Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement I
204 - “My Brigham Baby” App: Using Technology to Advance Parent Engagement and Promote Resilience in the Neonatal Intensive Care Unit
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 204
Publication Number: 204.126
Publication Number: 204.126
Madison D. Forde, Brigham and Women's Hospital, Boston, MA, United States; Sara Cherkerzian, Brigham and Women's Hospital, Boston, MA, United States; Maria S. Conley, Brigham and Women's Hospital, Boston, MA, United States; Cindy H. Liu, Brigham and Women's Hospital, Boston, MA, United States; Terrie E. Inder, Harvard Medical School, Boston, MA, United States; Carmina Erdei, Brigham and Women's Hospital and Harvard Medical School, Boston, MA, United States
- MF
Madison D. Forde
Research Assistant
Brigham and Women's Hospital
Brigham and Women's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Parents of infants who require hospitalization in the Neonatal Intensive Care Unit (NICU) often experience psychosocial distress, impacting infant and family outcomes. Technology-based interventions may enhance parent experience, discharge readiness, and promote family-centered developmental care in the NICU. An interdisciplinary team has partnered to create a smartphone application (App), “My Brigham Baby”, to better support parents of infants admitted to a level III NICU.
Objective: The objective of this study was to describe the family psychosocial experience in the NICU and assess how it evolved after rollout of an educational App.
Design/Methods: Responses to questionnaires regarding parental NICU experience were obtained from parents (25 pre- and 25 post-App rollout). Post-App data collection occurred during the COVID-19 pandemic (Pre-app: Spring/Summer 2020, Post-App: Summer-Winter 2020/Spring 2021). Data included self-reported discharge readiness, symptoms of stress and anxiety, and parenting skill confidence.
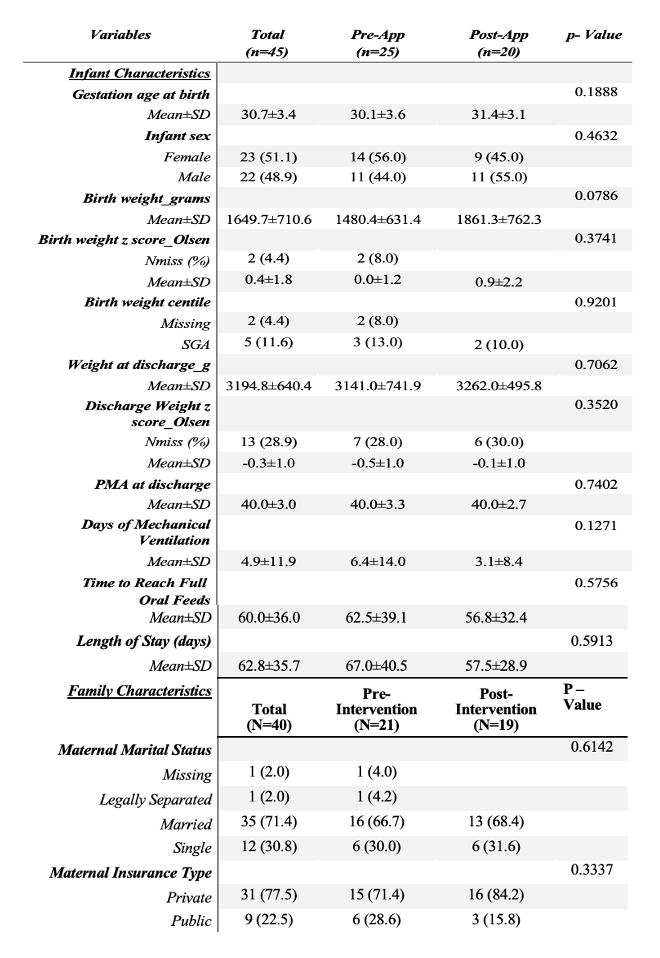
Descriptive statistics of the sample characteristics were evaluated by group status. Data was organized by family (n = 40), parent (n = 50 [n = 40 mothers and n = 10 fathers]), and infant (n = 45) levels. Differences in characteristics by rollout status were assessed using chi square or Wilcoxon rank sum tests.
Results: Demographic and clinical characteristics for pre- and post-App rollout groups indicated that there were no significant differences between group; both cohorts were comparable in terms of medical and family-social characteristics. Of the measured outcomes, frequency of “very ready” discharge readiness responses significantly increased in the post-App rollout group (56% v. 20%, p =0.02*) (Table 1). There were no statistically significant differences between continuous scores of parent stress, anxiety symptoms, and parenting skills between the pre- and post-App cohorts (Table 1). When scores for each outcome were categorized by severity, pre-App rollout parent experience data suggested that many of surveyed parents felt ill-prepared for discharge (36%), reported severe symptoms of stress (28%) and anxiety (40%), and were not confident in their parenting skills (8%). Post-App survey results indicated that a more parents reported optimal experiences of discharge readiness (56%), anxiety symptoms (44%), and parenting skills (25%) (Figure 1 and Table 1).Conclusion(s): Technology applications can improve maternal NICU experiences particularly during the COVID-19 pandemic.
Figure 1: Distribution of Survey Scores Among n = 50 parents by pre- and post- App rollout status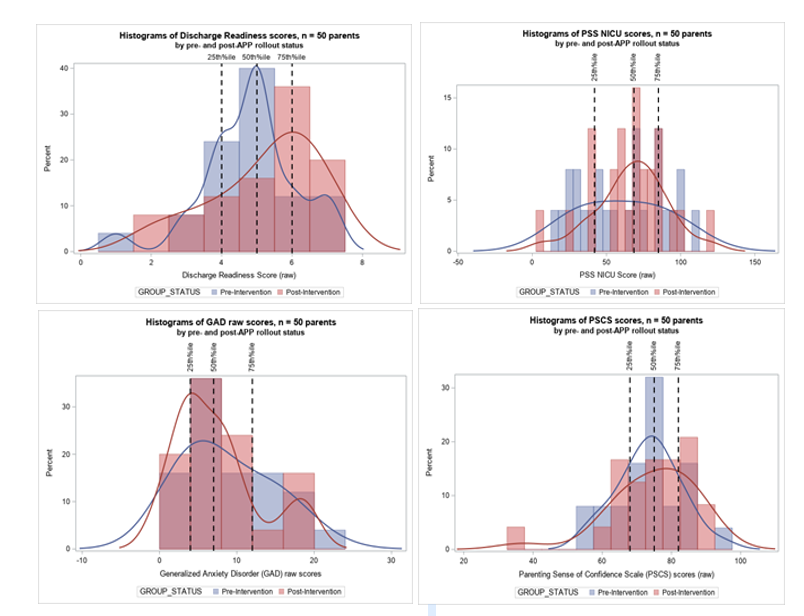
Table 1: Clinical and Demographic Characteristics for Pre- and Post-Intervention Cohorts of Infants and Parents. (n=50)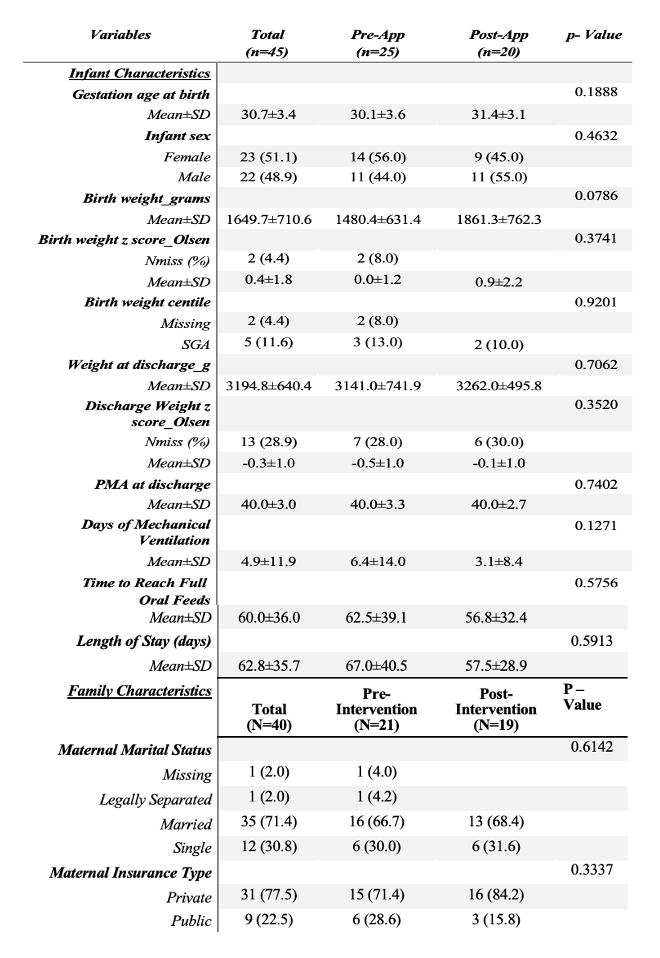
Objective: The objective of this study was to describe the family psychosocial experience in the NICU and assess how it evolved after rollout of an educational App.
Design/Methods: Responses to questionnaires regarding parental NICU experience were obtained from parents (25 pre- and 25 post-App rollout). Post-App data collection occurred during the COVID-19 pandemic (Pre-app: Spring/Summer 2020, Post-App: Summer-Winter 2020/Spring 2021). Data included self-reported discharge readiness, symptoms of stress and anxiety, and parenting skill confidence.
Descriptive statistics of the sample characteristics were evaluated by group status. Data was organized by family (n = 40), parent (n = 50 [n = 40 mothers and n = 10 fathers]), and infant (n = 45) levels. Differences in characteristics by rollout status were assessed using chi square or Wilcoxon rank sum tests.
Results: Demographic and clinical characteristics for pre- and post-App rollout groups indicated that there were no significant differences between group; both cohorts were comparable in terms of medical and family-social characteristics. Of the measured outcomes, frequency of “very ready” discharge readiness responses significantly increased in the post-App rollout group (56% v. 20%, p =0.02*) (Table 1). There were no statistically significant differences between continuous scores of parent stress, anxiety symptoms, and parenting skills between the pre- and post-App cohorts (Table 1). When scores for each outcome were categorized by severity, pre-App rollout parent experience data suggested that many of surveyed parents felt ill-prepared for discharge (36%), reported severe symptoms of stress (28%) and anxiety (40%), and were not confident in their parenting skills (8%). Post-App survey results indicated that a more parents reported optimal experiences of discharge readiness (56%), anxiety symptoms (44%), and parenting skills (25%) (Figure 1 and Table 1).Conclusion(s): Technology applications can improve maternal NICU experiences particularly during the COVID-19 pandemic.
Figure 1: Distribution of Survey Scores Among n = 50 parents by pre- and post- App rollout status
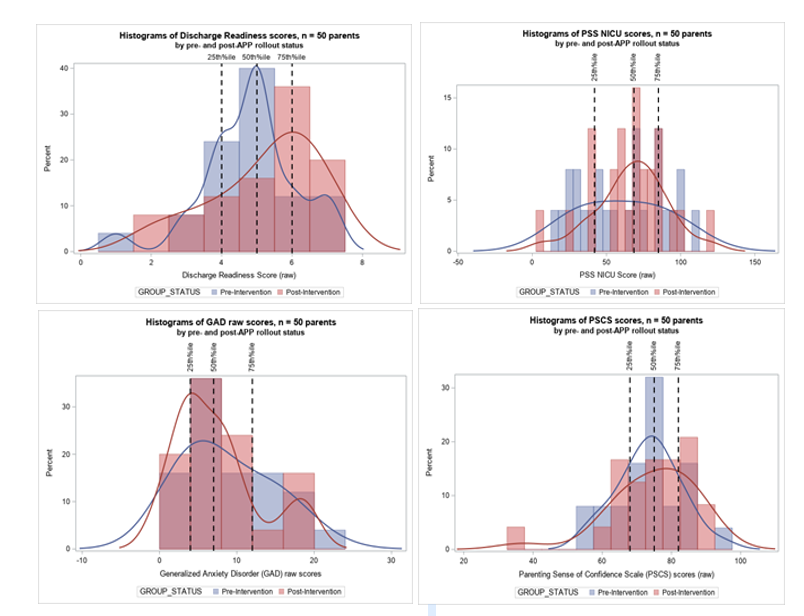
Table 1: Clinical and Demographic Characteristics for Pre- and Post-Intervention Cohorts of Infants and Parents. (n=50)