Cardiology
Category: Abstract Submission
Cardiology I
162 - A Successful Home Nasogastric Tube Program for Children with Congenital Heart Disease
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 162
Publication Number: 162.101
Publication Number: 162.101
Divya Patel, Children's Hospital Los Angeles, Los Angeles, CA, United States; Maria Theresa Alquiros, Children’s Hospital Los Angeles, Pasadena, CA, United States; Stephanie Sanborn, Children's Hospital Los Angeles, Los Angeles, CA, United States; Nhu Tran, Children's Hospital Los Angeles/USC, Los Angeles, CA, United States; Cynthia S. Herrington, Children's Hospital Los Angeles, Los angels, CA, United States; Jodie K. Votava-Smith, Children's Hopsital Los Angeles, Los Angeles, CA, United States
.jpg)
Divya Patel, MD
Pediatric Resident
Children's Hospital Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background: Feeding dysfunction is common in infants with congenital heart disease (CHD) and often prolongs hospital stay. We initiated a program to allow infants with CHD to be discharged home with nasogastric tube (NGT) feeds and close outpatient monitoring by a dedicated nurse and dietitian.
Objective: We aimed to assess the safety of home NGT and identify factors associated with successful wean to full oral intake (PO) as an outpatient.
Design/Methods: This is a prospective cohort study of infants with CHD requiring surgical palliation or repair in the home NGT program at Children’s Hospital Los Angeles from 10/1/17 to 12/1/21. Demographics, CHD type, PO % at discharge, and complications requiring emergency (ED) visit or re-admission were evaluated. Outcome data included full PO by study end and home NGT duration. Pearson Chi-square or ANOVA were used to examine characteristics of those who achieved full PO, and multivariate logistic regression explored relationships between clinical factors and successful wean off tube feeds.
Results: Of 61 CHD patients followed for home NGT, 2 died unrelated to NGT. Of 59 remaining, 56% were female, 76% full term. A majority had cyanotic CHD (58%) and 27% had single ventricle CHD. Cardiac intervention prior to home NGT included 42% with palliative and 41% with complete surgical repair; 17% had unrepaired CHD. At study end, 68% achieved full PO feeds. Median duration of home NGT was 78 days (IQR 30,153). Complications were infrequent: 9 ED visits for 7 patients & 3 feeding readmissions (17% of patients). There were no aspiration or other critical events. Factors associated with successful wean off NGT included percent PO at time of discharge, with a 4% increase in the odds of successful wean off tube feeds with every 1% increase in PO, corrected for prematurity (p=0.009). Infant sex, prematurity, and single ventricle or cyanotic CHD subtype did not predict full PO. Infants who achieved full PO were more likely to have unrepaired or fully repaired CHD than palliated CHD (p=0.002, 0.035). 100% of the infants with unrepaired CHD achieved full PO feeds.Conclusion(s): Home NGT is a safe option for infants with complex CHD to optimize nutrition and shorten hospital stay. Successful advancement to full PO was achieved in most patients, predicted by higher percentage oral intake at initiation of home NGT. Infants with unrepaired and fully repaired CHD were more likely to achieve full PO than those with palliated CHD. Our program was successful with few NGT readmissions, no serious complications, and a novel nurse/dietitian led model.
Home NGT study cohort flow diagram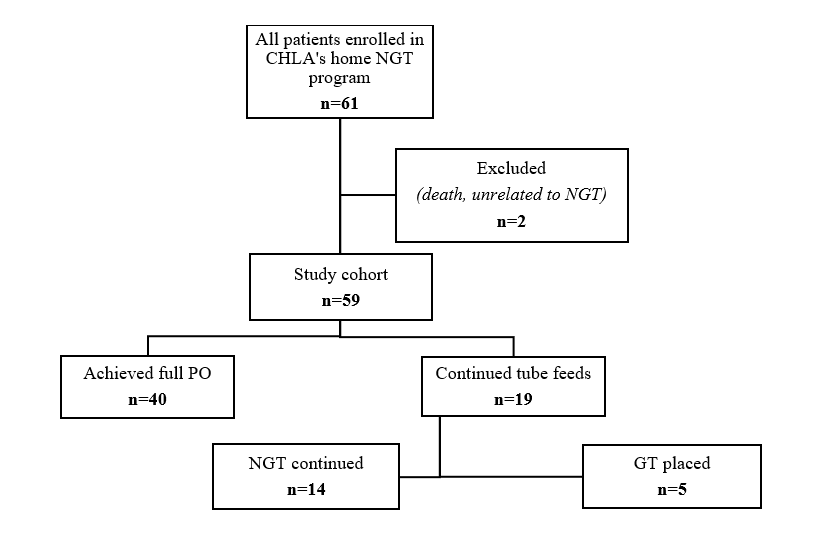
Patient characteristics by feeding status at end of study.png)
Objective: We aimed to assess the safety of home NGT and identify factors associated with successful wean to full oral intake (PO) as an outpatient.
Design/Methods: This is a prospective cohort study of infants with CHD requiring surgical palliation or repair in the home NGT program at Children’s Hospital Los Angeles from 10/1/17 to 12/1/21. Demographics, CHD type, PO % at discharge, and complications requiring emergency (ED) visit or re-admission were evaluated. Outcome data included full PO by study end and home NGT duration. Pearson Chi-square or ANOVA were used to examine characteristics of those who achieved full PO, and multivariate logistic regression explored relationships between clinical factors and successful wean off tube feeds.
Results: Of 61 CHD patients followed for home NGT, 2 died unrelated to NGT. Of 59 remaining, 56% were female, 76% full term. A majority had cyanotic CHD (58%) and 27% had single ventricle CHD. Cardiac intervention prior to home NGT included 42% with palliative and 41% with complete surgical repair; 17% had unrepaired CHD. At study end, 68% achieved full PO feeds. Median duration of home NGT was 78 days (IQR 30,153). Complications were infrequent: 9 ED visits for 7 patients & 3 feeding readmissions (17% of patients). There were no aspiration or other critical events. Factors associated with successful wean off NGT included percent PO at time of discharge, with a 4% increase in the odds of successful wean off tube feeds with every 1% increase in PO, corrected for prematurity (p=0.009). Infant sex, prematurity, and single ventricle or cyanotic CHD subtype did not predict full PO. Infants who achieved full PO were more likely to have unrepaired or fully repaired CHD than palliated CHD (p=0.002, 0.035). 100% of the infants with unrepaired CHD achieved full PO feeds.Conclusion(s): Home NGT is a safe option for infants with complex CHD to optimize nutrition and shorten hospital stay. Successful advancement to full PO was achieved in most patients, predicted by higher percentage oral intake at initiation of home NGT. Infants with unrepaired and fully repaired CHD were more likely to achieve full PO than those with palliated CHD. Our program was successful with few NGT readmissions, no serious complications, and a novel nurse/dietitian led model.
Home NGT study cohort flow diagram
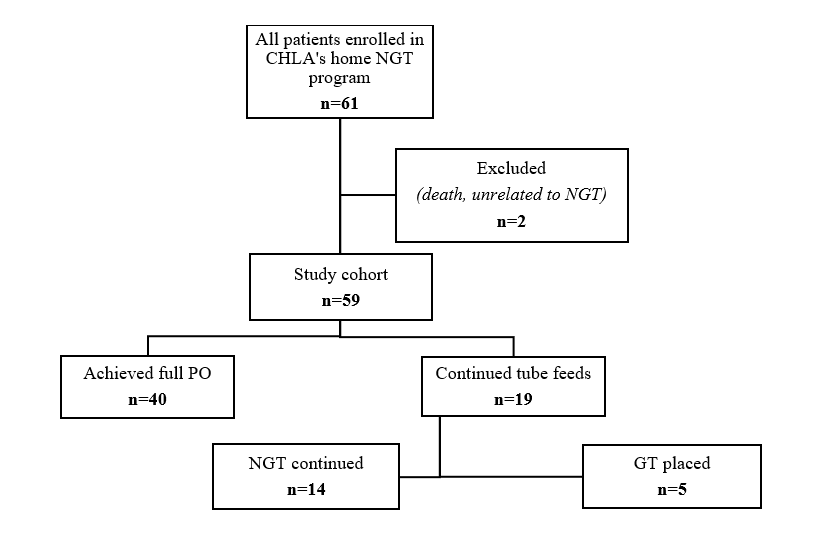
Patient characteristics by feeding status at end of study
.png)
