Neonatal Infectious Diseases/Immunology
Category: Abstract Submission
Neonatal Infectious Diseases/Immunology: COVID-19
283 - Factors influencing SARS-CoV-2 transplacental transmission
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 283
Daniele M. De Luca, Paris Saclay University - "A.Beclere" Hospital, Clamart (Paris), Ile-de-France, France; Sophie prevot, Université Paris Saclay APHP, Le Kremlin Bicetre, Ile-de-France, France; Christelle Vauloup-Fellous, Universite paris saclay, Villejuif, Ile-de-France, France; Alexandra Benachi, Antoine Beclere Hospital, Clamart, Ile-de-France, France; Alexandre J. Vivanti, Paris Saclay University, Clamart, Ile-de-France, France

Daniele De Luca, MD, PhD (he/him/his)
Full Professor
APHP-Paris Saclay University
Paris, Ile-de-France, France
Presenting Author(s)
Background: SARS-CoV-2 transplacental transmission is a rare event that can lead to relevant negative consequences for the offspring. The factors influencing transplacental transmission are unclear: we designed a study to verify whether placental expression of viral receptors, viral load, inflammation, or some clinical features influence SARS-CoV-2 transplacental transmission.
Objective: To clarify if one of the aforementioned factors influence SARS-CoV-2 transplacental transmission.
Design/Methods: The project was divided in two phases: 1) a case study of women affected by COVID-19 during the third trimester and their neonates if they experienced transplacental transmission of SARS-CoV-2; 2) a translational study analysing data and placental samples from various groups of pregnant women for factors possibly affecting transplacental transmission. We enrolled women diagnosed with COVID-19 during the third trimester, with (C+P+ group, n=10) or without (C+P- group, n=10) positive RT-PCR on placental tissue, and pregnant women without SARS-CoV-2 infection (Control group, n=11). Six cases of SARS-CoV-2 transplacental transmission were included in the C+P+ group. Investigators blinded to clinical data performed protein assay, ELISA for ACE2 and TMPRSS2 receptors, viral load estimation and Sanger sequencing, pathology examination with immunohistochemistry on placental specimens. Clinical data were real time collected
Results: Transplacental transmission of SARS-CoV-2 is not related to the placental expression of ACE2 (p=0.335) and TMPRSS2 (p=0.163) receptors or viral load (p=0.153) or any common clinical perinatal characteristics. Transplacental transmission was associated with placental inflammation, and particularly with intervillositis with peculiar pathological signature (massive fibrin deposition, diffuse chronic intervillositis with necrosis and positive viral staining in the intervillositis lesions - see Figure), which may damage the placental barrier and is associated with foetal distress (p=0.002), acidosis at the birth (p=0.038) and need for neonatal intensive care (p=0.008 - see Table).Conclusion(s): Transplacental SARS-CoV-2 transmission is associated with placental inflammation and seems to occur when the placental damage is sufficient to determine foetal distress and acidosis at the birth needing neonatal critical care.
Figure. Translational study: illustrative images of placentas infected by SARS-CoV-2 (C+P+ group) with or without SARS-CoV-2 transplacental transmission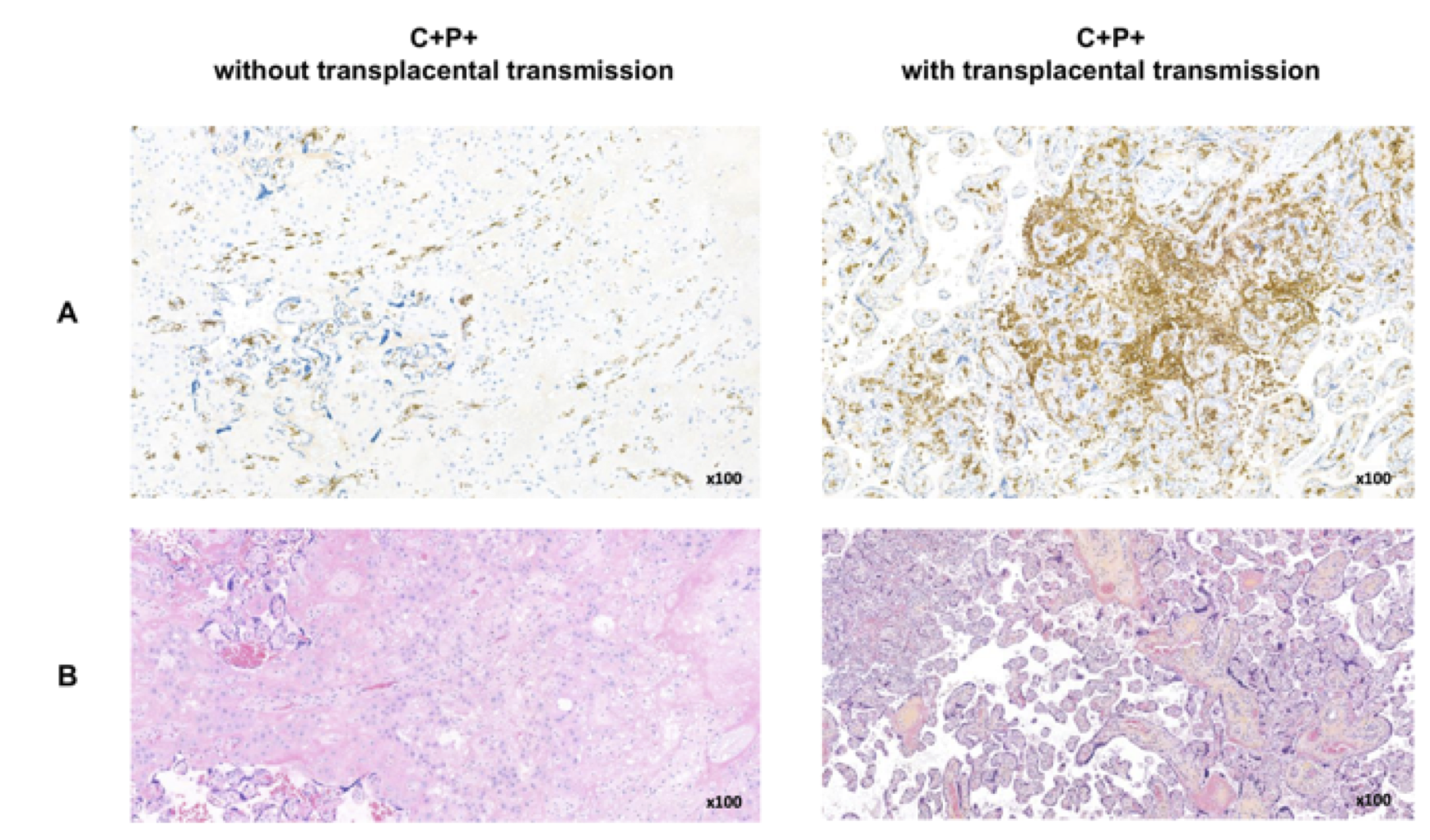 Images from a pregnancy without (left) or with transplacental transmission (right) are shown. Panels A and B depict CD163 immunostaining and HES stain, respectively. Infected placenta with transplacental transmission shows a higher degree of chronic intervillositis as seen in HES stain with macrophage infiltration as demonstrated by CD163 immunostaining.
Images from a pregnancy without (left) or with transplacental transmission (right) are shown. Panels A and B depict CD163 immunostaining and HES stain, respectively. Infected placenta with transplacental transmission shows a higher degree of chronic intervillositis as seen in HES stain with macrophage infiltration as demonstrated by CD163 immunostaining.
Case study of transplacental transmissions: perinatal outcomes of pregnancies complicated by COVID-19 during the third trimester with or without SARS-CoV-2 transplacental transmission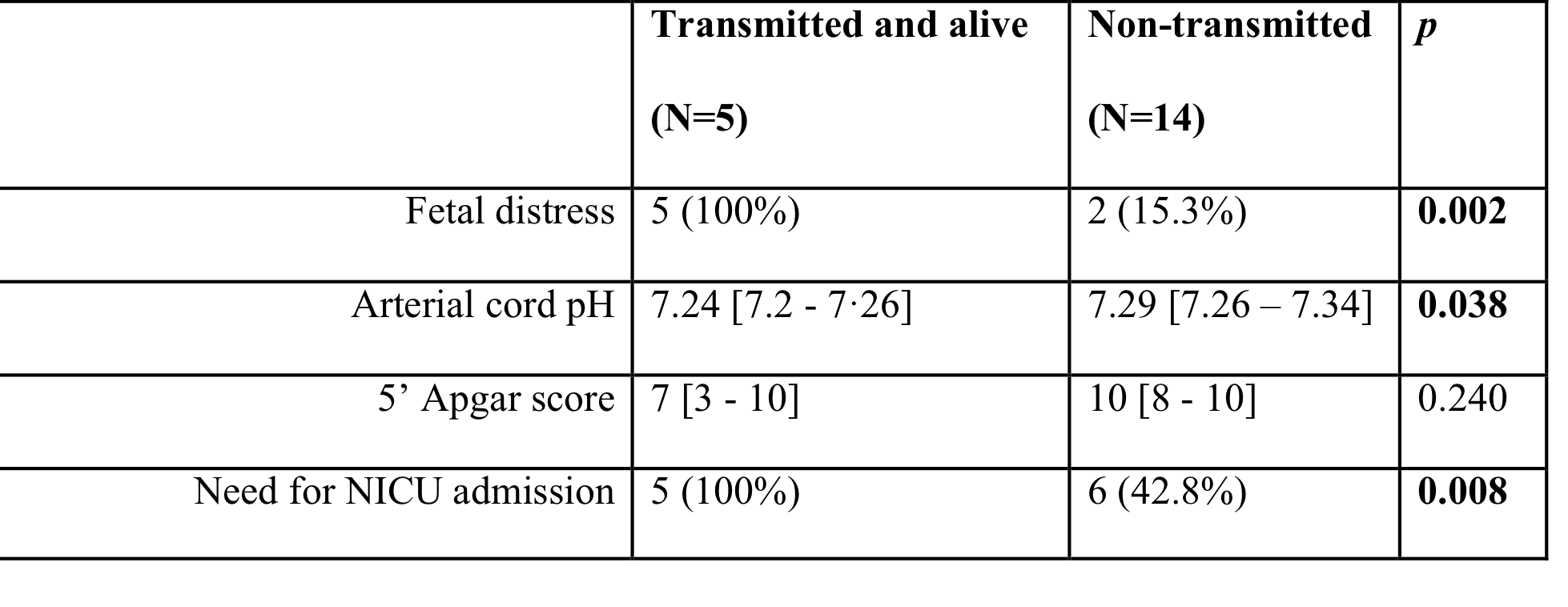 Live neonates with transplacentally transmitted SARS-CoV-2 infection were compared to 14 neonates born from women with COVID-19 during the third trimester. Data are expressed as median [25th – 75th percentile] or number (%). Abbreviations: NICU: neonatal intensive care unit.
Live neonates with transplacentally transmitted SARS-CoV-2 infection were compared to 14 neonates born from women with COVID-19 during the third trimester. Data are expressed as median [25th – 75th percentile] or number (%). Abbreviations: NICU: neonatal intensive care unit.
Objective: To clarify if one of the aforementioned factors influence SARS-CoV-2 transplacental transmission.
Design/Methods: The project was divided in two phases: 1) a case study of women affected by COVID-19 during the third trimester and their neonates if they experienced transplacental transmission of SARS-CoV-2; 2) a translational study analysing data and placental samples from various groups of pregnant women for factors possibly affecting transplacental transmission. We enrolled women diagnosed with COVID-19 during the third trimester, with (C+P+ group, n=10) or without (C+P- group, n=10) positive RT-PCR on placental tissue, and pregnant women without SARS-CoV-2 infection (Control group, n=11). Six cases of SARS-CoV-2 transplacental transmission were included in the C+P+ group. Investigators blinded to clinical data performed protein assay, ELISA for ACE2 and TMPRSS2 receptors, viral load estimation and Sanger sequencing, pathology examination with immunohistochemistry on placental specimens. Clinical data were real time collected
Results: Transplacental transmission of SARS-CoV-2 is not related to the placental expression of ACE2 (p=0.335) and TMPRSS2 (p=0.163) receptors or viral load (p=0.153) or any common clinical perinatal characteristics. Transplacental transmission was associated with placental inflammation, and particularly with intervillositis with peculiar pathological signature (massive fibrin deposition, diffuse chronic intervillositis with necrosis and positive viral staining in the intervillositis lesions - see Figure), which may damage the placental barrier and is associated with foetal distress (p=0.002), acidosis at the birth (p=0.038) and need for neonatal intensive care (p=0.008 - see Table).Conclusion(s): Transplacental SARS-CoV-2 transmission is associated with placental inflammation and seems to occur when the placental damage is sufficient to determine foetal distress and acidosis at the birth needing neonatal critical care.
Figure. Translational study: illustrative images of placentas infected by SARS-CoV-2 (C+P+ group) with or without SARS-CoV-2 transplacental transmission
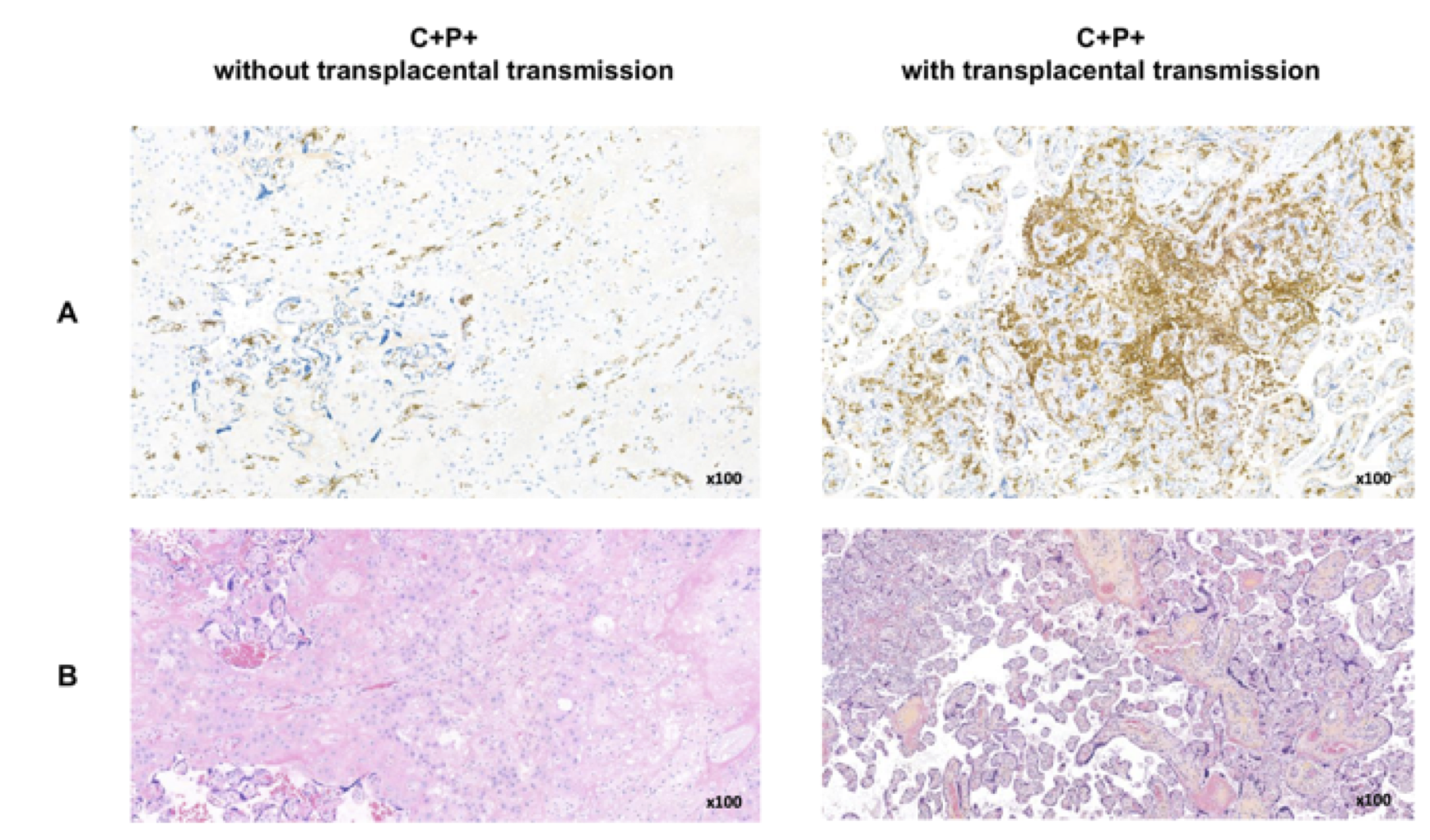 Images from a pregnancy without (left) or with transplacental transmission (right) are shown. Panels A and B depict CD163 immunostaining and HES stain, respectively. Infected placenta with transplacental transmission shows a higher degree of chronic intervillositis as seen in HES stain with macrophage infiltration as demonstrated by CD163 immunostaining.
Images from a pregnancy without (left) or with transplacental transmission (right) are shown. Panels A and B depict CD163 immunostaining and HES stain, respectively. Infected placenta with transplacental transmission shows a higher degree of chronic intervillositis as seen in HES stain with macrophage infiltration as demonstrated by CD163 immunostaining.Case study of transplacental transmissions: perinatal outcomes of pregnancies complicated by COVID-19 during the third trimester with or without SARS-CoV-2 transplacental transmission
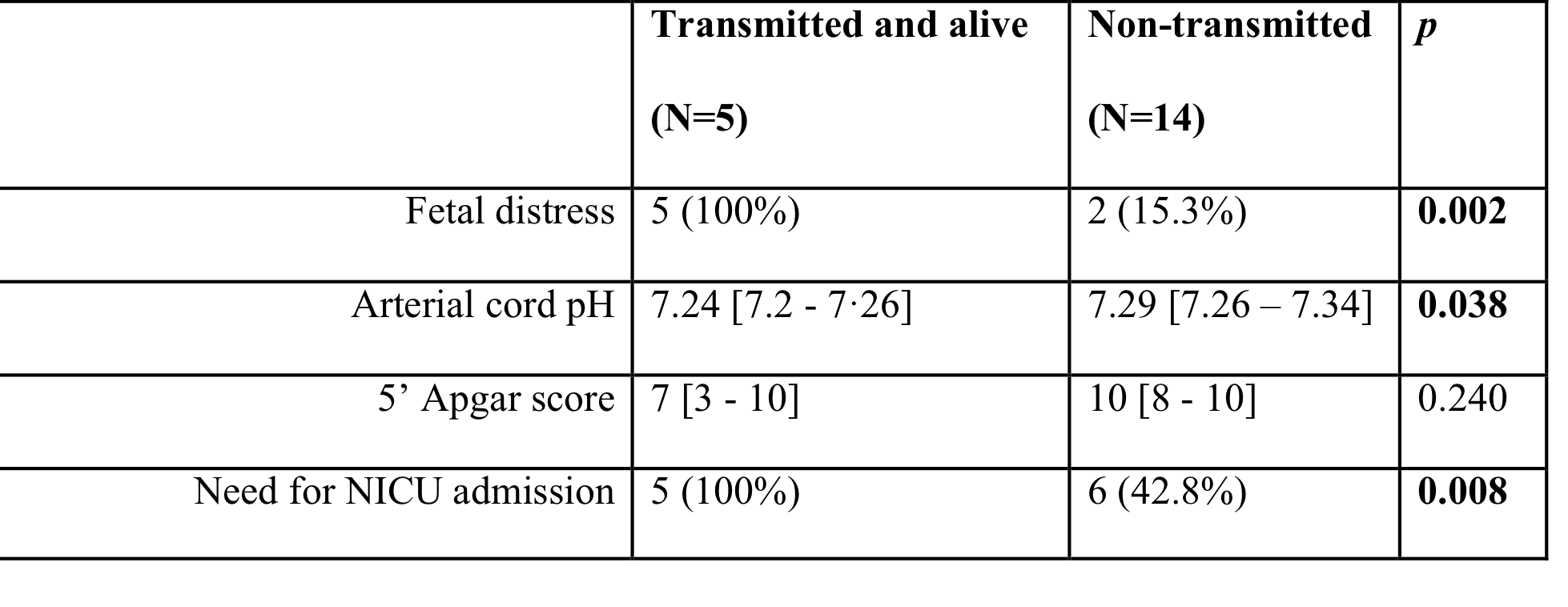 Live neonates with transplacentally transmitted SARS-CoV-2 infection were compared to 14 neonates born from women with COVID-19 during the third trimester. Data are expressed as median [25th – 75th percentile] or number (%). Abbreviations: NICU: neonatal intensive care unit.
Live neonates with transplacentally transmitted SARS-CoV-2 infection were compared to 14 neonates born from women with COVID-19 during the third trimester. Data are expressed as median [25th – 75th percentile] or number (%). Abbreviations: NICU: neonatal intensive care unit.