Neonatal Fetal Nutrition & Metabolism
Category: Abstract Submission
Neonatal Fetal Nutrition & Metabolism II
283 - Arachidonic acid metabolism and markers of poor fetal wellbeing in human fetal growth restricted pregnancies
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 283
Publication Number: 283.120
Publication Number: 283.120
Stephanie S. Chassen, University of Colorado Anschutz Medical Campus, Aurora, CO, United States; Karin A. Zemski Berry, University of Colorado School of Medicine, Aurora, CO, United States; Stefanie L. Raymond-Whish, University of Colorado Anschutz Medical Campus, Aurora, CO, United States; Camille Driver, University of Colorado School of Medicine, Denver, CO, United States; John C. Hobbins, University of Colorado School of Medicine, Denver, CO, United States; Theresa Powell, University of Colorado, Aurora, CO, United States

Stephanie S. Chassen, MD
Assistant Professor of Pediatrics
University of Colorado Neonatology
Aurora, Colorado, United States
Presenting Author(s)
Background: Arachidonic acid (AA) is a precursor to bioactive lipid molecules (eicosanoids) that influence inflammation and vasoregulation. Inflammation adversely affects fetal growth, and fetal growth restricted (FGR) infants have increased risk of perinatal mortality and lifelong metabolic disease. Umbilical artery (UA) and fetal middle cerebral artery (MCA) pulsatility index (PI) measurements by Doppler ultrasound (US) are used for surveillance of fetal compromise in FGR. Mechanisms of fetoplacental lipid transport and metabolism, and effects on fetal growth and wellbeing in FGR are poorly understood.
Objective: We hypothesized that AA and eicosanoid concentrations are increased in human FGR placentas and umbilical vein plasma, and correlate with US markers of fetal compromise (low MCA and high UA PI).
Design/Methods: Pregnant women with an estimated fetal weight (EFW) < 10% for gestation in the 2nd/3rd trimester were included. Growth and/or Doppler US (UA/MCA PI) was obtained every 1-4 weeks from enrollment. Birth weight (BW) was used to classify infants as FGR (BW < 5%), small for gestational age (BW 5-10%, SGA), or appropriate for gestational age (BW 10-90%, AGA). At delivery umbilical cord blood and placental tissue were collected. Targeted lipidomic analyses were performed by GCMS (free fatty acids) or LCMS [phosphatidyl-choline (PC), eicosanoids]. Statistical differences and correlations were assessed by student's t test and Pearson's coefficient.
Results: Birth weight was 25% smaller (p=0.004) and UA PI 22% higher (p=0.02) in the FGR group (n=8) compared to combined AGA/SGA group (n=12). Lower placenta concentrations of PC containing AA directly correlated with lower MCA PI (r=0.5, p< 0.05). Cord plasma concentrations of AA (+69%, p< 0.05), three PC containing AA (Fig 1- 16:1/20:4, 18:0e/20:4, 18:1e/20:4), and several AA-derived eicosanoid molecules (Fig 2- 5hete, 12hete, 5,6EET, 8,9EET, 11,12EET) were significantly increased in FGR. There was an inverse correlation between 5,6EET levels and BW, and a direct correlation of 5,6EET and 8,9EET concentrations with UA PI (Fig 3).Conclusion(s): AA (both PC and free) and several eicosanoid derivatives are increased in FGR cord plasma and correlate with markers of poor fetal wellbeing. We speculate that the hypoxemic placenta and fetus in FGR triggers eicosanoid production. Likely this disturbs the balance of pro/anti-inflammation and vasoconstriction/relaxation required for adequate fetal growth and wellbeing in utero.
Cord plasma PCs containing arachidonic acid (20:4) are increased in FGR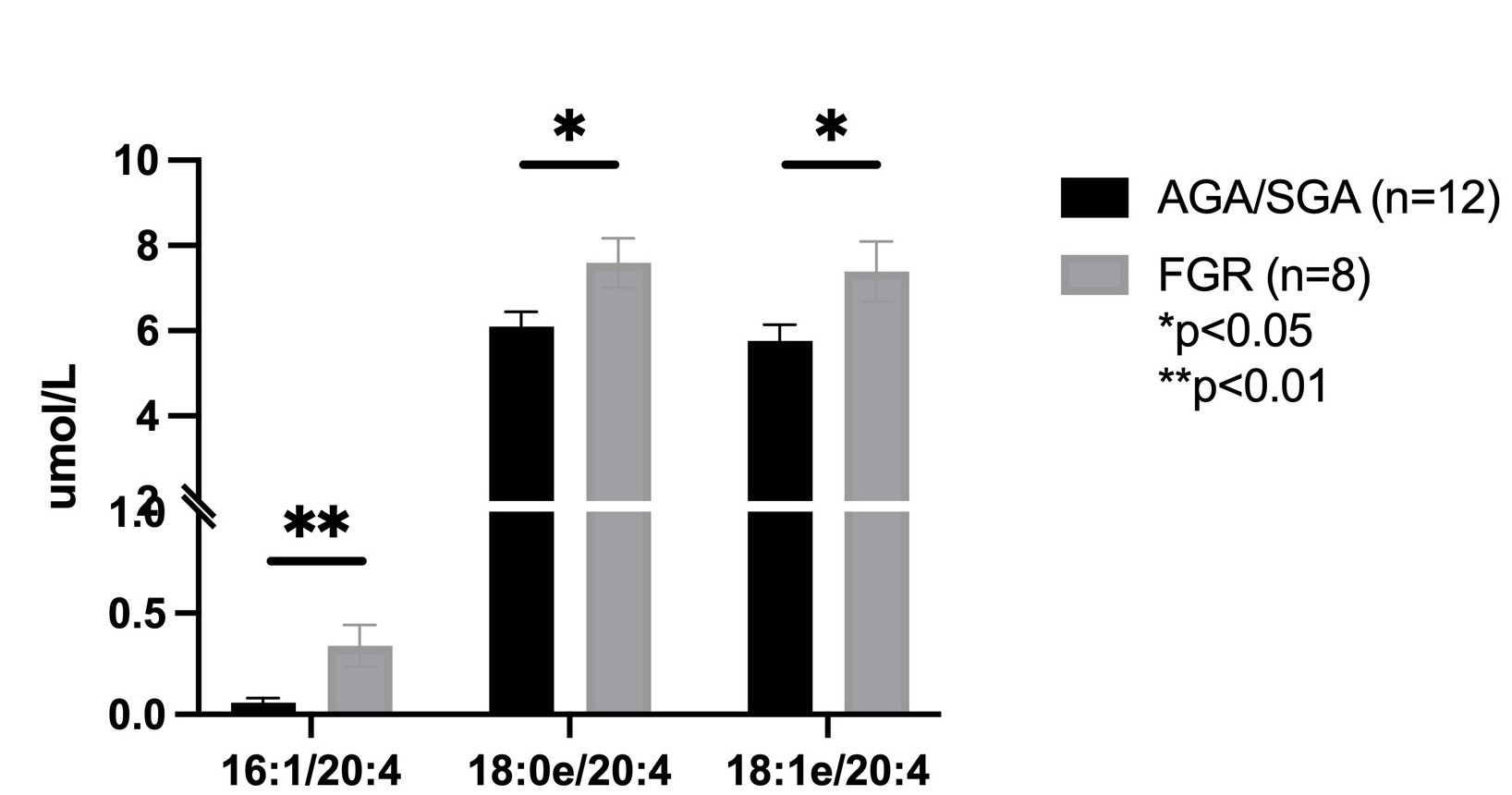 Graph depicting significantly increased concentrations (umol/L) of the phosphatidylcholine (PC) molecules containing 20:4 (arachidonic acid) in cord plasma from fetal growth restricted (FGR) pregnancies.
Graph depicting significantly increased concentrations (umol/L) of the phosphatidylcholine (PC) molecules containing 20:4 (arachidonic acid) in cord plasma from fetal growth restricted (FGR) pregnancies.
Cord plasma eicosanoids are increased in FGR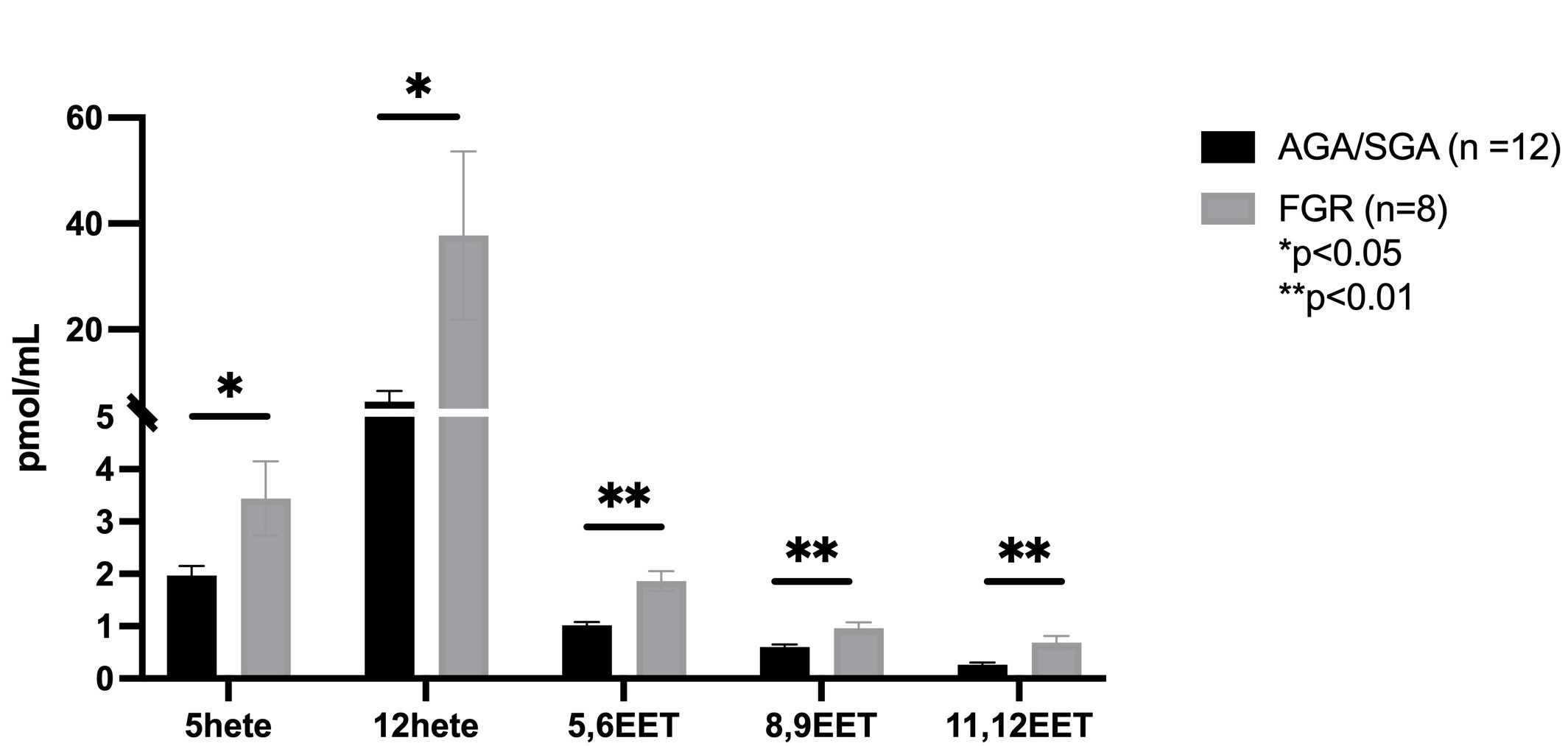 Graph depicting significantly increased concentrations (pmol/mL) of several eicosanoid molecules (epoxyeicosatrienoic acids, EETs; hydroxyeicosatetraenoic acids, Hetes) in cord plasma from fetal growth restricted (FGR) pregnancies.
Graph depicting significantly increased concentrations (pmol/mL) of several eicosanoid molecules (epoxyeicosatrienoic acids, EETs; hydroxyeicosatetraenoic acids, Hetes) in cord plasma from fetal growth restricted (FGR) pregnancies.
Objective: We hypothesized that AA and eicosanoid concentrations are increased in human FGR placentas and umbilical vein plasma, and correlate with US markers of fetal compromise (low MCA and high UA PI).
Design/Methods: Pregnant women with an estimated fetal weight (EFW) < 10% for gestation in the 2nd/3rd trimester were included. Growth and/or Doppler US (UA/MCA PI) was obtained every 1-4 weeks from enrollment. Birth weight (BW) was used to classify infants as FGR (BW < 5%), small for gestational age (BW 5-10%, SGA), or appropriate for gestational age (BW 10-90%, AGA). At delivery umbilical cord blood and placental tissue were collected. Targeted lipidomic analyses were performed by GCMS (free fatty acids) or LCMS [phosphatidyl-choline (PC), eicosanoids]. Statistical differences and correlations were assessed by student's t test and Pearson's coefficient.
Results: Birth weight was 25% smaller (p=0.004) and UA PI 22% higher (p=0.02) in the FGR group (n=8) compared to combined AGA/SGA group (n=12). Lower placenta concentrations of PC containing AA directly correlated with lower MCA PI (r=0.5, p< 0.05). Cord plasma concentrations of AA (+69%, p< 0.05), three PC containing AA (Fig 1- 16:1/20:4, 18:0e/20:4, 18:1e/20:4), and several AA-derived eicosanoid molecules (Fig 2- 5hete, 12hete, 5,6EET, 8,9EET, 11,12EET) were significantly increased in FGR. There was an inverse correlation between 5,6EET levels and BW, and a direct correlation of 5,6EET and 8,9EET concentrations with UA PI (Fig 3).Conclusion(s): AA (both PC and free) and several eicosanoid derivatives are increased in FGR cord plasma and correlate with markers of poor fetal wellbeing. We speculate that the hypoxemic placenta and fetus in FGR triggers eicosanoid production. Likely this disturbs the balance of pro/anti-inflammation and vasoconstriction/relaxation required for adequate fetal growth and wellbeing in utero.
Cord plasma PCs containing arachidonic acid (20:4) are increased in FGR
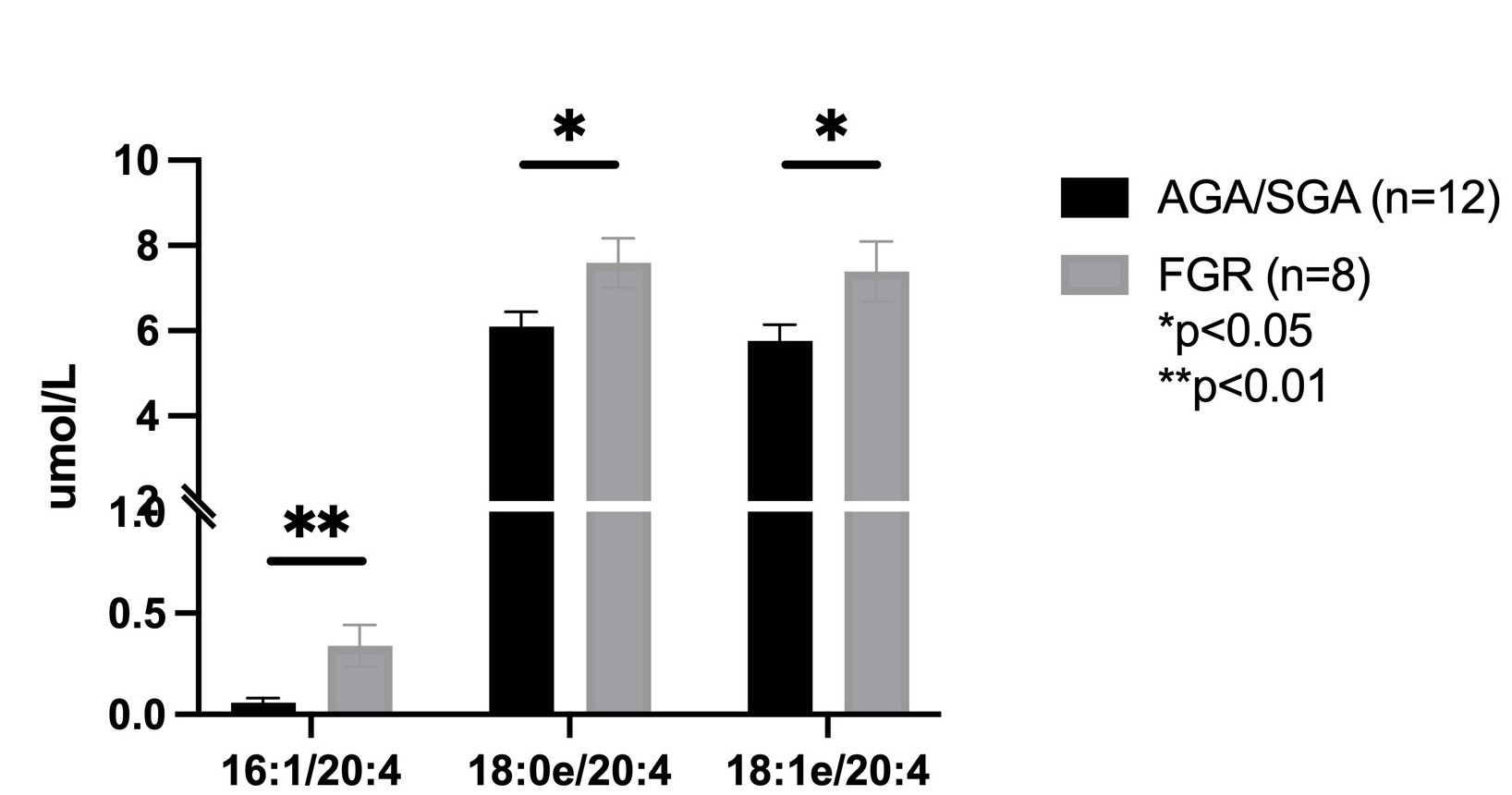 Graph depicting significantly increased concentrations (umol/L) of the phosphatidylcholine (PC) molecules containing 20:4 (arachidonic acid) in cord plasma from fetal growth restricted (FGR) pregnancies.
Graph depicting significantly increased concentrations (umol/L) of the phosphatidylcholine (PC) molecules containing 20:4 (arachidonic acid) in cord plasma from fetal growth restricted (FGR) pregnancies.Cord plasma eicosanoids are increased in FGR
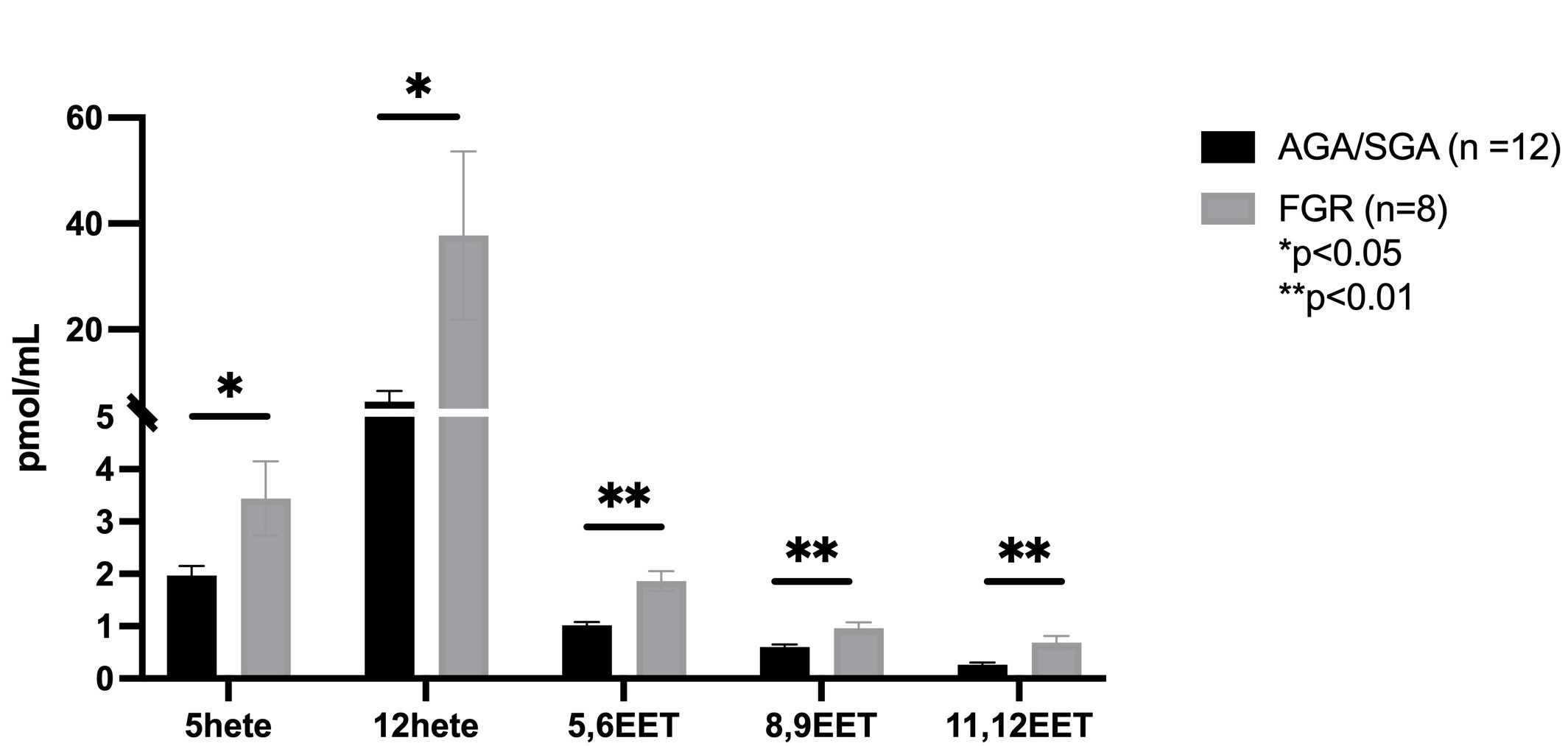 Graph depicting significantly increased concentrations (pmol/mL) of several eicosanoid molecules (epoxyeicosatrienoic acids, EETs; hydroxyeicosatetraenoic acids, Hetes) in cord plasma from fetal growth restricted (FGR) pregnancies.
Graph depicting significantly increased concentrations (pmol/mL) of several eicosanoid molecules (epoxyeicosatrienoic acids, EETs; hydroxyeicosatetraenoic acids, Hetes) in cord plasma from fetal growth restricted (FGR) pregnancies.