Back
Developmental and Behavioral Pediatrics: Other
Category: Abstract Submission
Developmental and Behavioral Pediatrics: Equity
64 - Mental Health and Adverse Childhood Experiences of Siblings of Children with Special Healthcare Needs
Saturday, April 23, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 64
Publication Number: 64.202
Publication Number: 64.202
Claudia Hatef, Cohen Children's Medical Center, Waverly, NY, United States; Duy Q. Pham, Cohen Children's Medical Center, New York, NY, United States; Allison Lin, Cohen Children's Medical Center, Port Washington, NY, United States; Hannah E. Rosenthal, Cohen Children's Medical Center, Hauppauge, NY, United States; Ruth Milanaik, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Great Neck, NY, United States
Allison Lin, BS
Visiting Scholar
Cohen Children's Medical Center
Port Washington, New York, United States
Presenting Author(s)
Background: Non-disabled siblings of children with special healthcare needs (CSHCN) may encounter particularly challenging experiences and responsibilities that can put them at increased risk for psychological issues. Having a child with an intellectual/developmental disability has also been associated with increased parental stress and depression, which could impact the relationship with their non-disabled children. While some studies indicate that siblings of children with disabilities are more likely to have increased psychological distress and reduced psychosocial functioning, research into outcomes of siblings of CSHCN have shown variable results.
Objective: To assess the likelihood of anxiety and depression, ACEs, and family relationship indicators among siblings of CSHCN.
Design/Methods: This study examines a total eligible sample of 51,469 children from a combined 2016-2019 National Survey of Children’s Health dataset. Linear and logistic regression are used to compute relevant odds ratios (OR), adjusted odds ratios (aOR), and 95% confidence intervals (95% CI) to model the outcomes of interest as a function of the sibling designation. Sociodemographic confounders including the child’s age, sex, race/ethnicity, highest level of adult education, insurance status, medical home status, and parent’s mental health status are adjusted for in the models.
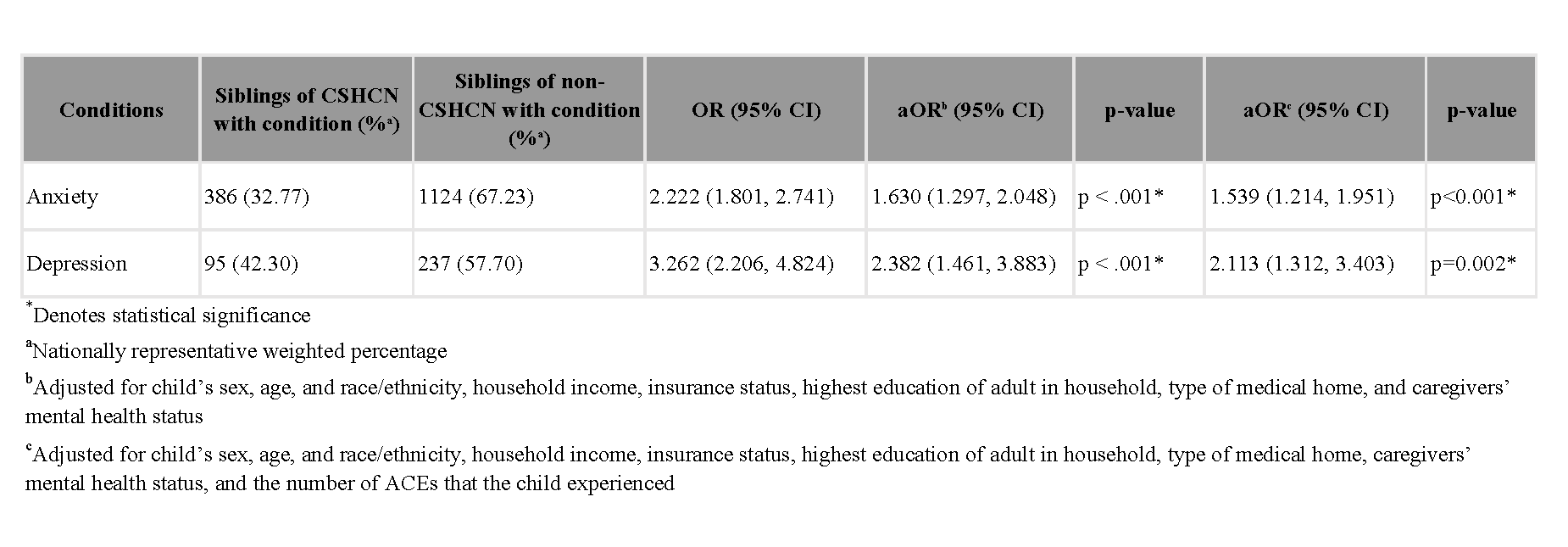
Results: Siblings of CSHCN have a higher likelihood of having various ACEs (Table 1). Most notably, siblings of CSHCN are more likely to live with someone who was mentally ill, suicidal, or severely depressed (aOR=3.433, 95% CI 2.019, 2.932), and to be a victim or witness of neighborhood violence (aOR=2.259, 95% CI: 1.61, 3.170). They are also more likely to experience anxiety and depression (aOR=1.630, 95% CI: 1.297, 2.048; aOR=2.382, 95% CI: 1.461, 3.883, respectively), even after controlling for exposures to ACEs (Table 2). Lastly, the parents indicated that there was no significant change in family resilience (βadj=-0.05, 95% CI: [-0.16,0.06]) while there was a slight increase in parental aggravation (βadj=0.12, 95% CI: [.02, .22]).Conclusion(s): Siblings of CSHCN are at an elevated risk of having mental health conditions and experiencing ACEs. As a result, pediatricians should dedicate additional attention to this unique population to ensure that appropriate support is given. Siblings of CSHCN should be provided with regular evaluations to screen for potential mental health issues, allowing for timely interventions such as therapy, counseling, and support services.
Table 1. Association between Siblings of CSHCN and Adverse Childhood Experiences, 2016-2019 National Survey of Children’s Health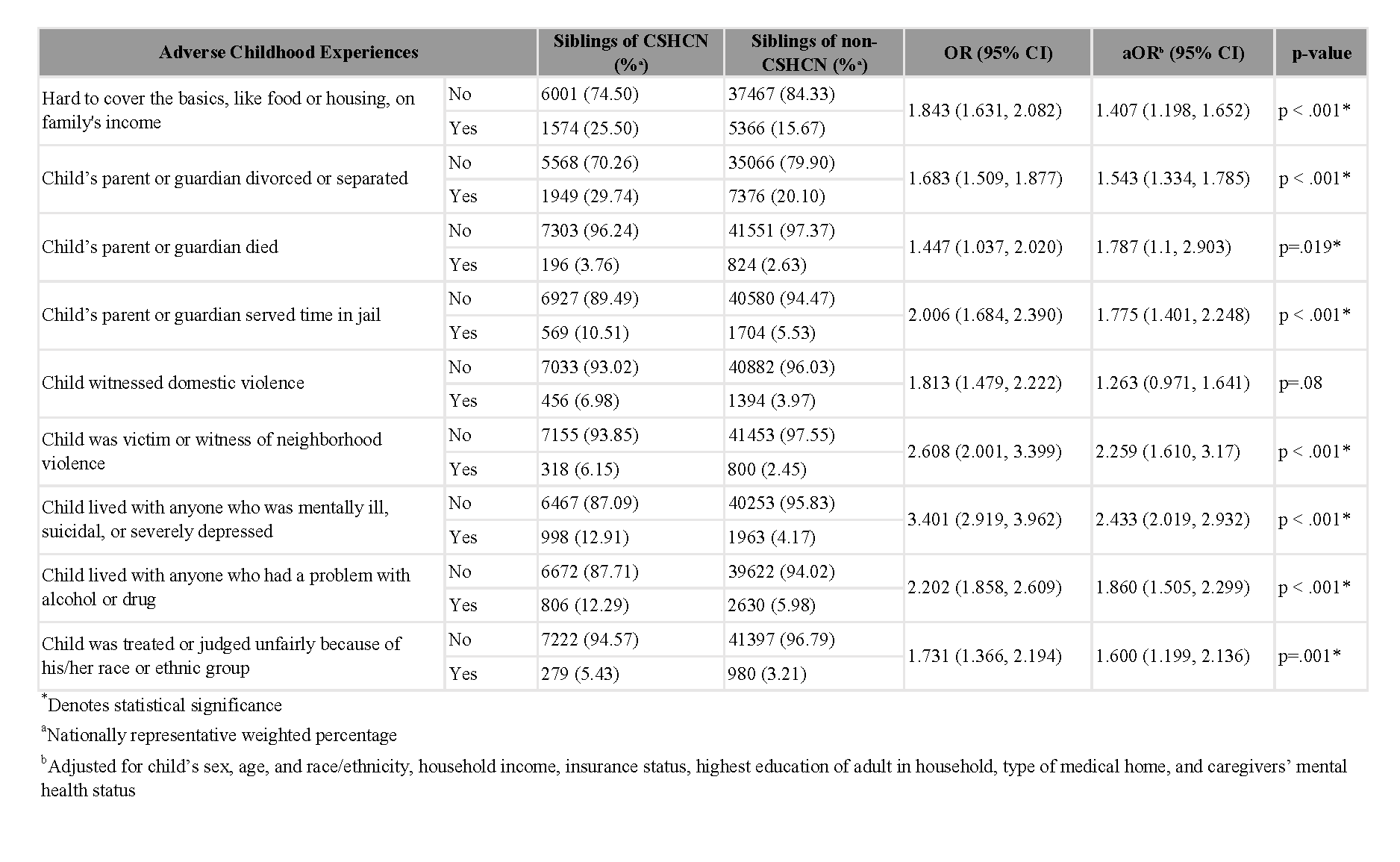
Table 2. Association between Siblings of CSHCN and Mental Health Conditions, 2016-2019 National Survey of Children’s Health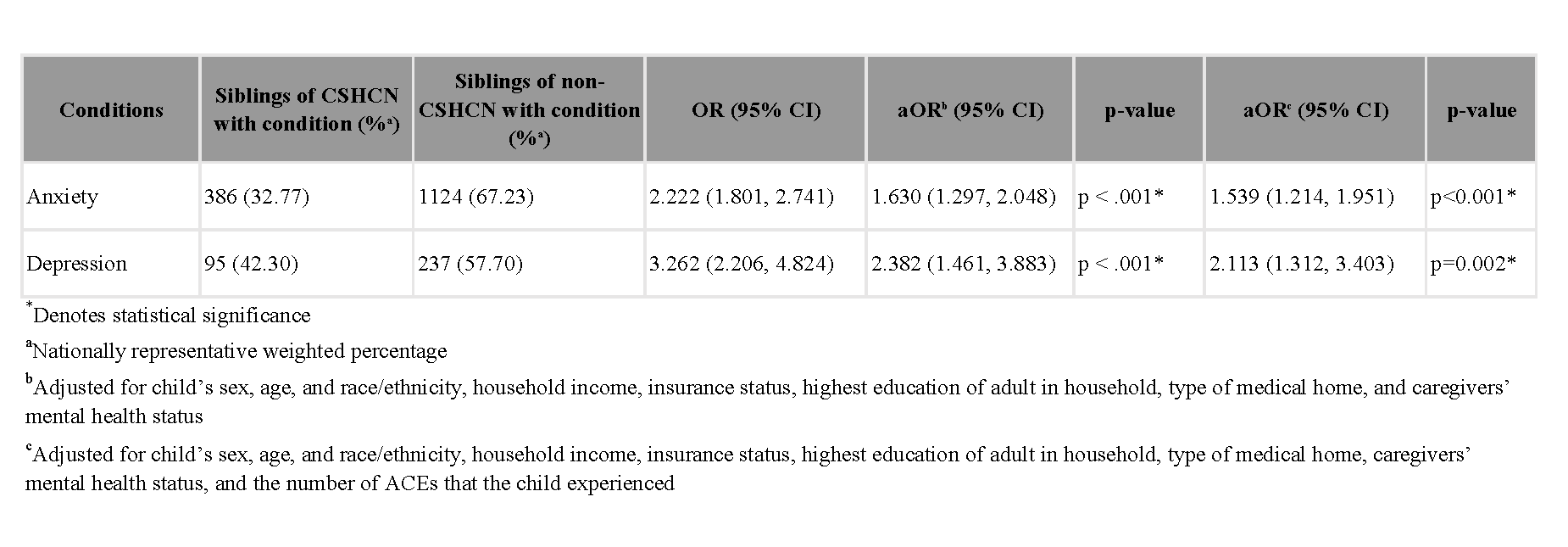
Objective: To assess the likelihood of anxiety and depression, ACEs, and family relationship indicators among siblings of CSHCN.
Design/Methods: This study examines a total eligible sample of 51,469 children from a combined 2016-2019 National Survey of Children’s Health dataset. Linear and logistic regression are used to compute relevant odds ratios (OR), adjusted odds ratios (aOR), and 95% confidence intervals (95% CI) to model the outcomes of interest as a function of the sibling designation. Sociodemographic confounders including the child’s age, sex, race/ethnicity, highest level of adult education, insurance status, medical home status, and parent’s mental health status are adjusted for in the models.
Results: Siblings of CSHCN have a higher likelihood of having various ACEs (Table 1). Most notably, siblings of CSHCN are more likely to live with someone who was mentally ill, suicidal, or severely depressed (aOR=3.433, 95% CI 2.019, 2.932), and to be a victim or witness of neighborhood violence (aOR=2.259, 95% CI: 1.61, 3.170). They are also more likely to experience anxiety and depression (aOR=1.630, 95% CI: 1.297, 2.048; aOR=2.382, 95% CI: 1.461, 3.883, respectively), even after controlling for exposures to ACEs (Table 2). Lastly, the parents indicated that there was no significant change in family resilience (βadj=-0.05, 95% CI: [-0.16,0.06]) while there was a slight increase in parental aggravation (βadj=0.12, 95% CI: [.02, .22]).Conclusion(s): Siblings of CSHCN are at an elevated risk of having mental health conditions and experiencing ACEs. As a result, pediatricians should dedicate additional attention to this unique population to ensure that appropriate support is given. Siblings of CSHCN should be provided with regular evaluations to screen for potential mental health issues, allowing for timely interventions such as therapy, counseling, and support services.
Table 1. Association between Siblings of CSHCN and Adverse Childhood Experiences, 2016-2019 National Survey of Children’s Health
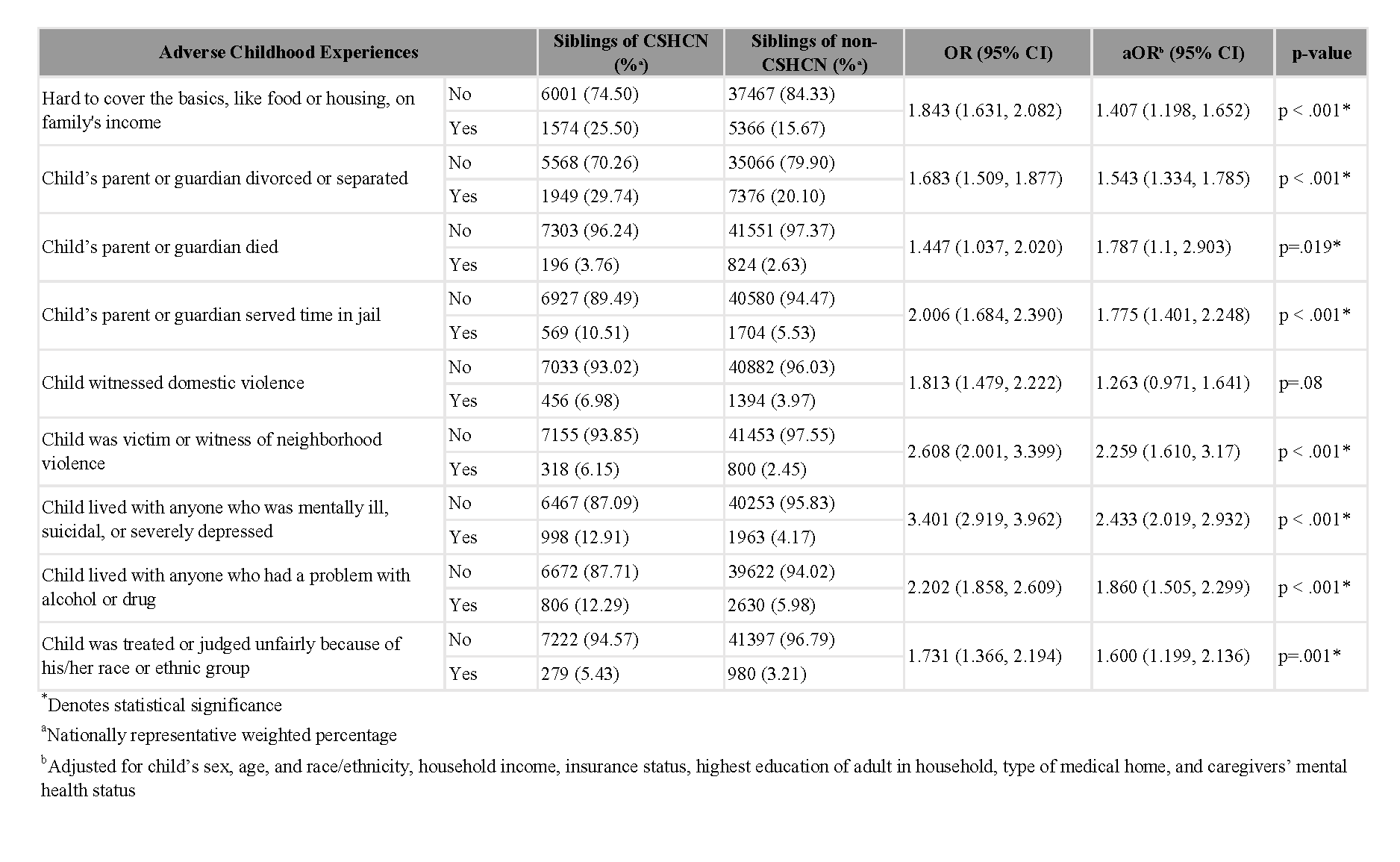
Table 2. Association between Siblings of CSHCN and Mental Health Conditions, 2016-2019 National Survey of Children’s Health