General Pediatrics: All Areas
Category: Abstract Submission
General Pediatrics I
592 - Factors Associated with Increased Clinician Reported Resource Use in Pediatrics
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 592
Publication Number: 592.208
Publication Number: 592.208
Nidhya Navanandan, University of Colorado School of Medicine, Aurora, CO, United States; Monica C. McNulty, University of Colorado School of Medicine, Aurora, CO, United States; Krithika Suresh, Colorado School of Public Health, Denver, CO, United States; Julia Freeman, University of Colorado School of Medicine, Children’s Hospital Colorado, Aurora, CO, United States; Amy Tyler, University of Colorado School of Medicine, Aurora, CO, United States

Nidhya Navanandan, MD, MSCS (she/her/hers)
Associate Professor of Pediatrics
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: High resource use is common in pediatric medicine and impacts patient outcomes and healthcare costs. In adult studies, diagnostic uncertainty has been associated with high resource use. Few studies have evaluated the impact of clinician uncertainty on diagnostic test and treatment use in the pediatric setting.
Objective: To determine predictors of resource use among pediatric providers for common respiratory illnesses.
Design/Methods: We surveyed pediatric primary care, emergency department (ED)/urgent care (UC), and hospital medicine providers at a free-standing children’s hospital system. Physicians (MD/DO) and advanced practice providers (APPs) were included; trainees were excluded. Five clinical vignettes were used to assess provider self-reported resource use. A total vignette score, computed as the sum of the numeric Likert scale responses to all vignette questions, was created (range of 16 to 80) with a higher score indicating higher resource use. The Physician Reaction to Uncertainty (PRU) scale and Medical Maximizer-Minimizer Scale (MMS) were used to assess tolerance to uncertainty and medical decision-making behaviors. Multivariate regression was performed to identify provider-level factors (provider-type, location of practice, tolerance to uncertainty, and medical decision-making behaviors) associated with high resource use as measured by the total vignette score.
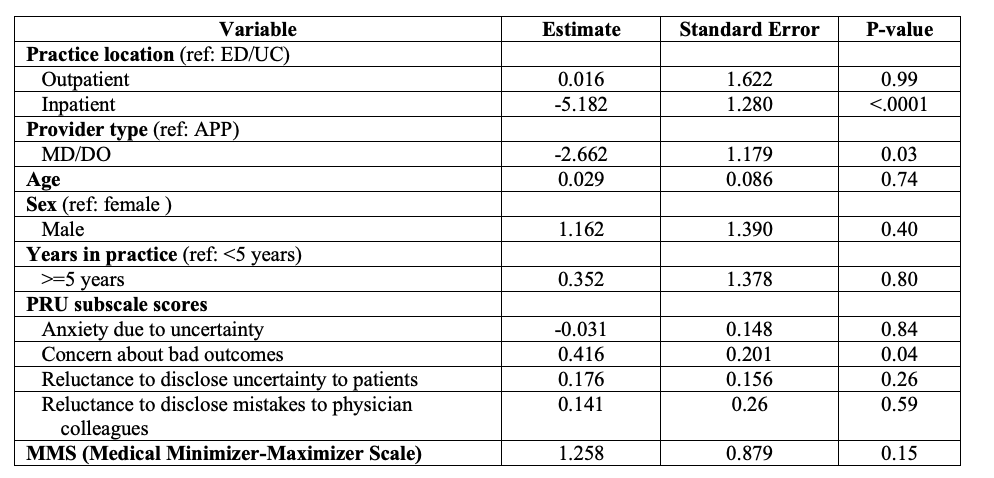
Results: The response rate was 75% (168/223). Most survey respondents were female (79%), physicians (65%), non-Hispanic (94%) and had ≥ 5 years of experience since completion of training (71%). ED/UC and primary care providers had higher vignette scores, indicating higher resource use, compared to inpatient providers; APPs had higher vignette scores compared to physicians. There were no statistically significant differences in PRU or MMS scores by location of practice. However, APPs had higher “anxiety due to uncertainty” and “reluctance to disclose uncertainty to patient” scores compared to physicians (Table 1). In multivariate analysis, being an ED/UC provider or an APP, and having greater concern for bad outcomes were associated with higher vignette scores (Table 2).Conclusion(s): Provider type and location of practice predict resource use for children with common respiratory illnesses. Interventions targeted at test-maximizing providers may improve quality of care and reduce resource burden and costs.
Table 1. Physician uncertainty measures by provider type and location of practice.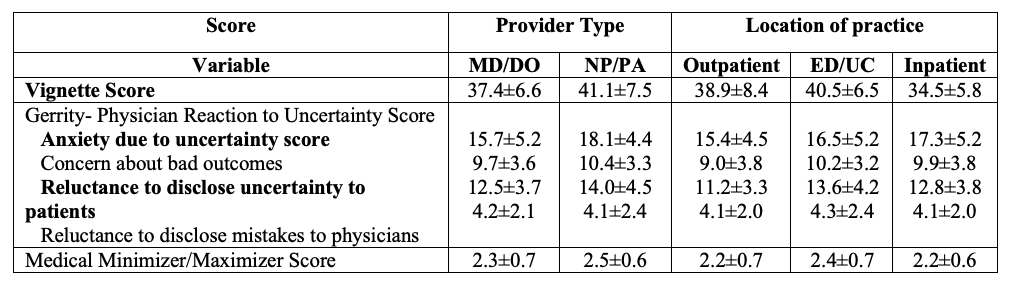 *Results presented as mean score ± standard deviation.
*Results presented as mean score ± standard deviation.
Table 2. Multivariable regression model for provider-level of resource use as measured by vignette scores.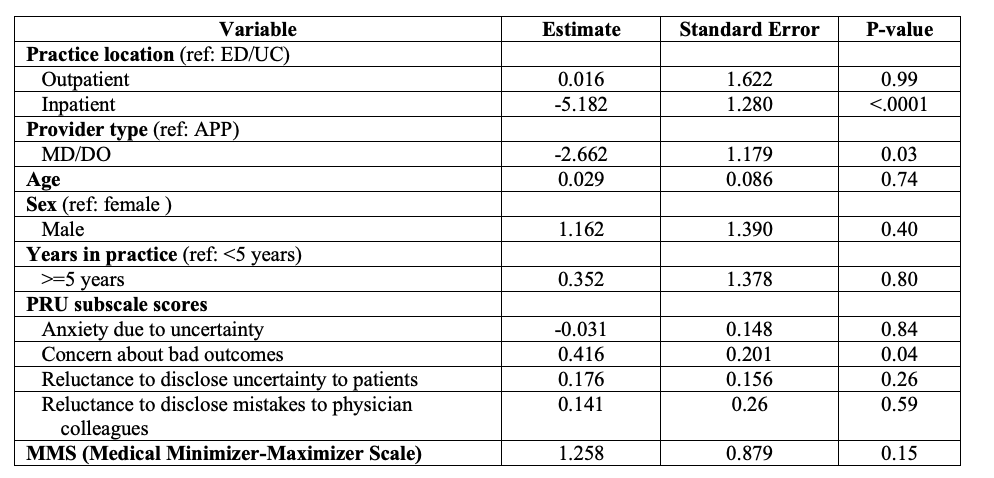
Objective: To determine predictors of resource use among pediatric providers for common respiratory illnesses.
Design/Methods: We surveyed pediatric primary care, emergency department (ED)/urgent care (UC), and hospital medicine providers at a free-standing children’s hospital system. Physicians (MD/DO) and advanced practice providers (APPs) were included; trainees were excluded. Five clinical vignettes were used to assess provider self-reported resource use. A total vignette score, computed as the sum of the numeric Likert scale responses to all vignette questions, was created (range of 16 to 80) with a higher score indicating higher resource use. The Physician Reaction to Uncertainty (PRU) scale and Medical Maximizer-Minimizer Scale (MMS) were used to assess tolerance to uncertainty and medical decision-making behaviors. Multivariate regression was performed to identify provider-level factors (provider-type, location of practice, tolerance to uncertainty, and medical decision-making behaviors) associated with high resource use as measured by the total vignette score.
Results: The response rate was 75% (168/223). Most survey respondents were female (79%), physicians (65%), non-Hispanic (94%) and had ≥ 5 years of experience since completion of training (71%). ED/UC and primary care providers had higher vignette scores, indicating higher resource use, compared to inpatient providers; APPs had higher vignette scores compared to physicians. There were no statistically significant differences in PRU or MMS scores by location of practice. However, APPs had higher “anxiety due to uncertainty” and “reluctance to disclose uncertainty to patient” scores compared to physicians (Table 1). In multivariate analysis, being an ED/UC provider or an APP, and having greater concern for bad outcomes were associated with higher vignette scores (Table 2).Conclusion(s): Provider type and location of practice predict resource use for children with common respiratory illnesses. Interventions targeted at test-maximizing providers may improve quality of care and reduce resource burden and costs.
Table 1. Physician uncertainty measures by provider type and location of practice.
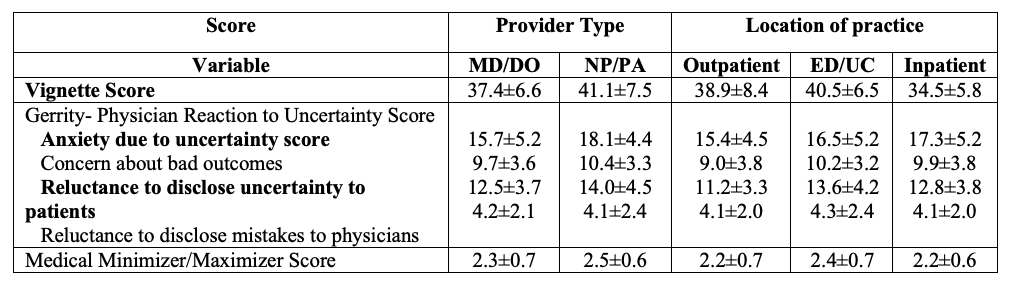 *Results presented as mean score ± standard deviation.
*Results presented as mean score ± standard deviation.Table 2. Multivariable regression model for provider-level of resource use as measured by vignette scores.