conclusion(s): Hospitalized children with obesity experienced similar rates of AE triggers to those without obesity, indicating they may not be at higher risk of true AEs for the included triggers. However, this study did not assess actual AE rates, and did not include triggers requiring manual chart review or those specific to children with obesity (e.g., drug dosing errors). Future work should focus on identification of true AEs and triggers specifically tailored for children with obesity to elucidate how obesity modulates AE rates in hospitalized children.
Table 1. Cohort demographic and clinical characteristics by weight category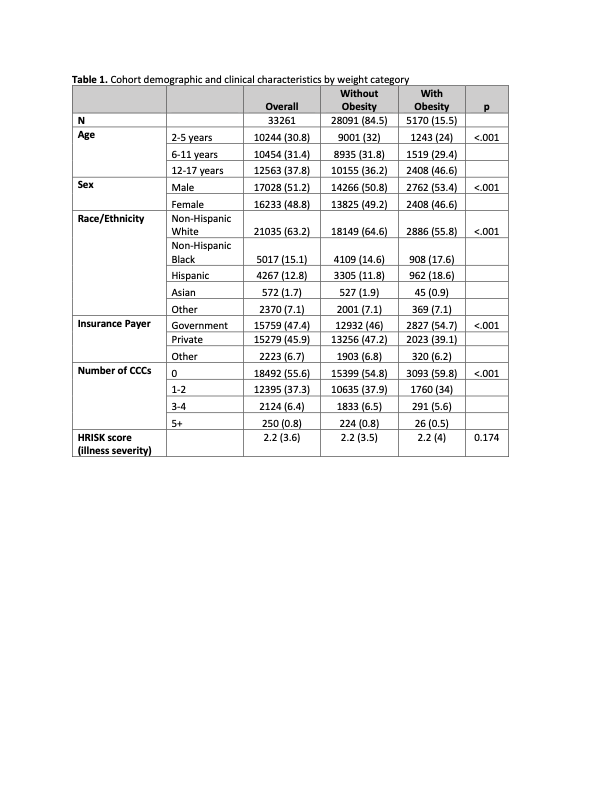
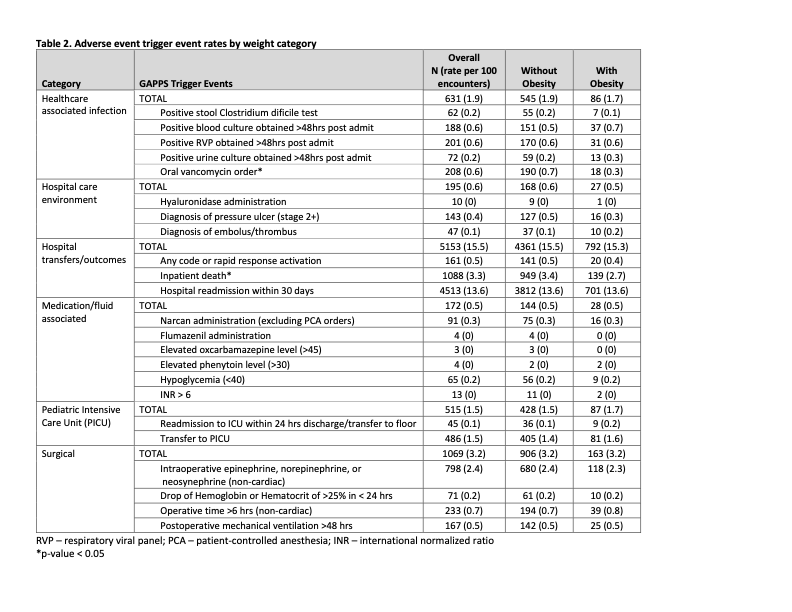
Table 2. Adverse event trigger event rates by weight category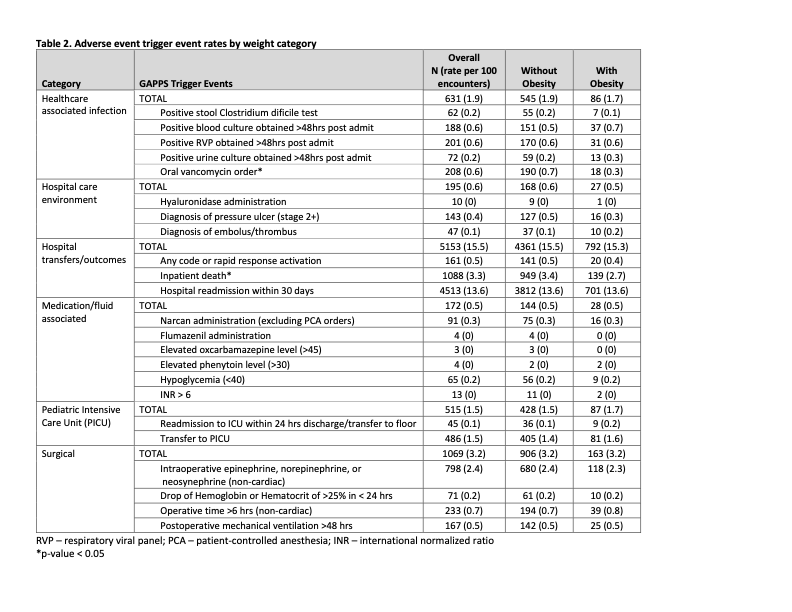
Objective: To compare rates of AE triggers between hospitalized children with and without obesity.
Design/Methods: This was a retrospective study of children aged 2-17 years hospitalized for any reason at a single free-standing children’s hospital during 2017-2019. Children were categorized as having or not having obesity based on measured height/weight using Centers for Disease Control and Prevention definitions. The occurrence of 23 validated GAPPS triggers within the electronic health record were recorded for each encounter using an automated process. Proportions of encounters experiencing triggers were compared between weight categories using Chi square tests. Logistic regression was used to determine the odds of experiencing any AE trigger by weight category, adjusted for demographic and clinical characteristics.
Results: A total of 33,261 encounters were included, 15.5% of which were patients with obesity (Table 1). Occurrence of AE triggers ranged from very rare events (e.g., flumazenil administration, 4 occurrences during study period) to common events (e.g., 30-day readmission rates, 4,513 occurrences). Trigger rates varied by weight category for only 2 triggers examined, both occurring less frequently in children with obesity: oral vancomycin ordered (p=0.006), and inpatient death (p=0.010) (Table 2). Children with obesity had no increased odds of experiencing any category of AE trigger compared to children without obesity (Table 3).Conclusion(s): Hospitalized children with obesity experienced similar rates of AE triggers to those without obesity, indicating they may not be at higher risk of true AEs for the included triggers. However, this study did not assess actual AE rates, and did not include triggers requiring manual chart review or those specific to children with obesity (e.g., drug dosing errors). Future work should focus on identification of true AEs and triggers specifically tailored for children with obesity to elucidate how obesity modulates AE rates in hospitalized children.
Table 1. Cohort demographic and clinical characteristics by weight category
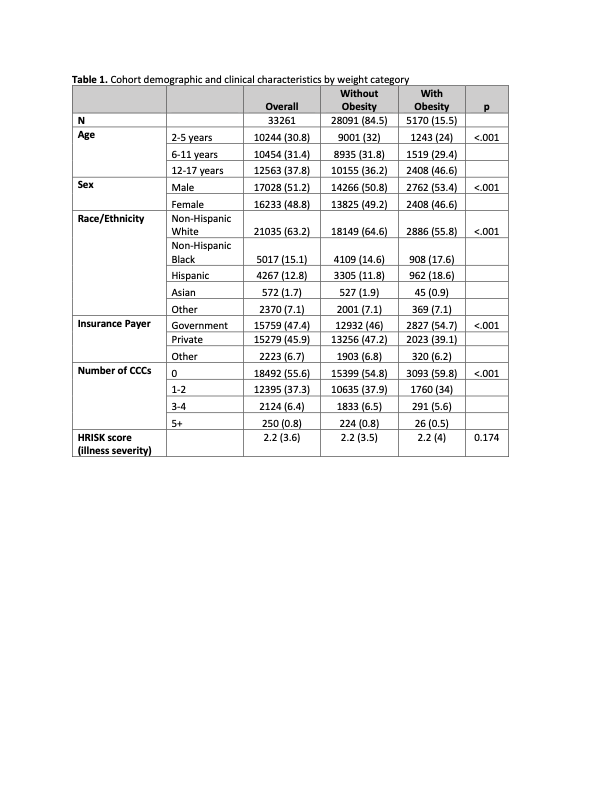
Table 2. Adverse event trigger event rates by weight category